Chapter: Biology of Disease: Disorders of the Endocrine System
Hypoglycemia - Regulation of Blood Glucose
HYPOGLYCEMIA
Hypoglycemia is defined as a blood glucose concentration less than 2.2 mmol dm–3 in a random specimen collected into a tube containing an inhibitor of glycolysis. Hypoglycemia occurs because of an imbalance between glucose intake, endogenous glucose production and glucose
Its clinical features are mainly due to abnormal function of the CNS (neuroglycopenia) and can be acute or chronic. Acute features include tiredness, confusion, hunger, dizziness, blurred vision, convulsions, coma, anxiety, profuse sweating and tachycardia. The typical signs and symptoms are more likely to occur if blood glucose falls rapidly: in children and young adults the symptoms often present when the glucose concentration is less than 2.2 whereas neonates develop symptoms only when it is less than 1.5 mmol dm–3. Acute hypoglycemia is usually associated with diabetics who have taken too much insulin. Its chronic features include personality changes, memory loss and dementia and are generally observed in patients with insulin secreting tumors.
Most cases of hypoglycemia occur in patients with type 1 diabetes mellitus because of insufficient carbohydrate, too high a dose of insulin, inappropriate use of hypoglycemic drugs, excessive alcohol intake and strenuous exercise. Hypoglycemia can occur during fasting if the individual has an insulin secreting tumor or insulinoma which is a primary tumor of the β cells of the islets of Langerhans. These tumors produce excessive amounts of insulin or secrete insulin when it is not required. Nonpancreatic tumors, especially carcinomas of the liver and sarcomas, may cause hypoglycemia by increasing cellular uptake of glucose but this is unlikely to be the sole cause. Many of these tumors secrete IGF-II which has insulin-like effects and is capable of causing hypoglycemia.
Hypoglycemia in children is particularly dangerous because of the high risk of permanent brain damage. Its diagnosis is especially necessary in the first few months of life. A fetus exposed to maternal hyperglycemia will have pancreatic islet cell hyperplasia and elevated insulin levels. Following birth, the neonate has hyperinsulinism and may develop hypoglycemia now the high glucose supply from the mother has been removed. In addition, these babies are larger than average in size since insulin promotes growth.
Diagnosis and treatment of hypoglycemia
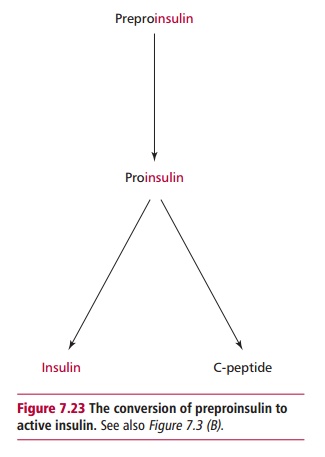
An initial assessment of a patient with frequent episodes of hypoglycemia involves a thorough clinical evaluation with an emphasis on the patient’s drug history, relationship of symptoms to meals, presence/history of endocrine disease and an investigation of a possible nonpancreatic tumor. Laboratory tests can confirm the diagnosis of hypoglycemia by demonstrating a low blood glucose concentration. To confirm that the clinical features are due to hypoglycemia, the patient can be given glucose by mouth or parenterally as appropriate. Symptoms that are due to acute neuroglycopenia resolve immediately whereas those due to chronic neuroglycopenia often persist. Measurement of plasma insulin concentration can help in the diagnosis or exclusion of an insulinoma. An insulinoma is likely if the patient has fasting hypoglycemia together with high serum insulin levels that are greater than 10 mU dm–3 and raised C-peptide levels (Figure 7.23). Insulin secretion in an insulin-treated diabetic cannot be determined for obvious reasons. However, insulin and the C-peptide are secreted by islet cells in equimolar amounts and therefore a measurement of C-peptide together with insulin can differentiate between hypoglycemia due to an insulinoma, which will have a high C-peptide concentration, from that due to exogenous insulin, which will have relatively low amounts of C-peptide.
Hypoglycemia can be fatal and patients must be treated urgently. The aim in comatose patients is to rapidly correct the hypoglycemia using intravenous dextrose or intramuscular glucagon. If a patient is conscious and can swallow, then they are given sweet drinks, sweets or glucose tablets. The underlying cause of hypoglycemia needs to be identified and rectified; an insulinoma, for example, requires surgical removal.
Related Topics