Chapter: Medical Surgical Nursing: Assessment and Management of Patients With Hepatic Disorders
Ascites - Hepatic Dysfunction
ASCITES
Pathophysiology
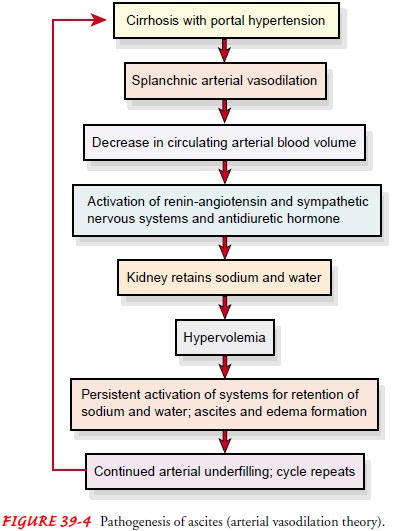
The
mechanisms responsible for the development of ascites are not completely
understood. Portal hypertension and the result-ing increase in capillary
pressure and obstruction of venous blood flow through the damaged liver are
contributing factors. The fail-ure of the liver to metabolize aldosterone
increases sodium and water retention by the kidney. Sodium and water retention,
increased intravascular fluid volume, and decreased synthesis of al-bumin by
the damaged liver all contribute to fluid moving from the vascular system into
the peritoneal space. Loss of fluid into the peritoneal space causes further
sodium and water retention by the kidney in an effort to maintain the vascular
fluid volume, and the process becomes self-perpetuating.
As a
result of liver damage, large amounts of albumin-rich fluid, 15 L or more, may
accumulate in the peritoneal cavity as ascites. With the movement of albumin
from the serum to the peritoneal cavity, the osmotic pressure of the serum
decreases. This, combined with increased portal pressure, results in move-ment
of fluid into the peritoneal cavity (Fig. 39-4).
Clinical Manifestations
Increased
abdominal girth and rapid weight gain are common presenting symptoms of
ascites. The patient may be short of breath and uncomfortable from the enlarged
abdomen, and striae and distended veins may be visible over the abdominal wall.
Fluid and electrolyte imbalances are common.
Assessment and Diagnostic Evaluation
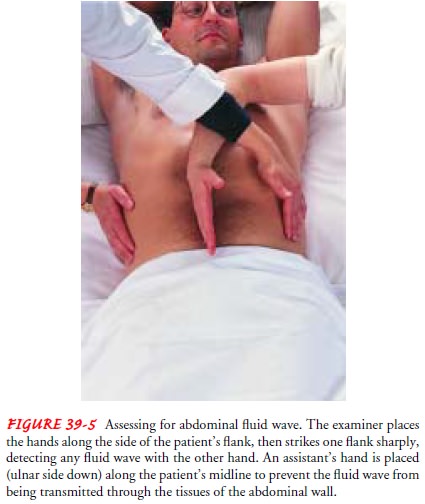
The presence and extent of ascites are assessed by percussion of the abdomen. When fluid has accumulated in the peritoneal cavity, the flanks bulge when the patient assumes a supine position. The presence of fluid can be confirmed either by percussing for shift-ing dullness or by detecting a fluid wave (Fig. 39-5). A fluid wave is likely to be found only when a large amount of fluid is present.
Daily
measurement and recording of abdominal girth and body weight are essential to
assess the progression of ascites and its re-sponse to treatment.
Medical Management
DIETARY MODIFICATION
The
goal of treatment for the patient with ascites is a negative sodium balance to
reduce fluid retention. Table salt, salty foods, salted butter and margarine,
and all ordinary canned and frozen foods (foods that are not specifically
prepared for low-sodium diets) should be avoided. It may take 2 to 3 months for
the patient’s taste buds to adjust to unsalted foods. In the meantime, the
taste of un-salted foods can be improved by using salt substitutes such as
lemon juice, oregano, and thyme. Commercial salt substitutes need to be approved
by the physician because those containing ammonia could precipitate hepatic
coma. Most salt substitutes contain potas-sium and should be avoided if the
patient has impaired renal func-tion. The patient should make liberal use of
powdered, low-sodium milk and milk products. If fluid accumulation is not
controlled with this regimen, the daily sodium allowance may be reduced
fur-ther to 500 mg, and diuretics may be administered.
Dietary
control of ascites via strict sodium restriction is diffi-cult to achieve at
home. The likelihood that the patient will fol-low even a 2-g sodium diet
increases if the patient and the person preparing meals understand the
rationale for the diet and receive periodic guidance about selecting and
preparing appropriate foods. Approximately 10% of patients with ascites respond
to these measures alone. Nonresponders and those who find sodium restriction
difficult require diuretic therapy.
DIURETICS
Use of diuretics along with sodium
restriction is successful in 90% of patients with ascites. Spironolactone
(Aldactone), an aldosterone-blocking agent, is most often the first-line
therapy in patients with ascites from cirrhosis. When used with other diuretics,
spirono-lactone helps prevent potassium loss. Oral diuretics such as furosemide
(Lasix) may be added but should be used cautiously because with long-term use
they may also induce severe sodium depletion (hyponatremia).
Ammonium
chloride and acetazolamide (Diamox) are con-traindicated because of the
possibility of precipitating hepatic coma. Daily weight loss should not exceed
1 to 2 kg (2.2 to 4.4 lb) in patients with ascites and peripheral edema or 0.5
to 0.75 kg (1.1 to 1.65 lb) in patients without edema. Fluid restriction is not
attempted unless the serum sodium concentration is very low.
Possible
complications of diuretic therapy include fluid and electrolyte disturbances
(including hypovolemia, hypokalemia, hyponatremia, and hypochloremic alkalosis)
and encephalopathy. Encephalopathy may be precipitated by dehydration and hypo-volemia.
Also, when potassium stores are depleted, the amount of ammonia in the systemic
circulation increases, which may cause impaired cerebral functioning and
encephalopathy.
BED REST
In
patients with ascites, an upright posture is associated with ac-tivation of the
renin-angiotensin-aldosterone system and sympa-thetic nervous system (Porth,
2002). This results in reduced renal glomerular filtration and sodium excretion
and a decreased re-sponse to loop diuretics. Bed rest may be a useful therapy, espe-cially
for patients whose condition is refractory to diuretics.
PARACENTESIS
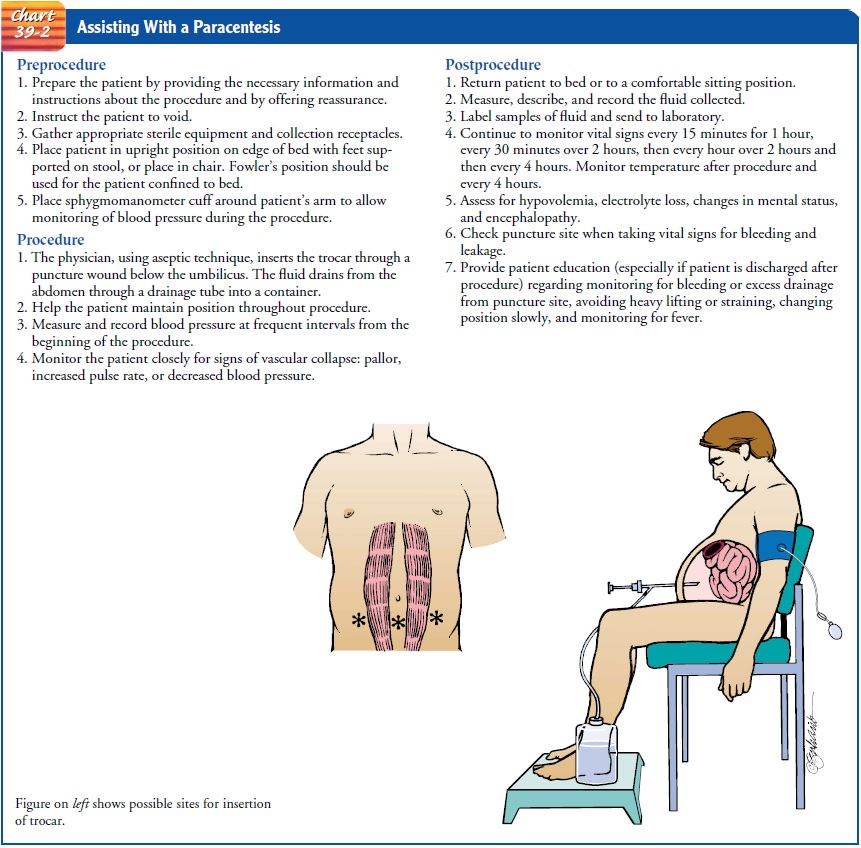
Paracentesis
is the removal of fluid (ascites) from the peritoneal cavity through a small
surgical incision or puncture made through the abdominal wall under sterile
conditions. Ultrasound guid-ance may be indicated in some patients at high risk
for bleeding because of an abnormal coagulation profile or in those who have
had previous abdominal surgery and who may have adhesions. Paracentesis was
once considered a routine form of treatment for ascites but is now performed
primarily for diagnostic examination of ascitic fluid, for treatment of massive
ascites that is resistant to nutritional and diuretic therapy and that is
causing severe problems to the patient, and as a prelude to diagnostic imaging
studies, peritoneal dialysis, or surgery. A sample of the ascitic fluid may be
sent to the laboratory for analysis. Cell count, albumin and total protein
levels, culture, and occasionally other tests are performed.
Use of
large-volume (5 to 6 liters) paracentesis has been shown to be a safe method
for treating patients with severe ascites. This technique, in combination with
the intravenous infusion of salt-poor albumin or other colloid, has become the
standard treatment for refractory, massive ascites (Krige & Beckingham,
2001; Menon Kamath, 2000). The salt-poor albumin helps reduce edema by causing
the ascitic fluid to be drawn back into the bloodstream and ultimately
eliminated by the kidneys. The procedure pro-vides only temporary removal of
fluid; it rapidly recurs, necessi-tating repeated removal. Nursing care of the
patient undergoing paracentesis is presented in Chart 39-2.
OTHER METHODS OF TREATMENT
Insertion of a peritoneovenous shunt to redirect ascitic fluid from the peritoneal cavity into the systemic circulation is a treatment modality for ascites, but this procedure is seldom used because of the high complication rate and high incidence of shunt failure. The shunt is reserved for those who are resistant to diuretic ther-apy, are not candidates for liver transplantation, have abdominal adhesions, or are ineligible for other procedures because of severe medical conditions, such as cardiac disease.
Nursing Management
If a
patient with ascites from liver dysfunction is hospitalized, nursing measures
include assessment and documentation of in-take and output, abdominal girth,
and daily weight to assess fluid status. The nurse monitors serum ammonia and
electrolyte levels to assess electrolyte balance, response to therapy, and
in-dicators of encephalopathy.
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care.
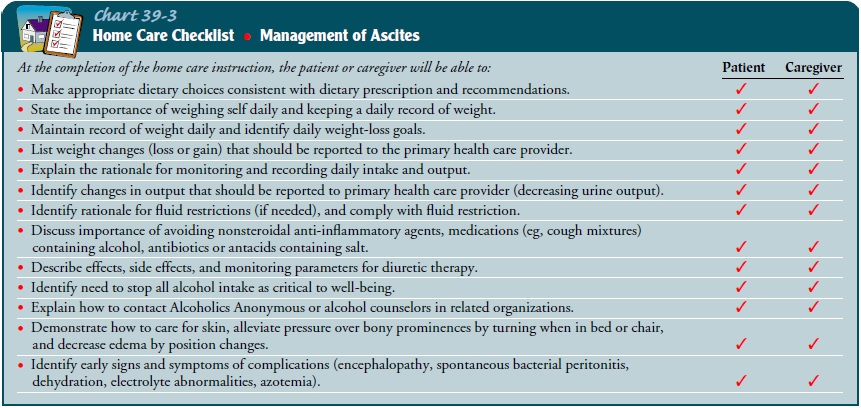
The patient
treated for ascites islikely to be discharged with some ascites still present.
Before hos-pital discharge, the nurse teaches the patient and family about the
treatment plan, including the need to avoid all alcohol intake, ad-here to a
low-sodium diet, take medications as prescribed, and check with the physician before taking any
new medications (Chart 39-3). Additional patient and family teaching addresses
skin care and the need to weigh the patient daily and to watch for and report
signs and symptoms of complications.
Continuing Care.
A referral for home care may be warranted,especially if the patient lives alone or cannot provide self-care. The home visit enables the nurse to assess changes in the patient’s condition and weight, abdominal girth, skin, and cognitive and emotional status. The home care nurse assesses the home envi-ronment and the availability of resources needed to adhere to the treatment plan (eg, a scale to obtain daily weights, facilities to pre-pare and store appropriate foods, resources to purchase needed medications). It is important to assess the patient’s adherence to the treatment plan and the ability to buy, prepare, and eat appropriate foods. The nurse reinforces previous teaching and emphasizes the need for regular follow-up and the importance of keeping scheduled health care appointments.
Related Topics