Chapter: Medical Surgical Nursing: Assessment and Management of Patients With Hepatic Disorders
Management of Patients With Hepatitis B Virus (HBV)
HEPATITIS
B VIRUS (HBV)
Unlike
hepatitis A, which is transmitted primarily by the fecal–oral route, hepatitis
B is transmitted primarily through blood (percuta-neous and permucosal routes).
HBV has been found in blood, saliva, semen, and vaginal secretions and can be
transmitted through mucous membranes and breaks in the skin. HBV is also
trans-ferred from carrier mothers to their babies, especially in areas with a
high incidence (ie, Southeast Asia). The infection is usually not via the umbilical
vein, but from the mother at the time of birth and during close contact
afterward.
HBV
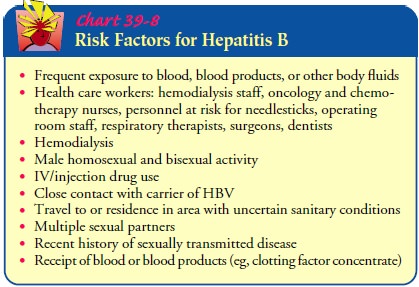
has a long incubation period. It replicates in the liver and remains in the
serum for relatively long periods, allowing transmission of the virus. Those at
risk for developing hepatitis B include surgeons, clinical laboratory workers,
dentists, nurses, and respiratory therapists. Staff and patients in
hemodialysis and oncology units and sexually active homosexual and bisexual men
and injection drug users are also at increased risk. Screening of blood donors
has greatly reduced the occurrence of hepatitis B after blood transfusion.
Most
people (>90%) who contract hepatitis B infections will develop antibodies
and recover spontaneously in 6 months. The mortality rate from hepatitis B has
been reported to be as high as 10%. Another 10% of patients who have hepatitis
B progress to a carrier state or develop chronic hepatitis with persistent HBV
infection and hepatocellular injury and inflammation. It remains a major cause
of cirrhosis and hepatocellular carcinoma world-wide (Chart 39-8).
Clinical Manifestations
Clinically,
the disease closely resembles hepatitis A, but the incu-bation period is much
longer (1 to 6 months). Signs and symp-toms of hepatitis B may be insidious and
variable. Fever and respiratory symptoms are rare; some patients have
arthralgias and rashes. The patient may have loss of appetite, dyspepsia,
abdom-inal pain, generalized aching, malaise, and weakness. Jaundice may or may
not be evident. If jaundice occurs, light-colored stools and dark urine
accompany it. The liver may be tender and enlarged to 12 to 14 cm vertically.
The spleen is enlarged and pal-pable in a few patients; the posterior cervical
lymph nodes may also be enlarged. Subclinical episodes also occur frequently.
Assessment and Diagnostic Findings
HBV is
a DNA virus composed of the following antigenic particles:
•
HBcAg—hepatitis B core antigen (antigenic material
in an inner core)
•
HBsAg—hepatitis B surface antigen (antigenic
material on surface of HBV)
•
HBeAg—an independent protein circulating in the
blood
•
HBxAg—gene product of X gene of HBV/DNA
Each
antigen elicits its specific antibody and is a marker for different stages of
the disease process:
•
anti-HBc—antibody to core antigen or HBV; persists
dur-ing the acute phase of illness; may indicate continuing HBV in the liver
•
anti-HBs—antibody to surface determinants on HBV;
de-tected during late convalescence; usually indicates recovery and development
of immunity
•
anti-HBe—antibody to hepatitis B e-antigen; usually
signi-fies reduced infectivity
•
anti-HBxAg—antibody to the hepatitis B x-antigen;
may indicate ongoing replication of HBV
HBsAg
appears in the circulation in 80% to 90% of infected pa-tients 1 to 10 weeks
after exposure to HBV and 2 to 8 weeks before the onset of symptoms or an
increase in transferase (transaminase) levels. Patients with HBsAg that
persists for 6 or more months after acute infection are considered HBsAg
carriers (Befeler & Di Bisceglie, 2000). HBeAg is the next antigen of HBV
to appear in the serum. It usually appears within a week of the appearance of
HBsAg and before changes in aminotransferase levels, disappearing from the
serum within 2 weeks. HBV DNA, detected by poly-merase chain reaction testing,
appears in the serum at about the same time as HBeAg. HBcAg is not always
detected in the serum in HBV infection.
About
15% of American adults are positive for anti-HBs, which indicates that they
have had hepatitis B. Anti-HBs may be positive in as many as two thirds of
IV/injection drug users.
Prevention
The
goals of prevention are to interrupt the chain of transmis-sion, to protect
people at high risk with active immunization through the use of hepatitis B
vaccine, and to use passive immu-nization for unprotected people exposed to
HBV.
PREVENTING TRANSMISSION
Continued
screening of blood donors for the presence of hepati-tis B antigens will
further decrease the risk of transmission by blood transfusion. The use of
disposable syringes, needles, and lancets and the introduction of needleless IV
administration sys-tems reduce the risk of spreading this infection from one
patient to another or to health care personnel during the collection of blood
samples or the administration of parenteral therapy. Good personal hygiene is
fundamental to infection control. In the clin-ical laboratory, work areas
should be disinfected daily. Gloves are worn when handling all blood and body
fluids as well as HBAg-positive specimens, or when there is potential exposure
to blood (blood drawing) or to patients’ secretions. Eating and smoking are
prohibited in the laboratory and in other areas exposed to se-cretions, blood,
or blood products. Patient education regarding the nature of the disease, its
infectiousness, and prognosis is a crit-ical factor in preventing transmission
and protecting contacts.
ACTIVE IMMUNIZATION: HEPATITIS B VACCINE
Active
immunization is recommended for individuals at high risk for hepatitis B (eg,
health care personnel and hemodialysis patients). In addition, individuals with
hepatitis C and other chronic liver diseases should receive the vaccine (CDC,
1999).
A
yeast-recombinant hepatitis B vaccine (Recombivax HB) is used to provide active
immunity. Long-term studies of healthy adults and children indicate that
immunologic memory remains intact for at least 5 to 10 years, although antibody
levels may be-come low or undetectable. Measurable levels of antibodies may not
be essential for protection. In those with normal immune sys-tems, booster
doses are not generally required. The CDC (2002) does not recommend booster
doses at this time except for he-modialysis patients. The need for booster
doses may be revisited if reports of hepatitis B increase or an increased
prevalence of the carrier state develops, indicating that protection is
declining.
A
hepatitis B vaccine prepared from plasma of humans chroni-cally infected with
HBV is used only rarely and in patients who are immunodeficient or allergic to
recombinant yeast-derived vaccines.
Both
forms of the hepatitis B vaccine are administered in-tramuscularly in three
doses, the second and third doses 1 and 6 months after the first dose. The
third dose is very important in producing prolonged immunity. Hepatitis B
vaccination should be administered to adults in the deltoid muscle. Antibody
response may be measured by anti-HBs levels 1 to 3 months after complet-ing the
basic course of vaccine, but this testing is not routine and not currently
recommended. Individuals who fail to respond may benefit from one to three
additional doses (Koff, 2001).
People
at high risk, including nurses and other health care per-sonnel exposed to
blood or blood products, should receive active immunization. Health care
workers who have had frequent con-tact with blood are screened for anti-HBs to
determine whether im-munity is already present from previous exposure. The
vaccine produces active immunity to HBV in 90% of healthy people (Koff, 2001).
It does not provide protection to those already exposed to HBV and provides no
protection against other types of viral hep-atitis. Side effects of
immunization are infrequent; soreness and redness at the injection site are the
most common complaints.
Because
hepatitis B infection is frequently transmitted sexually, hepatitis B
vaccination is recommended for all unvaccinated per-sons being evaluated for a
sexually transmitted disease (STD). It is also recommended for those with a
history of an STD, per-sons with multiple sex partners, those who have sex with
injection drug users, and sexually active men who have sex with other men (CDC,
2002).
Universal
childhood vaccination for hepatitis B prevention has been instituted in the
United States. Vaccination was initially targeted for select high-risk
populations, but the U.S. Public
Health
Service and the CDC (1999) have endorsed universal vac-cination of all infants.
Catch-up vaccination is also recommended for all children and adolescents up to
the age of 19 who were not previously immunized. Studies (Chang, 2000; Wu et
al., 1999) show that universal vaccination of all newborns in endemic areas has
dramatically reduced the carrier rate among children and the incidence of
childhood hepatocellular carcinoma. In the United States, studies regarding the
effectiveness of the vaccine are ongo-ing, but it is known that clinical
infection is rarely observed during long-term follow-up of known responders
(ie, health care workers) who seroconverted within 3 months of the third dose
of vaccine (Bircher et al., 1999). Development of chronic carrier states has
not been reported in adult responders to the vaccine.
PASSIVE IMMUNITY: HEPATITIS B IMMUNE GLOBULIN
Hepatitis B immune globulin (HBIG) provides passive immunity to
hepatitis B and is indicated for people exposed to HBV who have never had
hepatitis B and have never received hepatitis B vaccine. Specific indications
for postexposure vaccine with HBIG include: (1) inadvertent exposure to HBAg-positive blood
through percu-taneous (needlestick) or transmucosal (splashes in contact with
mu-cous membrane) routes, (2) sexual contact with people positive for HBAg, and
(3) perinatal exposure (babies born to HBV-infected mothers should receive HBIG
within 12 hours of delivery). HBIG, which provides passive immunity, is
prepared from plasma selected for high titers of anti-HBs. Prompt immunization
with HBIG (within hours to a few days after exposure to hepatitis B) increases
the likelihood of protection. Both active and passive immunization are
recommended for people exposed to hepatitis B through sexual contact or through
percutaneous or transmucosal routes. If HBIG and hepatitis B vaccine are
administered at the same time, separate sites and separate syringes should be
used. Prophylaxis with high doses of HBIG started at the time of liver
transplantation and con-tinued indefinitely improves survival by thwarting
recurrence of hepatitis B (Bacon & Di Bisceglie, 2000). There has been no
evi-dence that HIV infection can be transmitted by HBIG.
Gerontologic Considerations
The
elderly patient who contracts hepatitis B has a serious risk of severe liver
cell necrosis or fulminant hepatic failure, particularly if other illnesses are
present. The patient is seriously ill and the prog-nosis is poor, so efforts
should be undertaken to eliminate other factors (eg, medications, alcohol) that
may affect liver function.
Medical Management
The
goals of treatment are to minimize infectivity, normalize liver inflammation,
and decrease symptoms. Of all the agents that have been used to treat chronic
type B viral hepatitis, alpha in-terferon as the single modality of therapy
offers the most promise. This regimen of 5 million units daily or 10 million
units three times weekly for 4 to 6 months results in remission of disease in
approximately one third of patients (Befeler & Di Bisceglie, 2000). The
long-term benefits of this treatment are being as-sessed. Interferon must be
administered by injection and has sig-nificant side effects, including fever,
chills, anorexia, nausea, myalgias, and fatigue. Late side effects are more
serious and may necessitate dosage reduction or discontinuation. These include
bone marrow suppression, thyroid dysfunction, alopecia, and bacterial
infections.
Two
antiviral agents (lamivudine [Epvir] and adefovir [Hep-sera]) oral nucleoside
analogs, have been approved for use in chronic hepatitis B in the United
States. Viral resistance may be an issue with these agents, and studies of
their effectiveness alone and in combination with other therapies are ongoing
(Befeler & Di Bisceglie, 2000).
Bed
rest may be recommended, regardless of other treatment, until the symptoms of
hepatitis have subsided. Activities are re-stricted until the hepatic
enlargement and elevated levels of serum bilirubin and liver enzymes have
disappeared. Gradually increased activity is then allowed.
Adequate
nutrition should be maintained; proteins are re-stricted when the liver’s
ability to metabolize protein byproducts is impaired, as demonstrated by
symptoms. Measures to control the dyspeptic symptoms and general malaise
include the use of antacids and antiemetics, but all medications should be
avoided if vomiting occurs. If vomiting persists, the patient may require
hospitalization and fluid therapy. Because of the mode of transmission, the
patient is evaluated for other bloodborne diseases (eg, HIV infection).
Nursing Management
Convalescence
may be prolonged, with complete symptomatic recovery sometimes requiring 3 to 4
months or longer. During this stage, gradual resumption of physical activity is
encouraged after the jaundice has resolved.
The
nurse identifies psychosocial issues and concerns, partic-ularly the effects of
separation from family and friends if the pa-tient is hospitalized during the
acute and infective stages. Even if not hospitalized, the patient will be
unable to work and must avoid sexual contact. Planning is required to minimize
alterations in sensory perception. Planning that includes the family helps to
decrease their fears and anxieties about the spread of the disease.
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care.
Because of
the prolonged period ofconvalescence, the patient and family must be prepared
for home care. Provision for adequate rest and nutrition must be ensured. The
nurse informs family members and friends who have had in-timate contact with
the patient about the risks of contracting he-patitis B and makes arrangements
for them to receive hepatitis B vaccine or hepatitis B immune globulin as
prescribed. Those at risk must be aware of the early signs of hepatitis B and
of ways to reduce risk to themselves by avoiding all modes of transmission.
Patients with all forms of hepatitis should avoid drinking alcohol.
Continuing Care.
Follow-up
visits by a home care nurse may beneeded to assess the patient’s progress and
answer family mem-bers’ questions about disease transmission. A home visit also
per-mits assessment of the patient’s physical and psychological status and the
patient and family’s understanding of the importance of adequate rest and
nutrition. The nurse also reinforces previous instructions. Because of the risk
of transmission through sexual intercourse, strategies to prevent exchange of
body fluids are ad-vised, such as abstinence or the use of condoms. The nurse
em-phasizes the importance of keeping follow-up appointments and participating
in other health promotion activities and recom-mended health screenings.
Related Topics