Chapter: Basic & Clinical Pharmacology : Antiprotozoal Drugs
Pentamidine Antiprotozoal Drugs
PENTAMIDINE
Pentamidine has
activity against trypanosomatid protozoans and against P jiroveci, but toxicity is significant.
Chemistry & Pharmacokinetics
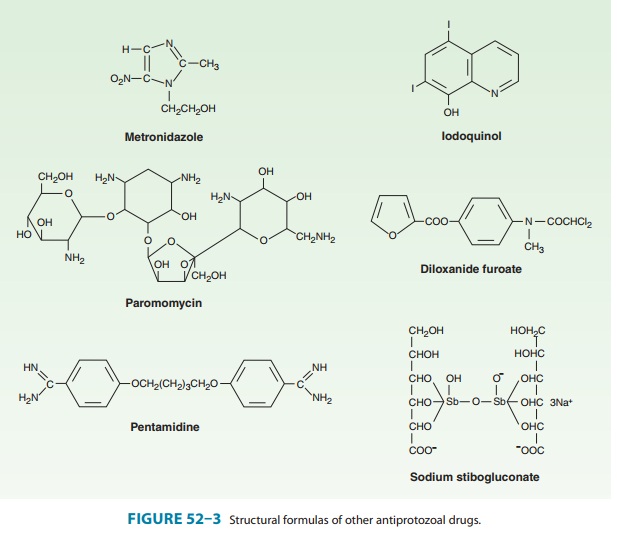
Pentamidine is an aromatic diamidine (Figure 52–3) formulated as an isethionate salt. Pentamidine is only administered parenter-ally. The drug leaves the circulation rapidly, with an initial half-life of about 6 hours, but it is bound avidly by tissues. Pentamidine thus accumulates and is eliminated very slowly, with a terminal elimination half-life of about 12 days. The drug can be detected in urine 6 or more weeks after treatment. Only trace amounts of pentamidine appear in the central nervous system, so it is not effective against central nervous system African trypanosomiasis. Pentamidine can also be inhaled as a nebulized powder for the prevention of pneumocystosis. Absorption into the systemic circu-lation after inhalation appears to be minimal. The mechanism of action of pentamidine is unknown.
Clinical Uses
A. Pneumocystosis
Pentamidine
is a well-established alternative therapy for pulmo-nary and extrapulmonary
disease caused by P jiroveci. The
drug has somewhat lower efficacy and greater toxicity than
trimetho-prim-sulfamethoxazole. The standard dosage is 3 mg/kg/d intrave-nously
for 21 days. Significant adverse reactions are common, and with multiple
regimens now available to treat P
jiroveci infection, pentamidine is best reserved for patients with severe
disease who cannot tolerate or fail other drugs.
Pentamidine is also an
alternative agent for primary or second-ary prophylaxis against pneumocystosis
in immunocompromised individuals, including patients with advanced AIDS. For
this indi-cation, pentamidine is administered as an inhaled aerosol (300 mg
inhaled monthly). The drug is well tolerated in this form. Its effi-cacy is
very good but clearly less than that of daily trimethoprim-sulfamethoxazole.
Because of its cost and ineffectiveness against nonpulmonary disease, it is
best reserved for patients who cannot tolerate oral chemoprophylaxis with other
drugs.
B. African Trypanosomiasis (Sleeping Sickness)
Pentamidine has been used since 1940 and is the drug of choice to treat the early hemolymphatic stage of disease caused by Trypanosomabrucei gambiense (West African sleeping sickness). The drug is infe-rior to suramin for the treatment of early East African sleeping sick-ness. Pentamidine should not be used to treat late trypanosomiasis with central nervous system involvement. A number of dosing regi-mens have been described, generally providing 2–4 mg/kg daily or on alternate days for a total of 10–15 doses. Pentamidine has also been used for chemoprophylaxis against African trypanosomiasis, with dosing of 4 mg/kg every 3–6 months.
C. Leishmaniasis
Pentamidine is an
alternative to sodium stibogluconate in the treatment of visceral
leishmaniasis, with similar efficacy, although resistance has been reported.
The drug has been successful in some cases that have failed therapy with
antimonials. The dosage is 2–4 mg/kg intramuscularly daily or every other day
for up to 15 doses, and a second course may be necessary. Pentamidine has also
shown success against cutaneous leishmaniasis, but it is not rou-tinely used
for this purpose.
Adverse Effects & Cautions
Pentamidine is a
highly toxic drug, with adverse effects noted in about 50% of patients
receiving 4 mg/kg/d. Rapid intravenous administration can lead to severe
hypotension, tachycardia, dizzi-ness, and dyspnea, so the drug should be
administered slowly (over 2 hours), and patients should be recumbent and monitored
closely during treatment. With intramuscular administration, pain at the
injection site is common, and sterile abscesses may develop.
Pancreatic toxicity is
common. Hypoglycemia due to inappro-priate insulin release often appears 5–7
days after onset of treat-ment, can persist for days to several weeks, and may
be followed by hyperglycemia. Reversible renal insufficiency is also common.
Other adverse effects include rash, metallic taste, fever, gastro-intestinal
symptoms, abnormal liver function tests, acute pancrea-titis, hypocalcemia,
thrombocytopenia, hallucinations, and cardiac arrhythmias. Inhaled pentamidine
is generally well tolerated but may cause cough, dyspnea, and bronchospasm.
Related Topics