Chapter: Biology of Disease: Disorders of the Endocrine System
Regulation of Blood Glucose
REGULATION OF BLOOD GLUCOSE
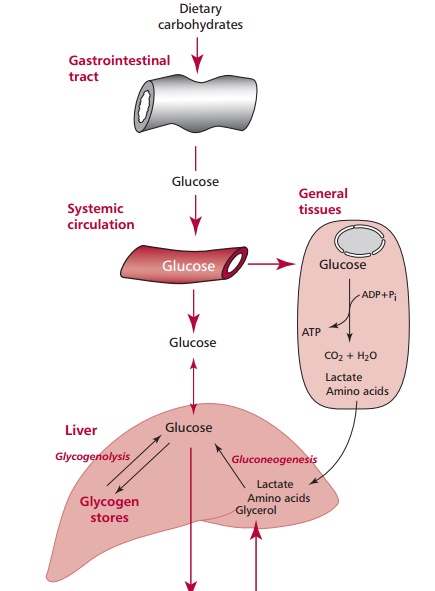
Adequate concentrations of glucose in the blood are necessary
for brain cells as they cannot metabolize substances other than glucose and
ketone bodies as energy sources nor can they store or synthesize glucose. After
a meal, any released glucose is absorbed by the gastrointestinal tract enters
the bloodstream and is delivered to the peripheral tissues where it may be metabolized
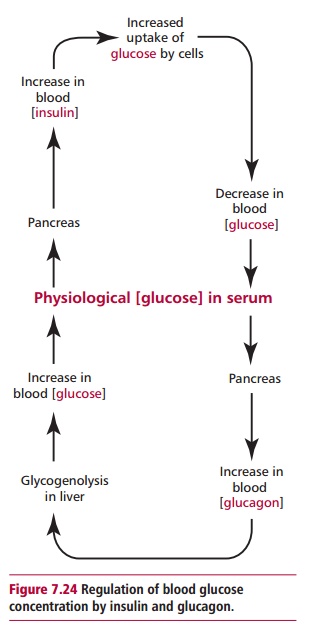
to allow ATP production. Surplus glucose is converted to glycogen and stored in
the liver and skeletal muscles or converted to triacylglycerols and stored in
adipose tissue. During fasting, the liver produces glucose by glycogenolysis or
gluconeogenesis and this is used to maintain blood glucose concentration (Figure 7.22).
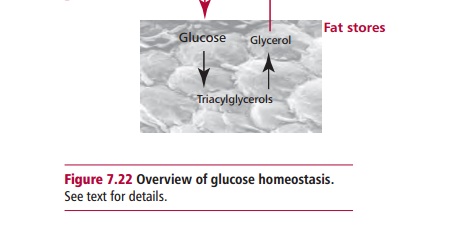
The concentration of glucose in plasma is regulated by the
hormones insulin and glucagon. Insulin is synthesized as preproinsulin in the β cells of the islets of Langerhans in the pancreas
but during its secretion is enzymatically converted to active insulin (Figures 7.3 (B) and 7.23). Insulin has a number of functions. It inhibits
glycogenolysis, gluconeogenesis, lipolysis, ketogenesis
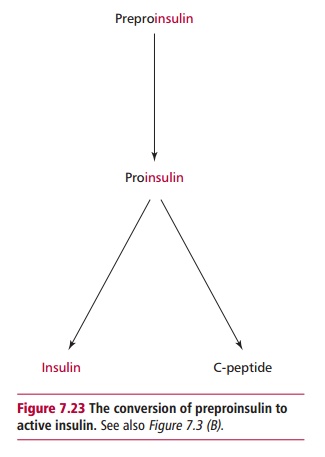
and proteolysis and stimulates glucose uptake by muscle and
adipose tissues, glycolysis, glycogenesis, protein synthesis and uptake of K+
and Pi. Glucagon is released by the α cells of the pancreas. Its effects are antagonistic to those of
insulin. An increase in blood glucose stimulates the pancreas to produce
insulin which, in turn, promotes the uptake and utilization of glucose by cells
lowering its concentration. A reduction in blood glucose stimulates release of
glucagon that promotes glycogenolysis in the liver thereby increasing blood
glucose levels (Figure 7.24). Disorders of insulin release or
activity can cause an increase in blood glucose, hyperglycemia, or its
reduction, hypoglycemia.
Related Topics