Chapter: Biology of Disease: Disorders of the Endocrine System
Disorders of Sex Hormones
DISORDERS OF SEX HORMONES
Disorders associated with male sex hormones include hypogonadism and gynecomastia. In the former, there is deficient sperm production and decreased testosterone secretion. Hypogonadism can occur because of testicular disease, referred to as primary or hypergonadotrophic hypogonadism, or to a defect in the hypothalamus or pituitary gland leading to secondary or hypogonado-trophic hypogonadism. In the latter, there may be a deficiency of both gonado-trophins or only of LH. The causes of primary hypogonadism are varied. They include congenital defects, such as Klinefelter syndrome , a deficiency of 5 α -reductase activity, testicular agenesis (failure of the testes to develop), acquired defects due to testicular infections, for example mumps or cytotoxic drugs, trauma or irradiation. The causes of secondary hypogonad-ism include pituitary tumors and hypothalamic disorders such as Kallmann’s syndrome. The treatment of hypogonadism is usually directed at the underly-ing cause. Testosterone is given in cases of testosterone deficiency. However, if fertility is required then gonadotrophins may have to be administered.
Gynecomastia, or breast development in males, is usually related to a disturbance in the balance of estrogens to androgens. In puberty, it occurs in approximately 50% of normal boys due to a temporary increase in the secretion of estrogens. Other than at puberty, the condition is pathological. It may arise because of decreased androgen activity in hypogonadism or because of increased estrogen production from various endocrine tumors. Such tumors may secrete large quantities of estrogens or may secrete hCG that stimulates estrogen production. Some drugs possess estrogen or antiandrogen activity and their use can lead to gynecomastia.
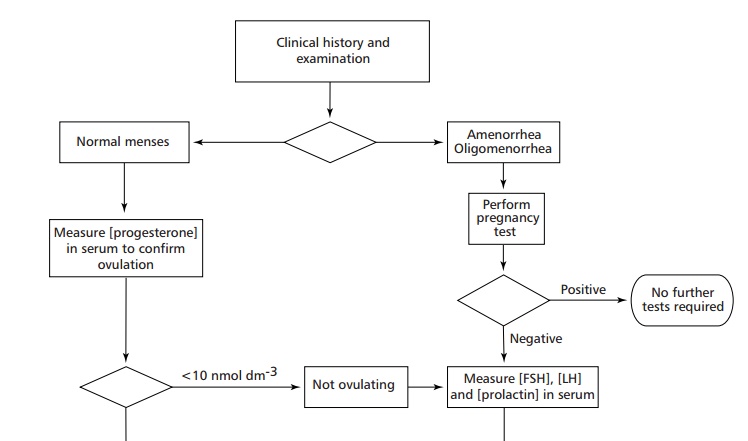
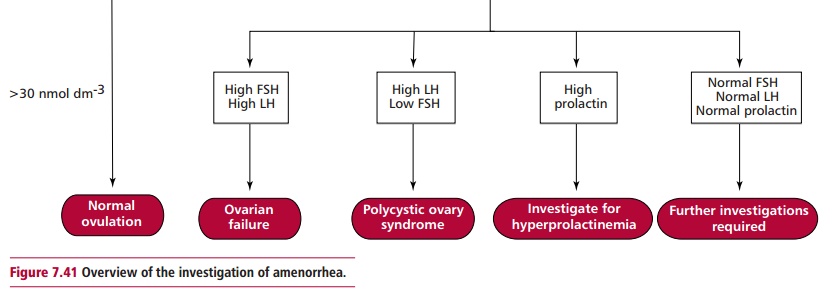
Disorders associated with female sex hormones include amenorrhea, oligomenorrhea, infrequent menstruation, and virilism, with the developmentof hirsutism, muscle mass, deepening of the voice and male psychological characteristics. Amenorrhea can be primary where menstruation fails to occur by the age of 16 years, or secondary, where menstruation stops for three months or more after normal menstruation has been established and before menopause. The other clinical features of amenorrhea include hirsutism, acne, menstrual cycle disturbances and obesity, although these features vary in their severity and prevalence. A common reason for secondary amenorrhea in females is pregnancy. This condition must be excluded before other possible causes, for example stress, severe weight loss, polycystic ovary syndrome (PCOS, see below), gonad dysgenesis, such as in Turner syndrome, the decrease in gonadotrophin secretion associated with some tumors,hyperprolactinemia and congenital adrenal hyperplasia, are investigated. The causes of amenorrhea are investigated by measuring the concentrations of FSH, LH and prolactin in plasma as outlined in Figure 7.41. A high value for FSH indicates ovarian failure. One for prolactin suggests hyperprolactinemia and requires further investigations to confirm this diagnosis. If, however, the values for FSH, LH and prolactin are normal, further tests to investigate pituitary or hypothalamic diseases are necessary. The management of amenorrhea is aimed at treating its underlying cause.
Patients with virilism present with enlargement of the clitoris, deepening of the voice, atrophy of the breasts and hirsutism. Hair growth is not only excessive but shows a male-like distribution. The cause of virilism is increased androgen secretion although abnormally low levels of SHBG can also increase the free testosterone fraction. In some cases virilism occurs because of an increased sensitivity to androgens by target cells. Its causes include PCOS, androgen secreting tumors, congenital adrenal hyperplasia, Cushing’s syndrome and may be iatrogenic following treatment with androgens and progesterone. Its commonest cause is PCOS, characterized by multiple cysts in the ovaries that arise from follicles that have failed to ovulate. The ovaries secrete large amounts of androgens although why this is so is unclear.
Many patients with PCOS suffer from acne, obesity, type 2 diabetes mellitus and may be infertile. A diagnosis of PCOS is made on clinical grounds and assisted by ultrasonography. Plasma LH is often increased in these patients but may be normal, whereas the concentration of testosterone is increased. Treatment of severe PCOS may involve using the antiandrogen drug, cyproterone but this leads to infertility. If fertility is required, then clomiphene, an antiestrogen drug, may be used and can induce ovulation in 75% of cases.
Infertility
Infertility is defined as a failure to conceive despite regular unprotected sexual intercourse for one year. Female infertility may be due to failure to ovulate, obstruction of the Fallopian tubes or to diseases of the uterine lining. In females, failures to ovulate due to hyperprolactinemia or to hypothalamic-pituitary dysfunction are responsible for 20% of cases of infertility. Damage to the Fallopian tubes may also be a cause of female infertility. Male infertility is usually due to decreased numbers or motility of sperm (oligospermia) or complete absence of sperm (azoospermia). Infertility due to endocrine dysfunction occurs only rarely in males. The normal volume of ejaculate is 2 to 5 cm3 and contains 40 to 500 million sperm. A sperm count of less than 20 million per cm3 is believed to be subnormal and causes 25% of infertility cases. In general, the lower the total sperm number the greater the chances of infertility although men with low counts have been known to father children. The motility of sperm is also necessary for fertilization to take place and at least 60% of sperm should have a normal shape and be mobile with beating flagella.
Investigating infertility involves a clinical and laboratory evaluation of both partners. Women should be investigated for regular menstruation. If it is regular, then ovulation is probably occurring. The concentration of progesterone in plasma is also indicative and should exceed 30 nmol dm–3 on day 21 of the menstrual cycle, values below 10 nmol dm–3 are suggestive of abnormal ovulation. If ovulation is confirmed then it may be necessary to examine cervical mucus following intercourse to determine the presence of motile, normal shaped sperm.
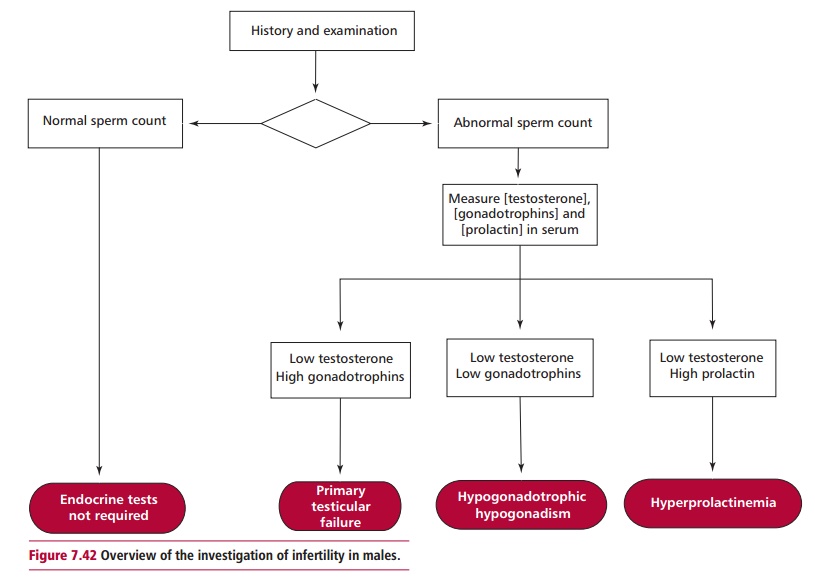
Microscopic examination of samples of ejaculate will indicate whether the sperm produced are motile and normal in shape or show abnormalities, such as malformed heads and twin sperm formed by a failure in development. Sperm counts will show if adequate numbers of sperm are produced. A low sperm count may be further investigated by measuring the concentrations of testosterone, FSH and LH in the plasma to compare with their reference ranges of 9–30 nmol dm–3, 2–10 U dm–3 and 2–10 U dm–3respectively. In some cases, a biopsy of the testes may by necessary. Investigation of infertility in males is outlined in Figure 7.42.
Related Topics