Chapter: Biology of Disease: Disorders of the Endocrine System
Diagnosis and Treatment of Thyroid Disorders
DIAGNOSIS AND TREATMENT OF THYROID DISORDERS
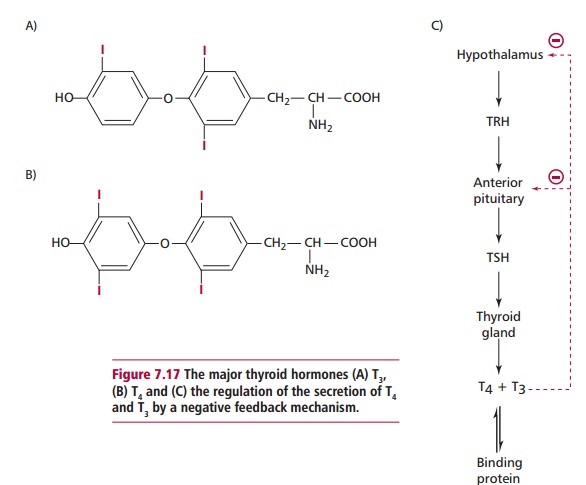
Investigating thyroid abnormalities involves measurements of serum TSH as a first line test for thyroid function. Some laboratories also include measurement of free T4 and/or free or total T 3 in their first line screen. Sensitive assays for measurement of TSH are readily available. Thyroid stimulating hormone levels are increased in primary hypothyroidism, normal in euthyroid individuals (those without thyroid disease) and low or undetectable in hyperthyroidism.
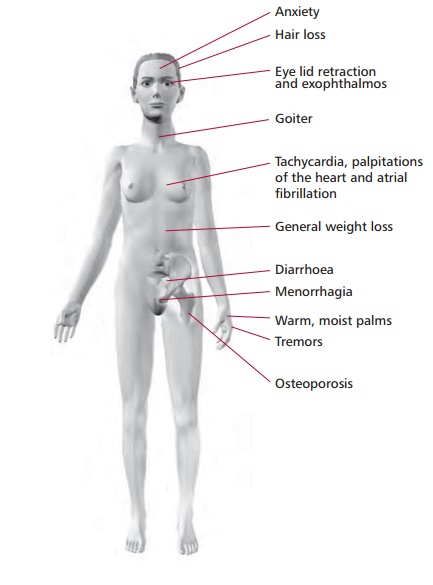
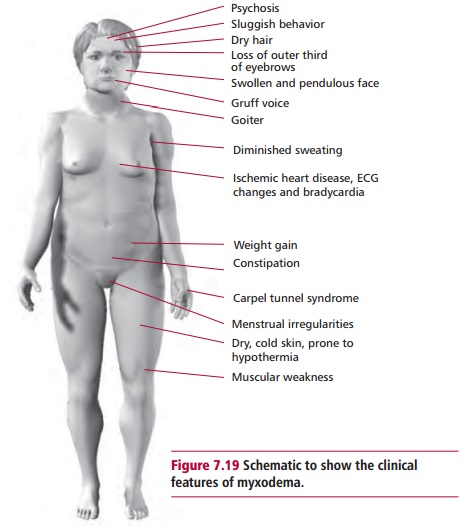
Total T4 and T3 measurements were once used widely in pathology laboratories but have the disadvantage that their values are dependent on plasma TBG levels, which can give misleading results. When TBG levels increase, for example in pregnancy or in females receiving estrogen-containing oral contraceptives, then total T4 and total T3 are also increased even though the individual is not hyperthyroid. Decreases in TBG concentrations occur in malnutrition, protein loss, severe illness and malabsorption and causes a reduction in total T4and T3. There has been some controversyon the validity of free thyroid hormone measurements, but most laboratories now determine free T4 and T3, rather than the total concentration. Free T4 and particularly free T3, are usually increased in hyperthyroidism. Free T4 is low in hypothyroidism and is the preferred measurement for its detection because free T3 can be normal in hypothyroidism due to an increase in its peripheral formation from T4. In a few patients with hyperthyroidism, free T4 is within the reference range but free T3 is increased and TSH is nearly always undetectable. This form of hyperthyroidism is referred to as T3 toxicosis.
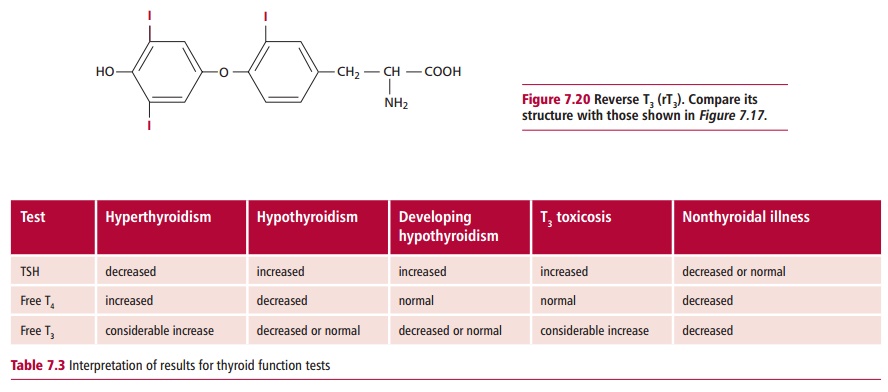
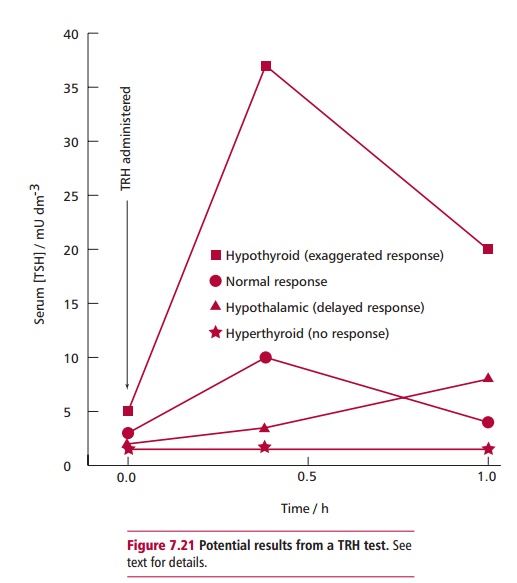
In any systemic illness, such as myocardial infarction, fever or liver disease, the normal metabolism of thyroid hormones is disturbed, reducing the concentrations of T4 and T3 in the plasma because T4 is converted to an inactive isomer called reverse T3 or rT3 (Figure 7.20) and T3 is not replenished from T4. Thyroid stimulating hormone levels may be normal or reduced and concentrations of TBG, albumin and prealbumin may also decline. Patients may have reduced T4, T3 and TSH, although there is no thyroid dysfunction. For this reason, thyroid function tests should not be performed on sick patients until they recover. Table 7.3 outlines the results of tests used in thyroid disorders. The TRH test is rarely used now in the diagnosis of thyroid disease. It is almost exclusively used in the diagnosis of patients with pituitary disease and to assess the capacity of the pituitary to secrete TSH. The patient is given 200 Mg of TRH intravenously and the serum TSH is measured after 0, 20 and 60 min. A normal response involves a three- to fivefold increase in TSH above the basal level. A slow rise in TSH (where the 60-min concentration is greater than the one at 20 min) together with low basal levels of TSH and thyroid hormones suggests hypothalamic disease, while a lack of response is suggestive of pituitary hypothyroidism or hyperthyroidism (Figure 7.21).
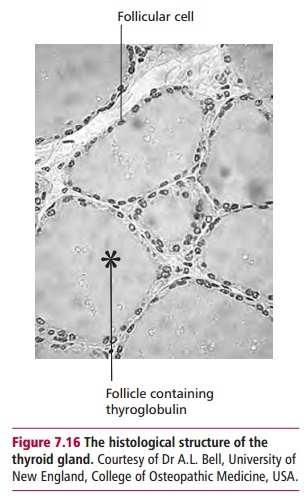
Other techniques for investigating thyroid function include administration of isotopes, such as 99mTc-pertechnetate, and determining their distribution using a camera that detects F radiation. This technique distinguishes between active and inactive thyroid nodules and can distinguish between Grave’s disease, multinodular goiter or an adenoma affecting the thyroid gland. A thyroid biopsy involves aspirating tissue from the affected region of the thyroid using a syringe and fine needle. The collected cells are examined microscopically for evidence of thyroid nodules. Often thyroid disease has an autoimmune basis and measurement of antibodies can aid diagnosis. Antiperoxidase and antithyroglobulin antibodies are found in patients affected by Hashimoto’s thyroiditis and often in those with Grave’s disease. However, the detection of antibodies is not always diagnostic, as low levels of these antibodies can occur in older people who are euthyroid.
The management of hyperthyroidism includes using antithyroid drugs, for example, carbimazole. This is useful in young patients and acts by reducing the production of thyroid hormones. Other forms of treatment include radioiodine therapy with 131I, although this is normally used in older patients, and partial or complete surgical removal of the thyroid gland (thyroidectomy). Some patients develop hypothyroidism, often as a consequence of treatment, and may have to be placed on thyroxine therapy. In this regard it is important to monitor TSH levels to detect developing hypothyroidism. Management of hypothyroidism involves replacement therapy with thyroxine, often for life. Thyroxine is readily available, safe and inexpensive. The treatment is monitored at regular intervals by measurement of serum concentrations of TSH to ensure they are kept within its reference range.
Related Topics