Chapter: Medical Surgical Nursing: Assessment and Management of Patients With Hepatic Disorders
Liver Transplantation
Liver Transplantation
Liver
transplantation is used to treat life-threatening, end-stage liver disease for
which no other form of treatment is available. The transplantation procedure
involves total removal of the dis-eased liver and its replacement with a healthy
liver in the same anatomic location (orthotopic
liver transplantation [OLT]). Removal of the liver leaves a space for the
new liver and permits anatomic reconstruction of the hepatic vasculature and
biliary tract as close to normal as possible.
The
success of liver transplantation depends on successful immunosuppression.
Immunosuppressants currently in use in-clude cyclosporine (Neoral),
corticosteroids, azathioprine (Imuran), mycophenolate mofetil (CellCept), OKT3
(a monoclonal anti-body), tacrolimus (FK506, Prograf), sirolimus (formerly
known as rapamycin [Rapamune]), and antithymocyte globulin. Studies are
underway to find the most effective combination of immuno-suppressive agents
and to identify new agents with fewer side effects (Hebert et al., 1999;
Watson, Friend & Jamieson, 1999).
Despite
the success of immunosuppression in reducing the incidence of rejection of
transplanted organs, liver transplan-tation is not a routine procedure and may
be accompanied by complications related to the lengthy surgical procedure,
immunosuppressive therapy, infection, and the technical diffi-culties
encountered in reconstructing the blood vessels and bil-iary tract.
Long-standing systemic problems resulting from the primary liver disease may
complicate the preoperative and postoperative course. Previous surgery of the
abdomen, in-cluding procedures to treat complications of advanced liver disease
(ie, shunt procedures used to treat portal hypertension and esophageal varices)
increase the complexity of the trans-plantation procedure.
The
indications for liver transplantation are not as limited today as they were
when the procedure was first introduced, due to advances in immunosuppressive
therapy, improvements in bil-iary tract reconstruction, and in some cases the
use of venovenous bypass. General indications for liver transplantation include
irre-versible advanced chronic liver disease, fulminant hepatic failure,
metabolic liver diseases, and some hepatic malignancies. Exam-ples of disorders
that are indications for liver transplantation in-clude hepatocellular liver
disease (eg, viral hepatitis, drug- and alcohol-induced liver disease, and
Wilson’s disease) and cholesta-tic diseases (primary biliary cirrhosis,
sclerosing cholangitis, and biliary atresia).
The
patient being considered for liver transplantation fre-quently has many
systemic problems that influence preopera-tive and postoperative care. Because
transplantation is more difficult when the patient has developed severe GI
bleeding and hepatic coma, efforts are made to perform the procedure before
this stage.
Liver
transplantation is now recognized as an established ther-apeutic modality
rather than an experimental procedure to treat these disorders. As a result,
the number of centers where liver transplantation is performed is increasing.
Patients requiring transplantation are often referred from distant hospitals to
these sites. To prepare the patient and family for liver transplantation,
nurses in all settings must understand the processes and proce-dures of liver
transplantation.
SURGICAL PROCEDURE
The
donor liver is freed from other structures, the bile is flushed from the
gallbladder to prevent damage to the walls of the bil-iary tract, and the liver
is perfused with a preservative andcooled. Before the donor liver is placed in
the recipient, it is flushed with cold lactated Ringer’s solution to remove
potas-sium and air bubbles.
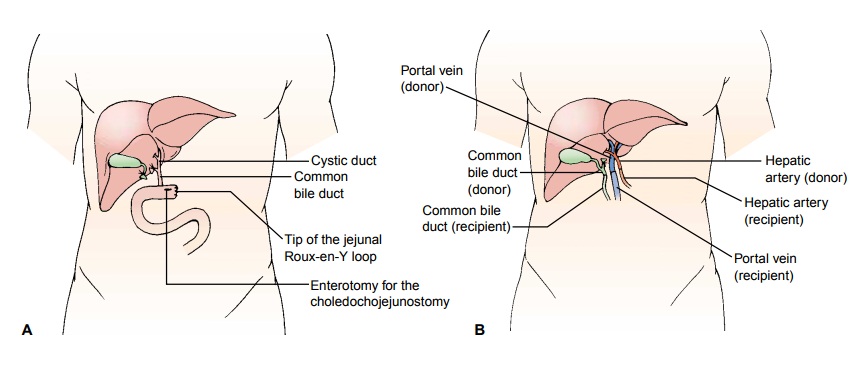
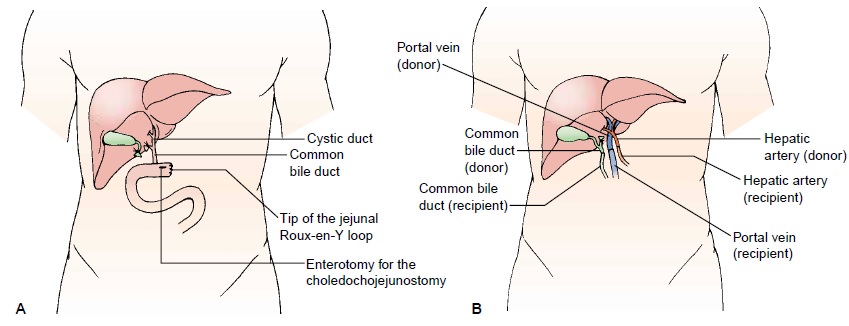
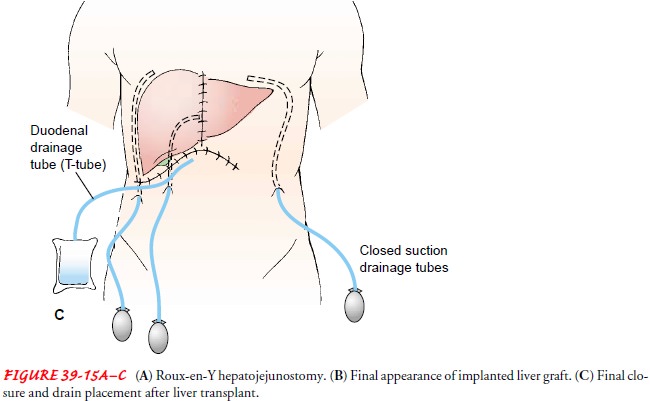
Anastomoses
(connections) of the blood vessels and bile duct are performed between the
donor liver and the recipient liver. Bil-iary reconstruction is performed with
an end-to-end anastomosis of the donor and recipient common bile ducts; a
stented T-tube is inserted for external drainage of bile. If an end-to-end
anastomosis is not possible because of diseased or absent bile ducts, an
end-to-side anastomosis is made between the common bile duct of the graft and a
loop (Roux-en-Y portion) of jejunum (Fig. 39-15A); in this case, bile drainage will be internal and a T-tube will
not be in-serted (Maddrey et al., 2001). Figure 39-15B and C illustrates the
final appearance of the grafted liver and final closure and drain placement.
Liver transplantation is a long surgical procedure, partly be-cause the patient with liver failure often has portal hypertension and
subsequently many venous collateral vessels that must be ligated. Blood loss
during the surgical procedure may be exten-sive. If the patient has adhesions
from previous abdominal surgery, lysis of adhesions is often necessary. If a shunt
proce-dure was performed previously, it must be surgically reversed to permit
adequate portal venous blood supply to the new liver. During the lengthy
surgery, providing regular updates to the family about the progress of the
operation and the patient’s sta-tus is helpful.
COMPLICATIONS
The
postoperative complication rate is high, primarily because of technical
complications or infection. Immediate postoperative complications may include
bleeding, infection, and rejection. Disruption, infection, or obstruction of
the biliary anastomosis and impaired biliary drainage may occur. Vascular
thrombosis and stenosis are other potential complications.
Bleeding
Bleeding
is common in the postoperative period and may result from coagulopathy, portal
hypertension, and fibrinolysis caused by ischemic injury to the donor liver.
Hypotension may occur in this phase secondary to blood loss. Administration of
platelets, fresh-frozen plasma, and other blood products may be necessary.
Hypertension is more common, but its cause is uncertain. Blood pressure
elevation that is significant or sustained is treated.
Infection
Infection
is the leading cause of death after liver transplantation. Pulmonary and fungal
infections are common; susceptibility to in-fection is increased by the
immunosuppression needed to prevent rejection (Maddrey et al., 2001).
Therefore, precautions must be taken to prevent nosocomial infections by strict
asepsis when ma-nipulating arterial lines and urine, bile, and other drainage
sys-tems; obtaining specimens; and changing dressings. Meticulous hand hygiene
is crucial.
Rejection
Rejection
is a key concern. A transplanted liver is perceived by the immune system as a
foreign antigen. This triggers an im-mune response, leading to the activation
of T lymphocytes that attack and destroy the transplanted liver.
Immunosuppressive agents are used long term to prevent this response and
rejection of the transplanted liver. These agents inhibit the activation of
immunocompetent T lymphocytes to prevent the production of effector T cells.
Although
the 1- and 5-year survival rates have increased dra-matically with the use of
new immunosuppressive therapies, these advances are not without major side
effects. A major side effect of cyclosporine, which is widely used in
transplantation, is nephrotoxicity; this problem seems to be dose-related, and
renal dysfunction can be reversed if the dose of cyclosporine is appropriately
decreased or if its use is not initiated immediately. Cyclosporine-related side
effects have caused many centers to use tacrolimus as first-line therapy
because of its efficacy and lower side effect profile.
Corticosteroids,
azathioprine, mycophenolate mofetil, rapa-mycin, antithymocyte globulin, and
OKT3 are also elements of the various regimens of immunosuppression and may be
used as the initial therapy to prevent rejection, or later to treat rejection.
Liver biopsy and ultrasound may be required to evaluate sus-pected episodes of
rejection.
Retransplantation
is usually attempted if the transplanted liver fails, but the success rate of
retransplantation does not approach that of initial transplantation.
Nursing Management
The
patient considering transplantation and the family have diffi-cult decisions to
make about treatment, use of financial resources, and relocation to another
area to be closer to the medical center. They also must cope with the patient’s
long-standing health prob-lems and perhaps social and family problems
associated with be-haviors that may be responsible for the patient’s liver
failure. Therefore, the time during which the patient and family are
con-sidering liver transplantation and awaiting the news that a liver is
available is often stressful. The nurse must be aware of these issues and
attuned to the emotional and psychological status of the pa-tient and family.
Referral of the patient and family to a psychiatric liaison nurse,
psychologist, psychiatrist, or spiritual advisor may be helpful to them as they
deal with the stressors associated with end-stage liver disease and liver
transplantation.
PREOPERATIVE NURSING INTERVENTIONS
If
irreversible, severe liver dysfunction has been diagnosed, the pa-tient may be
a candidate for transplantation. An extensive diag-nostic evaluation will be
carried out to determine whether the patient is a candidate. The nurse and
other health care team members provide the patient and family with full
explanations about the procedure, the chances of success, and the risks,
in-cluding the side effects of long-term immunosuppression. The need for close
follow-up and lifelong compliance with the thera-peutic regimen, including
immunosuppression, is explained to the patient and family.
Once
accepted as a candidate, the patient is placed on a wait-ing list at the
transplant center and patient information is entered into the United Network
for Organ Sharing (UNOS) computer system so that candidates may be matched with
appropriate or-gans as they become available.
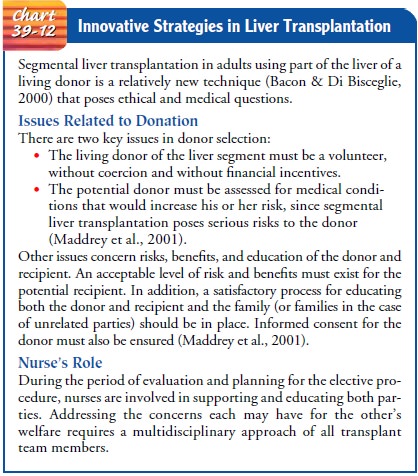
Unless
the patient is having a segmental liver transplanta-tion from a living donor (Chart
39-12), a liver becomes avail-able for transplantation only with the death of
another individual, who is usually healthy except for severe brain injury and
brain death. Thus, the patient and family undergo a stress-ful waiting period,
and the nurse is often the major source of support. The patient must be
accessible at all times in case an appropriate liver becomes available. During
this time, liver function may deteriorate further and the patient may
experi-ence other complications from the primary liver disease. Be-cause of the
current shortage of donor organs, many patients die awaiting transplantation.
Malnutrition,
massive ascites, and fluid and electrolyte distur-bances are treated before
surgery to increase the chance of a suc-cessful outcome. If the patient’s liver
dysfunction has a very rapid onset, as in fulminant hepatic failure, there is
little time or oppor-tunity for the patient to consider and weigh options and
their con-sequences; often this patient is in a coma, and the decision to proceed
with transplantation is made by the family.
The nurse coordinator is an integral member of the transplant team and plays an important role in preparing the patient for liver transplantation. The nurse serves as a patient and family advocate and assumes the important role of link between the patient and the other members of the transplant team. The nurse also serves as a resource to other nurses and health care team members involved in evaluating and caring for the patient.
POSTOPERATIVE NURSING INTERVENTIONS
The
patient is maintained in an environment as free from bac-teria, viruses, and
fungi as possible, because immunosuppressive medications reduce the body’s
natural defenses. In the imme-diate postoperative period, cardiovascular,
pulmonary, renal, neurologic, and metabolic functions are monitored
continu-ously. Mean arterial and pulmonary artery pressures are moni-tored
continuously. Cardiac output, central venous pressure, pulmonary capillary
wedge pressure, arterial and mixed venous blood gases, oxygen saturation,
oxygen demand and delivery, urine output, heart rate, and blood pressure are
used to evalu-ate the patient’s hemodynamic status and intravascular fluid
volume. Liver function tests, electrolyte levels, the coagulation profile,
chest x-ray, electrocardiogram, and fluid output, in-cluding urine, bile, and
drainage from Jackson-Pratt tubes, are monitored closely. Because the liver is
responsible for the stor-age of glycogen and the synthesis of protein and clotting
factors, these substances need to be monitored and replaced in the im-mediate
postoperative period.
Because
of the likelihood of atelectasis and an altered ventilation–perfusion ratio as
a result of the insult to the dia-phragm during the surgical procedure,
prolonged anesthesia, immobility, and postoperative pain, the patient will have
an en-dotracheal tube in place and will require mechanical ventilation during
the initial postoperative period. Suctioning is performed as required and
sterile humidification is provided.
As the
vital signs and condition stabilize, efforts are made to as-sist the patient to
recover from the trauma of this complex surgery. After removal of the
endotracheal tube, the nurse encourages the patient to use an incentive spirometer
to decrease the risk for atelectasis. Once the arterial lines and the urinary
catheter are removed, the patient is assisted to get out of bed, to ambulate as
tolerated, and to participate in self-care to prevent the compli-cations
associated with immobility. Close monitoring for signs and symptoms of liver
dysfunction and rejection will continue throughout the hospital stay. Plans
will be made for close follow-up after discharge as well. Teaching, initiated
during the pre-operative period, continues after surgery.
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care.Teaching the
patient and familyabout long-term measures to promote health is crucial for
success of the transplant and represents an important role of the nurse. The
patient and family must understand why they should adhere continuously to the
therapeutic regimen, with special emphasis on the methods of administration,
rationale, and side effects of the prescribed immunosuppressive agents. The
nurse provides written as well as verbal instructions about how and when to
take the medications. To avoid running out of medication or skipping a dose,
the patient must make sure that an adequate supply of medication is available.
Instructions are also provided about the signs and symptoms that indicate
problems that require consul-tation with the transplant team. The patient with
a T-tube in place must be taught how to manage the tube.
Continuing Care.The nurse
emphasizes the importance offollow-up blood tests and visits to the transplant
team. Trough blood levels of immunosuppressive agents are obtained, along with
other blood tests that assess the function of the liver and kidneys. During the
first months, the patient is likely to require blood tests two or three times a
week. As the patient’s condition stabilizes, blood studies and visits to the
transplant team are less frequent. The importance of routine ophthalmologic
examina-tions is emphasized because of the increased incidence of cataracts and
glaucoma with the long-term corticosteroid therapy used with transplantation.
Regular oral hygiene and follow-up dental care, with administration of
prophylactic antibiotics before dental treatments, are recommended because of
the immunosuppression.
The
nurse reminds the patient that although a successful transplantation will not
return him or her to normal, it does in-crease the chances for survival and a
more normal life than before transplantation if rejection and infection can be
prevented. Many patients have lived successful and productive lives after
receiving a liver transplant. In fact, pregnancy can be considered 1 year after
transplantation. Successful outcomes have been reported, but these pregnancies
are considered high risk for mother and in-fant (Sherlock & Dooley, 2002).
Related Topics