Chapter: Biology of Disease: Disorders of the Endocrine System
Reproductive Hormones
REPRODUCTIVE HORMONES
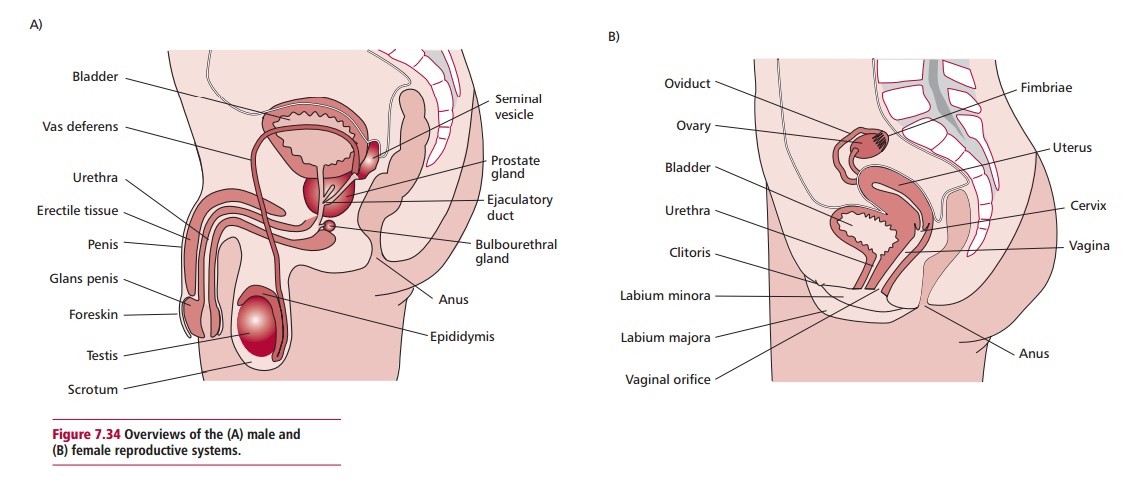
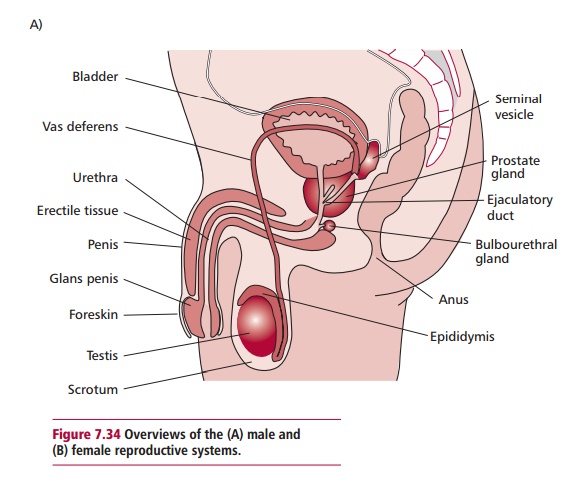
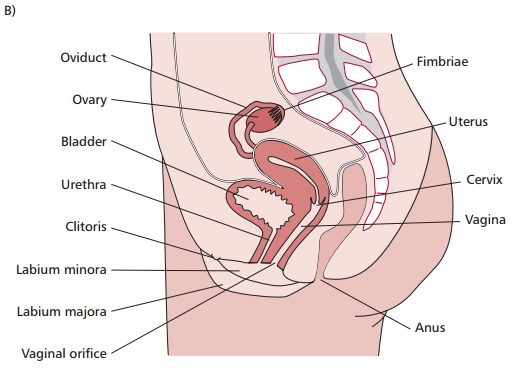
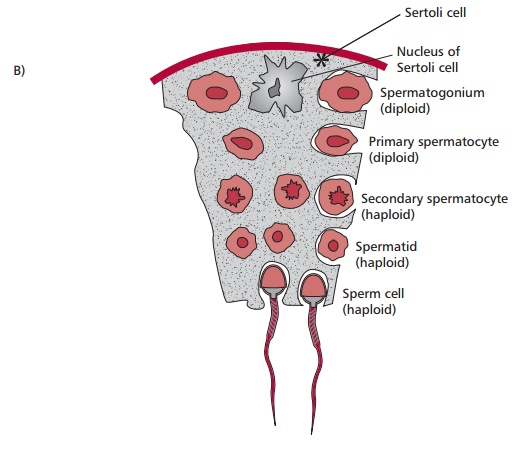
The male and female reproductive systems (Figure 7.34 (A) and (B)) produce and secrete a number of sex hormones and are
responsible for the maturation of germ cells, the production of gametes and, in
the female, the fertilization of the ovum and its subsequent growth and
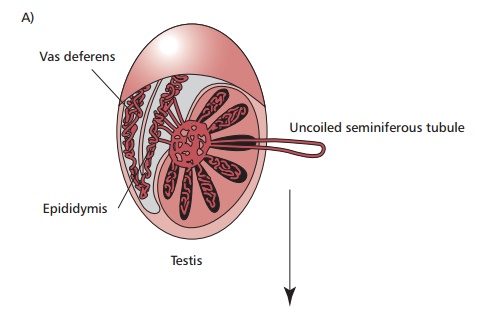
development. The testes produce male gametes or spermatozoa (ŌĆśspermsŌĆÖ) that
mature and are stored in the epididymis and vas deferens. Testes are composed
of lobules with up to three seminiferous tubules containing cells undergoing
spermatogenesis. These cells are supported and nourished by Sertoli cells.
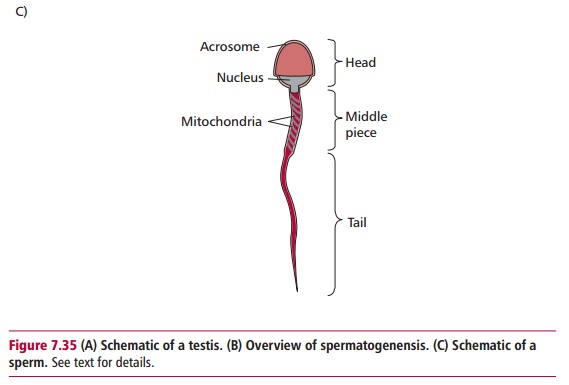
Spermatogenesis involves meiosis and produces haploid sperm as outlined in Figure 7.35. Each sperm has a head and a
tail consisting of a midpiece andflagellum. The midpiece contains mitochondria
that provide energy for the locomotory movements of the flagellum. The head
contains a nucleus and
is covered by a cap called an acrosome, which
contains enzymes required to penetrate the ovum or egg. The production of ova,
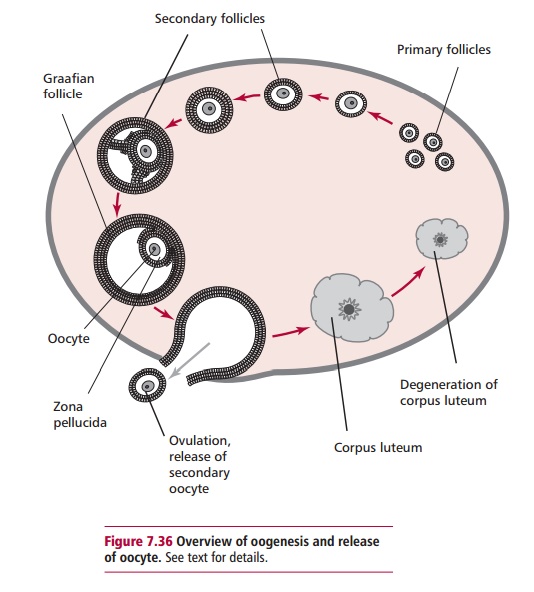
female gametes, begins in the ovaries by a process called oogenesis (Figure 7.36). Primordial germ cells in
the outer germinal epithelium divide by mitosis to form a diploid primary
oocyte that becomes surrounded by follicle cells to produce primary follicles.
These migrate into the center of the ovary. As many as two million primary
follicles are present at birth and remain dormant until puberty. Approximately
400 primary follicles mature over the lifetime of a female until follicle
development ceases at the menopause. The primary follicle matures to form a
secondary follicle. During this development, the primary oocyte divides by
meiosis but this is arrested and forms a haploid secondary oocyte, which is the
precursor of the ovum, and a small polar body. In an adult fertile female, the
nucleus of a secondary oocyte begins the second meiotic division at each
monthly ovulation but progresses only to metaphase, when
In males and females, the hypothalamus secretes
gonadotrophin releasing hormone (GnRH) which regulates secretion of LH and FSH
from the basophil cells of the anterior pituitary. Secretion of GnRH, LH and
FSH occurs in pulses. Follicle stimulating hormone and LH act cooperatively to
stimulate the ovaries and testes to secrete sex hormones and to develop germ
cells.
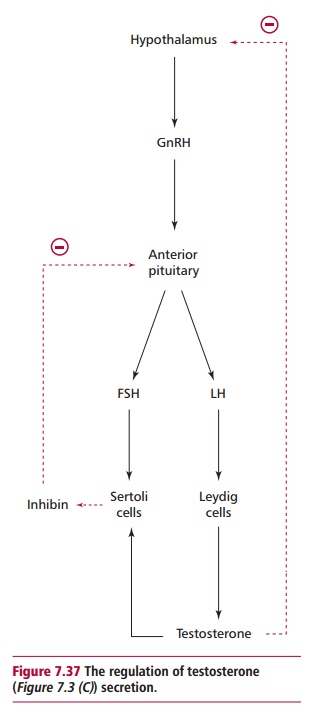
The testes are stimulated by LH to release
testosterone from their Leydig cells (Figure
7.37). Testosterone is the principal androgen and its secretion inhibits
further release of LH by a negative feedback mechanism. Follicle stimulating
hormone and testosterone are required by Sertoli cells in the basement membrane
of the seminiferous tubules to produce inhibin that, in turn, inhibits the
secretion of FSH by negative feedback (Figure
7.37). Testosterone is also required for sexual differentiation, the
development of secondary sexual characteristics and spermatogenesis. It is
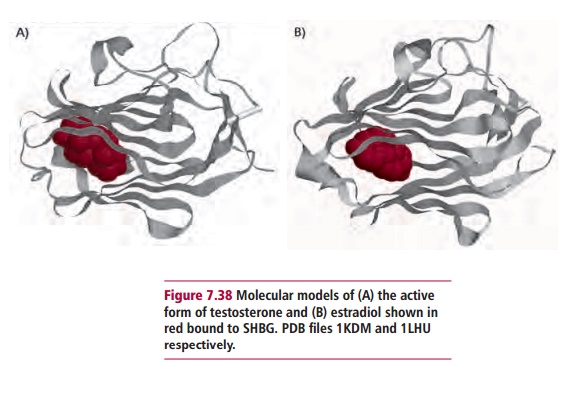
transported in the blood, bound to sex hormone binding globulin, SHBG (Figure 7.38 (A)) and to a lesser extent
albumin. Typically, only its free fraction is metabolically active.
Testosterone enters target cells and is converted to the potent androgen,
dihydrotestosterone by the enzyme 5@-reductase. Testosterone is also
found in the plasma of normal females, half of which is secreted by the
ovaries, the remainder arising from the peripheral conversion of
androstenedione and DHEAS, both of which are secreted by the adrenal cortex.
The ovaries produce estrogens, of which estradiol is
required for the develop-ment of female secondary sexual characteristics and
normal menstruation. Circulating estradiol is bound mostly to SHBG (Figure 7.38 (B) ), although the blood
concentration of estradiol varies widely with the menstrual cycle.
The plasma concentration of estradiol is low before
puberty but increases rapidly and fluctuates during the menstrual cycle, a
series of cyclical changes in the ovary, uterus and pituitary that occur
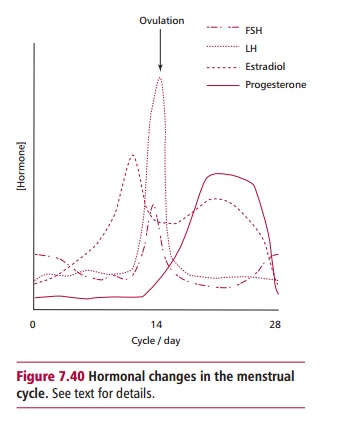
approximately every 28 days until the menopause. Variations in plasma hormones
in the menstrual cycle (Figure7.40)
depend on interactions between the hypothalamus, anterior pituitaryand ovaries.
Follicle stimulating hormone is released at the beginning of the cycle and
increases growth of the follicles in the ovaries. Estradiol production
increases the sensitivity of the pituitary to GnRH but decreases its secretion
by the hypothalamus. The release of estradiol gradually increases and a
follicle matures during the first half of the cycle. At the start of each
cycle, about 20 secondary follicles enlarge and begin to secrete estrogen and
the hormone inhibin, and a cavity filled with follicular fluid forms around
their ova. This is referred to as antrum formation. By about the sixth day, one
of the secondary follicles in an ovary has outgrown the others and becomes the
dominant follicle. Its secretion of estrogen and inhibin decreases the
secretion of FSH (Figures 7.36 and 7.40), leading to the regression of the
other follicles in an apoptotic process to form atretic follicles. It is
uncertain how only the one follicle becomes dominant, but appears to be related
to its ability to secrete the estrogen, needed for its maturation under the
influence of LH. Maturation involves the dominant secondary follicle accumulating
fluid filled cavities that eventually enlarge to the point where they are
called a Graafian follicle. Ovulation occurs each month when a Graafian
follicle ruptures to release the oocyte, now usually called an ovum, into the
Fallopian tube. The ovum is transported along the tube by ciliary action. The
portion of the follicle remaining in the ovary develops into a corpus luteum.
If fertilization does not occur, this degenerates within 10 days or so.
Following copulation, the sperm are propelled through
the vas deferens by muscular contractions into the urethra. The sperm are
suspended in liquid semen produced by the seminal vesicles, prostate and
bulbourethral glands. Semen contains nutrients, which activates and increases
the motility of sperm, and is alkaline to counteract the acidity of the vagina.
The ruptured follicle develops into the corpus luteum, which secretes
progesterone and estradiol and stimulates the development of the endometrium
for implantation. Fertilization of the egg to form a zygote usually takes place
in the Fallopian tubes and the developing embryo is transported to the uterus
by ciliary action and muscular contractions. The zygote begins a series of
mitotic divisions to form a developing embryo that embeds into the endometrium
lining the uterus and undergoes further development to produce a fetus and
eventually a neonate in 9 months. Fertilization ensures that the corpus luteum
does not degenerate but begins to produce a number of sex hormones, together
with those produced by the gonads and anterior pituitary. Following the
menopause, plasma levels of estradiol decline despite the high levels of
gonadotrophins and ovulation ceases.
Related Topics