Chapter: Medical Surgical Nursing: Assessment and Management of Patients With Eye and Vision Disorders
Cataracts
Cataracts
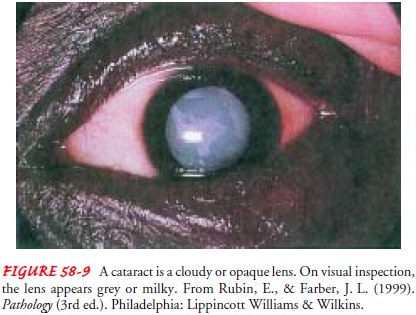
cataract
is a lens opacity or cloudiness (Fig. 58-9). Cataracts rank only behind
arthritis and heart disease as a leading cause of disability in older adults.
Cataracts affect nearly 20.5 million Americans who are 40 years of age or
older, or about one in every six people in this age range. By age 80, more than
half of all Amer-icans have cataracts. According to the World Health
Organization, cataract is the leading cause of blindness in the world (Preshel
& Prevent Blindness America, 2002).
Pathophysiology
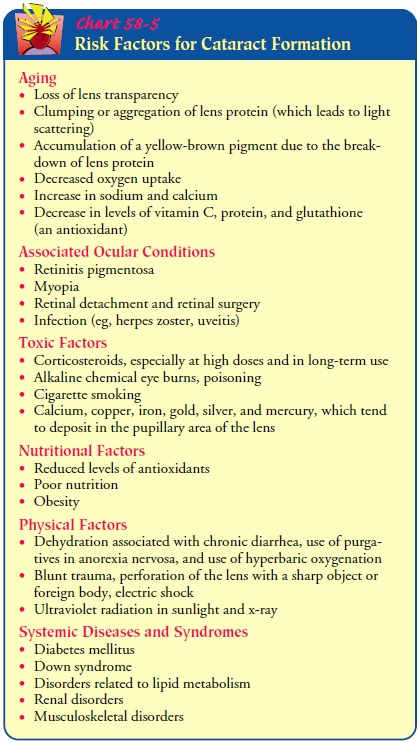
Cataracts
can develop in one or both eyes at any age for a variety of causes (Chart
58-5). Visual impairment normally progresses at the same rate in both eyes over
many years or in a matter of months. The three most common types of senile
(age-related) cataracts are defined by their location in the lens: nuclear,
cortical, and posterior subcapsular. The extent of visual impairment de-pends
on the size, density, and location in the lens. More than one type can be
present in one eye.
A
nuclear cataract is associated with myopia (ie, nearsighted-ness), which
worsens when the cataract progresses. If dense, the cataract severely blurs
vision. Periodic changes in prescription eyeglasses help manage this problem.
A cortical cataract involves the anterior,
posterior, or equato-rial cortex of the lens. A cataract in the equator or
periphery of the cortex does not interfere with the passage of light through
the center of the lens and has little effect on vision. Cortical cataracts
progress at a highly variable rate. Vision is worse in very bright light.
Studies show that people with the highest levels of sun-light exposure have
twice the risk of developing cortical cataracts than those with low-level
sunlight exposure (West et al., 1998).
Posterior subcapsular cataracts occur in front of the posterior capsule. This type typically develops in younger people and, in some cases, is associated with prolonged corticosteroid use, in-flammation, or trauma. Near vision is diminished, and the eye is increasingly sensitive to glare from bright light (eg, sunlight, headlights).
Clinical Manifestations
Painless,
blurry vision is characteristic of cataracts. The patient perceives that
surroundings are dimmer, as if glasses need clean-ing. Light scattering is
common, and the individual experiences reduced contrast sensitivity,
sensitivity to glare, and reduced vi-sual acuity. Other effects include myopic
shift, astigmatism, monocular diplopia
(ie, double vision), color shift (ie, the aging lens becomes progressively more
absorbent at the blue end of the spectrum), brunescens (ie, color values shift
to yellow-brown), and reduced light transmission.
Assessment and Diagnostic Findings
Decreased visual acuity is directly proportionate
to cataract den-sity. The Snellen visual acuity test, ophthalmoscopy, and
slit-lamp biomicroscopic examination are used to establish the degree of
cataract formation. The degree of lens opacity does not always correlate with
the patient’s functional status. Some patients can perform normal activities
despite clinically significant cataracts. Others with less lens opacification
have a disproportionate decrease in visual acuity; hence, visual acuity is an
imperfect mea-sure of visual impairment.
Medical Management
No nonsurgical treatment cures cataracts. Ongoing
studies are in-vestigating ways to slow cataract progression, such as intake of
antioxidants (eg, vitamin C, beta-carotene, vitamin E) (Age-Related Eye Disease
Research Study Group, 2001). In the early stages of cataract development,
glasses, contact lenses, strong bifocals, or magnifying lenses may improve
vision. Reducing glare with proper light and appropriate lighting can
facilitate reading. Mydriatics can be used as short-term treatment to dilate
the pupil and allow more light to reach the retina, although this increases
glare.
SURGICAL MANAGEMENT
Fewer than 15% of people with cataracts suffer
vision problems severe enough to require surgery. In general, if reduced vision
from cataract does not interfere with normal activities, surgery may not be
needed. However, in deciding when cataract surgery is to be performed, the
patient’s functional and visual status should be a primary consideration.
Surgery is performed on an outpatient basis and usually takes less than 1 hour,
with the patient being dis-charged in 30 minutes or less afterward. Although
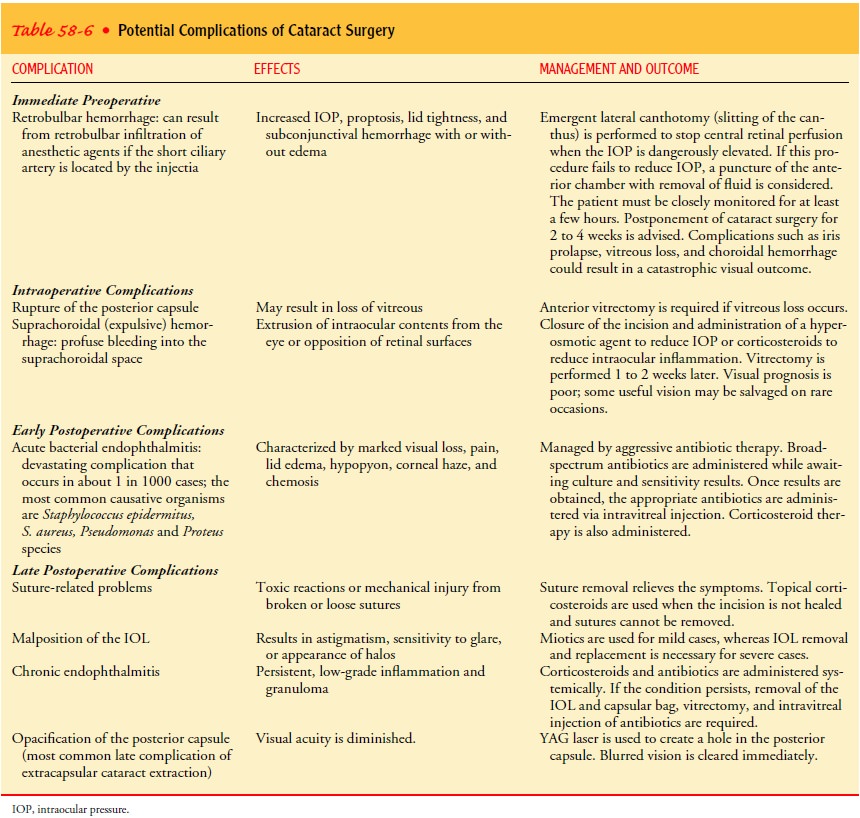
complications from cataract surgery are uncommon, they can have significant
effects on vision (Table 58-6). Restoration of visual function through a safe
and minimally invasive procedure is the surgical goal, which is achieved with
advances in topical anesthesia, smaller wound incision (ie, clear cornea
incision), and lens design (ie, foldable and more accurate intraocular lens
measurements).
Topical anesthesia, such as lidocaine gel applied
to the surface of the eye, eliminates the hazards of regional anesthesia, such
as oc-ular perforation, retrobulbar hemorrhage, optic injuries, diplopia, and
ptosis, and is ideal for patients receiving anticoagulants. More-over, patients
can communicate and cooperate during surgery.
When
both eyes have cataracts, one eye is treated first, with at least several
weeks, preferably months, separating the two opera-tions. Because cataract
surgery is performed to improve visual functioning, the delay for the other eye
gives time for the patient and the surgeon to evaluate whether the results from
the first surgery are adequate enough to preclude the need for a second
operation. The delay also provides time for the first eye to recover; if there
are any complications, the surgeon may decide to perform the second procedure
differently.
Intracapsular Cataract Extraction.
From the late 1800s
until the1970s, the technique of choice for cataract extraction was
intra-capsular cataract extraction (ICCE). The entire lens (ie, nucleus,
cortex, and capsule) is removed, and fine sutures close the inci-sion. ICCE is
infrequently performed today; however, it is indi-cated when there is a need to
remove the entire lens, such as with a subluxated cataract (ie, partially or
completely dislocated lens).
Extracapsular Surgery.
Extracapsular cataract extraction (ECCE)achieves the intactness of smaller incisional wounds (less trauma to the eye) and maintenance of the posterior capsule of the lens, reducing postoperative complications, particularly aphakic reti-nal detachment and cystoid macular edema. In ECCE, a portion of the anterior capsule is removed, allowing extraction of the lens nucleus and cortex. The posterior capsule and zonular support are left intact. An intact zonular-capsular diaphragm provides the needed safe anchor for the posterior chamber intraocular lens (IOL). After the pupil has been dilated and the surgeon has made a small incision on the upper edge of the cornea, a viscoelastic substance (clear gel) is injected into the space between the cornea and the lens. This prevents the space from collapsing and facili-tates insertion of the IOL.
Phacoemulsification.
This method of extracapsular surgery usesan ultrasonic device that
liquefies the nucleus and cortex, which are then suctioned out through a tube.
The posterior capsule is left intact. Because the incision is even smaller than
the standard ECCE, the wound heals more rapidly, and there is early
stabi-lization of refractive error and less astigmatism. Hardware and software
advances in ultrasonic technology—including new phaco needles that are used to
cut and aspirate the cataract— permit safe and efficient removal of nearly all
cataracts through a clear cornea incision that is as small or smaller than
required for available foldable lenses. Ultimately, advances in technology will
achieve an injectable IOL.
Lens Replacement.
After removal of the crystalline lens, the pa-tient is referred to as aphakic (ie, without lens). The lens,
which focuses light on the retina, must be replaced for the patient to see
clearly. There are three lens replacement options: aphakic eye-glasses, contact
lenses, and IOL implants.
Aphakic glasses are effective but heavy. Objects
are magnified by 25%, making them appear closer than they actually are.
Ob-jects are magnified unequally, creating distortion. Peripheral vi-sion is
also limited, and binocular vision
(ie, ability of both eyes to focus on one object and fuse the two images into
one) is im-possible if the other eye is phakic (normal).
Contact lenses provide patients with almost normal
vision, but because contact lenses need to be removed occasionally, the patient
also needs a pair of aphakic glasses. Contact lenses are not advised for
patients who have difficulty inserting, removing, and cleaning them. Frequent
handling and improper disinfection increase the risk for infection.
Insertion of IOLs during cataract surgery is the
usual approach to lens replacement. After ICCE, the surgeon implants an
anterior chamber IOL in front of the iris. Posterior chamber lenses, gener-ally
used in ECCE, are implanted behind the iris. ECCE and pos-terior chamber IOLs
are associated with a relatively low incidence of complications (eg, hyphema,
macular edema, secondary glau-coma, damage to the corneal endothelium). IOL
implantation is contraindicated in patients with recurrent uveitis,
proliferative di-abetic retinopathy, neovascular glaucoma, or rubeosis iridis.
Like any device, IOLs can malfunction and cause complications.
Nursing Management
The patient with cataracts should receive the usual
preoperative care for ambulatory surgical patients undergoing eye surgery.
According to the study on Medical Testing for Cataract Surgery, routine
preoperative testing before cataract surgery does not im-prove health or
clinical outcomes. Hence, the standard battery of preoperative tests should be
prescribed only when they would have been indicated by the patient’s medical
history (Schein et al., 2000).
PROVIDING PREOPERATIVE CARE
To
reduce the risk for retrobulbar hemorrhage (after retrobulbar injection), any
anticoagulation therapy that the patient is receiv-ing is withheld, if
medically appropriate. Aspirin should be with-held for 5 to 7 days,
nonsteroidal anti-inflammatory medications (NSAIDs) for 3 to 5 days, and
warfarin (Coumadin) until the prothrombin time of 1.5 is almost reached.
Dilating
drops are administered every 10 minutes for four doses at least 1 hour before
surgery. Additional dilating drops may be administered in the operating room
(immediately before surgery) if the affected eye is not fully dilated.
Antibiotic, corti-costeroid, and NSAID drops may be administered
prophylacti-cally to prevent postoperative infection and inflammation.
PROVIDING POSTOPERATIVE CARE
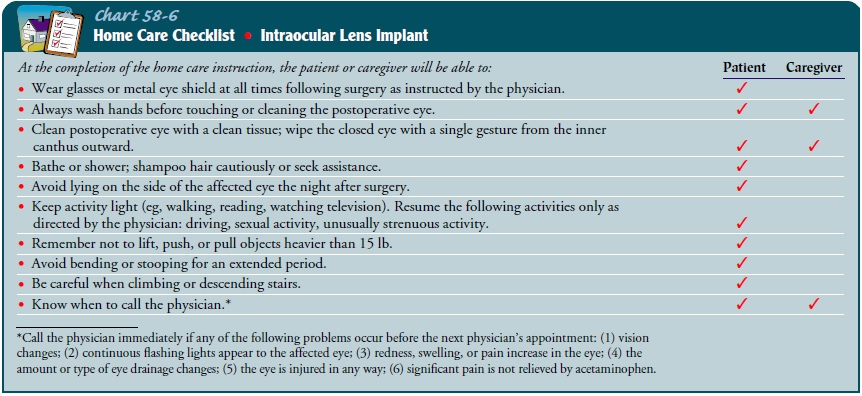
After recovery from anesthesia, the patient
receives verbal and writ-ten instruction regarding how to protect the eye,
administer med-ications, recognize signs of complications, and obtain emergency
care. Activities to be avoided are identified in Chart 58-6. The nurse also
explains that there is minimal discomfort after surgery and instructs the
patient to take a mild analgesic agent, such as aceta-minophen, as needed.
Antibiotic, anti-inflammatory, and cortico-steroid eye drops or ointments are
prescribed postoperatively.
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care.
To prevent accidental rubbing orpoking of the eye,
the patient wears a protective eye patch for 24 hours after surgery, followed
by eyeglasses worn during the day and a metal shield worn at night for 1 to 4
weeks. The nurse in-structs the patient and family in applying and caring for
the eye shield. Sunglasses should be worn while outdoors during the day because
the eye is sensitive to light.
Slight morning discharge, some redness, and a
scratchy feeling may be expected for a few days. A clean, damp washcloth may be
used to remove slight morning eye discharge. Because cataract surgery increases
the risk for retinal detachment, the patient must know to notify the surgeon if
new floaters (ie, dots) in vision, flash-ing lights, decrease in vision, pain,
or increase in redness occurs.
Continuing Care.
The eye patch is removed after the first follow-up appointment. Patients
may experience blurring of vision for several days to weeks. Sutures left in
the eye alter the curvature of the cornea, resulting in temporary blurring and
some astigma-tism. Vision gradually improves as the eye heals. Patients with
IOL implants have visual improvement faster than those waiting for aphakic
glasses or contact lenses. Vision is stabilized when the eye is completely
healed, usually within 6 to 12 weeks, when final corrective prescription is
completed. Visual correction is needed for any remaining nearsightedness or
farsightedness (even in pa-tients with IOL implants).
Related Topics