Chapter: Psychology: Motivation and Emotion
Obesity
Obesity
The
physiological and cognitive mechanisms regulating an organism’s food intake
work remarkably well—but not perfectly. We see this in the fact that organisms
(humans in particular!) can end up either weighing far more than is healthy for
them or weighing too little. In some cases, the person is underweight
because—tragically—poverty and malnutrition are common problems in many parts
of the world (including nations that we would otherwise consider relatively
wealthy). Even when food is available, though, people can end up underweight.
Here, we deal with the more common problem in the Western world: obesity, a
problem so widespread that the World Health Organization has classified obesity
as a global epidemic (Ravussin & Bouchard, 2000).
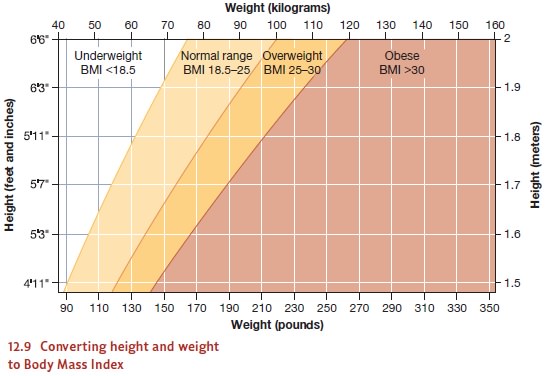
Obesity
is sometimes defined as a body weight that exceeds the average for a given
height by 20%. More commonly, though, researchers use a definition cast in
terms of the Body Mass Index (BMI),
defined as someone’s weight in kilograms divided by the square of his height in
meters (Figure 12.9). A BMI between 18.5 and 24.9 is considered normal. A BMI
between 25 and 30 counts as overweight, and a BMI of 30 or more is considered
obese. A BMI over 40 defines morbid
obesity—the level of obesity at which someone’s health is genuinely at
risk. For most people, morbid obesity means a weight roughly 100 pounds (45.3
kg) beyond their ideal.
THE GENETICROOTS OF OBESITY
Why
do people become obese? The simplest hypothesis is that some people eat too
much. In this view, obesity might be understood as the end result of
self-indulgence, or perhaps the consequence of an inability to resist temptation.
This hypothesis makes it seem like people could be blamed for their obesity,
like the condition is, in essence, their own fault. Such a view of obesity,
however, is almost certainly a mistake, because it ignores the powerful forces
that can put someone on the path toward obesity in the first place. Although
people do have considerable control over what and how much they eat, the
evidence suggests that some people are strongly genetically predisposed toward
obesity.
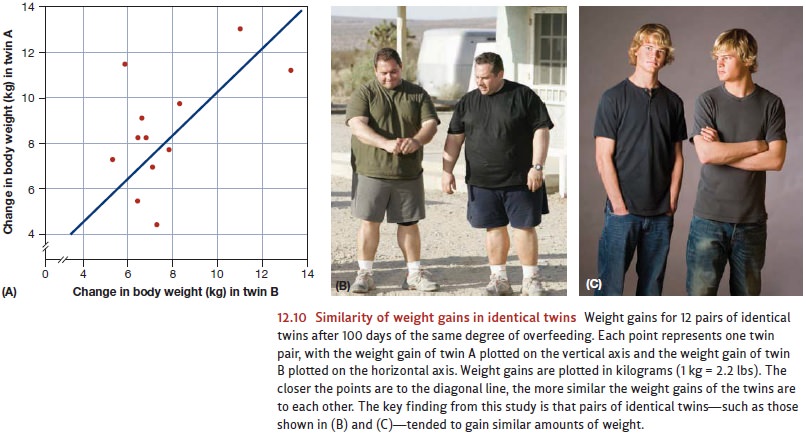
One
long-term study examined 12 pairs of male identical twins. Each of these men
ate about 1,000 calories per day above the amount required to maintain his
initial weight. The activities of each participant were kept as close to
equivalent as possible, and there was very little exercise. This regimen
continued for 100 days. Needless to say, all 24 men gained weight, but the
amounts they gained varied substantially, from about 10 to 30 pounds. The men
also differed in terms of where on their bodies the weight was deposited. For
some participants, it was the abdomen; for others, it was the thighs and
buttocks. Crucially, though, the amount each person gained was statistically
related to the weight gain of his twin (Figure 12.10). The twins also tended to
deposit the weight in the same place. If one developed a prominent paunch, so
did his twin; if another deposited the fat in his thighs, his twin did, too
(Bouchard, Lykken, McGue, Segal, & Tellegen, 1990; also see Herbert et al.,
2006).
It
seems, therefore, that the tendency to turn extra calories into fat has a
genetic basis. In fact, several mechanisms may be involved in this pattern, so
that, in the end, obesity can arise from a variety of causes. For example, some
people seem to be less sen-sitive to the appetite-reducing signals from leptin
and thus are more vulnerable to the effects of appetite stimulants such as NPY
(J. Friedman, 2003). For these people, a
tendency
to overeat may be genetically rooted. In addition, people differ in the
effi-ciency of their digestive apparatus, with some people simply extracting
more calories from any given food. People also differ in their overall
metabolic level; if, as a result, less nutrient fuel is burned up, then more is
stored as fat (Astrup, 2000; also M. I. Friedman, 1990a, b; Sims, 1986).
Given
these various mechanisms, should we perhaps think about obesity as some sort of
genetic defect, a biologically rooted
condition that leads to substantial health risk? Proponents of the “thrifty
gene” hypothesis emphatically reject this suggestion. They note that our
ancestors lived in times when food supplies were unpredictable and food
shortages were common, so natural selection may have favored individuals who
had especially inefficient metabolisms and, as a result, stored more fat. These
individu-als would have been better prepared for lean times and thus may have
had a survival advantage. As a result, the genes leading to this fat storage
might have been assets, not defects (J. Friedman, 2003; Fujimoto et al., 1995;
Groop & Tuomi, 1997; Ravussin, 1994).
ENVIRONMENTAL FACTORS AND OBESITY
Clearly,
then, “thrifty genes” might have helped our ancestors to maintain a healthy
body weight, but our ancestors lived in a time in which food was scarce. The
same genes will have a different outcome in modern times—especially for people
living in an afflu-ent culture in which a quick trip to the supermarket provides
all the calories one wishes. In this modern context, the “thrifty genes” can
lead to levels of obesity that create seri-ous health problems.
Whether
for genetic reasons, though, or otherwise, the evidence is clear that obesity
rates are climbing across the globe. In the United States, roughly 23% of the
population in 1991 was obese; more recent estimates of the rate—30%—are
appreciably higher (J. Friedman, 2003). Similar patterns are evident in other
countries. Over the last 10 years, for example, the obesity rates in most
European countries have increased by at least 10%, and, in some countries, by
as much as 40%. These shifts cannot reflect changes in the human genome;
genetic changes proceed at a much slower pace. Instead, the increase has to be understood
in terms of changes in diet and activity level—with people consuming more
calorically dense, high-fat foods and living a lifestyle that causes them to
expend relatively few calories in their daily routines.
This
increase in obesity rates is associated with increased rates of many health
problems, including heart attack, stroke, Type 2 diabetes, and some types of
cancer. The debate continues over the severity of these risks for people with
moderate levels of obesity—e.g., a BMI between 30 and 40 (Couzin, 2005; Yan et
al., 2006). There is no debate, however, about the health risks of so-called
morbid obesity (a BMI of 40 or higher), and this makes the worldwide statistics
on obesity a serious concern for health professionals.
Related Topics