Chapter: Medical Surgical Nursing: Assessment and Management of Patients With Diabetes Mellitus
Implementing the Plan - Nursing Management of Patients With Diabetes Mellitus
IMPLEMENTING
THE PLAN
Teaching Experienced Diabetic Patients
The
nurse should continue to assess the skills of patients who have had diabetes
for many years, because it is estimated that up to 50% of patients may make
errors in self-care. Assessment of these patients must include direct
observation of skills, not just their self-report of self-care behaviors. In
addition, these patients must be fully aware of preventive measures related to
foot care, eye care, and risk factor management. If patients are experienc-ing
long-term diabetic complications for the first time, they may go through the
grieving process again. Some of these patients may have a renewed interest in
diabetes self-care in the hope of delay-ing further complications. Other
patients may be overwhelmed by feelings of guilt and depression. The patient is
encouraged to discuss feelings and fears related to complications; the nurse
meanwhile provides appropriate information regarding diabetic complications.
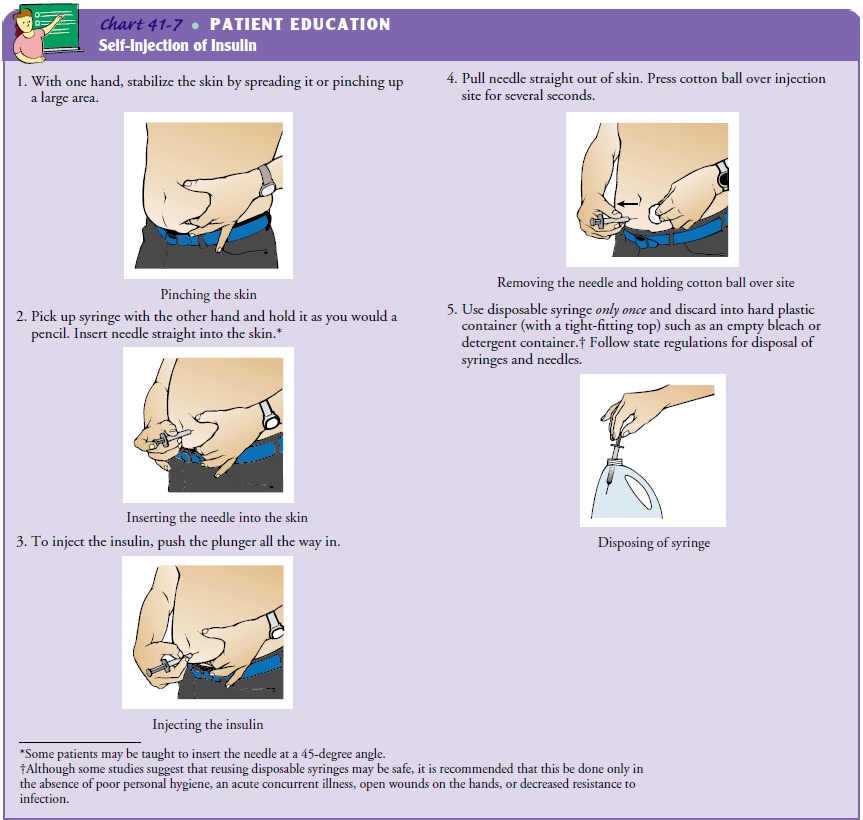
Teaching Patients to Self-Administer Insulin
Insulin
injections are administered into the subcutaneous tissue with the use of
special insulin syringes. A variety of syringes and injection-aid devices are
available. Chart 41-7 provides important information to include and evaluate
when teaching patients about insulin. Basic information includes explanation of
the equipment, insulins, syringes, and mixing insulin.
STORING INSULIN
Cloudy
insulins should be thoroughly mixed by gently inverting the vial or rolling it
between the hands before drawing the solu-tion into a syringe or a pen.
Whether
insulin is the short- or long-acting preparation, the vials not in use should
be refrigerated and extremes of tempera-ture should be avoided; insulin should
not be allowed to freeze and should not be kept in direct sunlight or in a hot
car. The insulin vial in use should be kept at room temperature to reduce local
irritation at the injection site, which may occur when cold insulin is injected.
If a vial of insulin will be used up in 1 month, it may be kept at room
temperature. Patients should be instructed to always have a spare vial of the
type or types of insulin they use (ADA, Insulin Administration, 2003). Spare
vials should be refrigerated.
Insulin
bottles should also be inspected for flocculation, which is a frosted, whitish
coating inside the bottle of intermediate- or long-acting insulins. This occurs
most commonly with human insulins that are not refrigerated. If a frosted,
adherent coating is present, some of the insulin is bound and should not be
used.
SELECTING SYRINGES
Syringes must be matched with the insulin concentration (eg, U-100). Currently, three sizes of U-100 insulin syringes are available:
•
1-mL (cc) syringes that hold 100 units
•
0.5-mL syringes that hold 50 units
•
0.3-mL syringes that hold 30 units
The
concentration of insulin used in the United States is U-100; that is, there are
100 units per milliliter (or cubic cen-timeter). Syringe size varies. Small
syringes allow patients who re-quire small amounts of insulin to measure and
draw up the amount of insulin accurately. Patients who require large amounts of
insulin would use larger syringes. Although there is a U-500 (500 units/mL)
concentration of insulin available by special order for patients who have
severe insulin resistance and require mas-sive doses of insulin, it is rarely
used. (Individuals who travel out-side of the United States should be aware
that insulin is available in 40-U concentration to avoid dosing errors.)
Most
insulin syringes have a disposable 27- to 29-gauge nee-dle that is
approximately 0.5 inch long. The smaller syringes are marked in 1-unit
increments and may be easier to use for patients with visual deficits or patients
taking very small doses of insulin. The 1-mL syringes are marked in 2-unit
increments. A small dis-posable insulin needle (29- to 30-gauge, 8 mm long) is
available for very thin patients and children.
PREPARING THE INJECTION: MIXING INSULINS
When
rapid- or short-acting insulins are to be given simultane-ously with
longer-acting insulins, they are usually mixed together in the same syringe;
the longer-acting insulins must be mixed thoroughly before use. There is some
question as to whether the two insulins are stable if the mixture is kept in
the syringe for more than 5 to 15 minutes. This may depend on the ratio of the
insulins as well as the time between mixing and injecting. When regular insulin
is mixed with long-acting insulin, there is a bind-ing reaction that slows the
action of the regular insulin. This may also occur to a greater degree when
mixing regular insulin with one of the Lente insulins. Patients are advised to
consult their health care provider for advice on this matter. The most impor-tant
issue is that patients be consistent in how they prepare their insulin
injections from day to day.
While
there are varying opinions regarding which type of insulin (short- or
longer-acting) should be drawn up into the syringe first when they are going to
be mixed, the ADA recom-mends that the regular insulin be drawn up first. The
most impor-tant issues are, again, that patients be consistent in technique so
as not to draw up the wrong dose accidentally or the wrong type of insulin, and
that patients not inject one type of insulin into the bottle containing a
different type of insulin (ADA, Insulin Administration, 2003).
For
patients who have difficulty mixing insulins, two options are available: they
may use a premixed insulin, or they may have prefilled syringes prepared.
Premixed insulins are available in sev-eral different ratios of NPH insulin to
regular insulin. The ratio of 70/30 (70% NPH and 30% regular insulin in one
bottle) is the most common and is available as Novolin 70/30 (Novo Nordisk) and
Humulin 70/30 (Lilly). Other ratios available in-clude 80/20, 60/40, and 50/50.
The ratio of 75% NPL and 25% insulin lispro is also available (ADA, Insulin
Administration, 2002). NPL is used only to mix with Humalog; its action is the
same as NPH. The appropriate initial dosage of premixed insulin must be
calculated so that the ratio of NPH to regular insulin most closely
approximates the separate doses needed.
For
patients who can inject insulin but who have difficulty drawing up a single or
mixed dose, syringes can be prefilled with the help of home care nurses or
family and friends. A 3-week supply of insulin syringes may be prepared and
kept in the refriger-ator. The prefilled syringes should be stored with the
needle in an upright position to avoid clogging of the needle (ADA, Insulin
Administration, 2003).
WITHDRAWING INSULIN
Most
(if not all) of the printed materials available on insulin dose preparation
instruct patients to inject air into the bottle of insulin equivalent to the
number of units of insulin to be withdrawn. The rationale for this is to
prevent the formation of a vacuum in-side the bottle, which would make it
difficult to withdraw the proper amount of insulin. Some nurses who specialize
in diabetes report that some patients (who have been taking insulin for many
years) have stopped injecting air before withdrawing the insulin. These
patients found that the extra step was not necessary for ac-curately drawing up
the insulin dose. Most patients find it easier to withdraw the insulin by
eliminating the step and report no dif-ficulty in preparing the proper insulin
dose.
Eliminating
this step (or alternating it by, for instance, inject-ing a syringe full of air
into the vial once per week) facilitates the teaching process for some patients
learning to draw up insulin for the first time. Some patients become confused
with the sequence of steps involved in injecting air into two separate bottles
in two different amounts before drawing up a mixed dose. For many in-dividuals,
including elderly ones, simplifying the procedure for preparing insulin
injections may help them maintain indepen-dence in daily living.
As
with other variations in insulin injection technique, the most important
factors are that the patient maintain consistency in the procedure and that the
nurse be flexible when teaching new patients or assessing the skills of
experienced patients.
SELECTING AND ROTATING THE INJECTION SITE
The
four main areas for injection are the abdomen, arms (poste-rior surface),
thighs (anterior surface), and hips (Fig. 41-7). In-sulin is absorbed faster in
some areas of the body than others. The speed of absorption is greatest in the
abdomen and decreases pro-gressively in the arm, thigh, and hip.
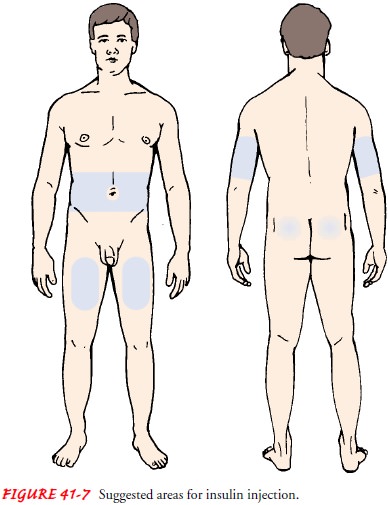
Systematic
rotation of injection sites within an anatomic area is recommended to prevent
localized changes in fatty tissue (lipodystrophy). In addition, to promote
consistency in insulin absorption, patients should be encouraged to use all
available in-jection sites within one area rather than randomly rotating sites
from area to area (ADA, Insulin Administration, 2002). For ex-ample, some
patients almost exclusively use the abdominal area, administering each
injection 0.5 to 1 inch away from the previ-ous injection. Another approach to
rotation is always to use the same area at the same time of day. For example,
patients may in-ject morning doses into the abdomen and evening doses into the
arms or legs.
A few
general principles apply to all rotation patterns. First, patients should try
not to use the same site more than once in 2 to 3 weeks. In addition, if the
patient is planning to exercise, in-sulin should not be injected into the limb
that will be exercised, because it will be absorbed faster, and this may result
in hypo-glycemia.
In the past, patients were taught to rotate injections from one area to the next (eg, injecting once in the right arm, then once in the right abdomen, then once in the right thigh). Patients who still use this system must be taught to avoid repeated injec-tions into the same site within an area. However, as previously stated, it is preferable for the patient to use the same anatomic area at the same time of day consistently; this reduces day-to-day variation in blood glucose levels because of different absorption rates.
PREPARING THE SKIN
Use of
alcohol to cleanse the skin is not recommended, but pa-tients who have learned
this technique often continue to use it. They should be cautioned to allow the
skin to dry after cleansing with alcohol. If the skin is not allowed to dry
before the injection, the alcohol may be carried into the tissues, resulting in
a localized reddened area.
INSERTING THE NEEDLE
There
are varying approaches to inserting the needle for insulin injections. The
correct technique is based on the need for the in-sulin to be injected into the
subcutaneous tissue. Injection that is too deep (eg, intramuscular) or too
shallow may affect the rate of absorption of the insulin. Aspiration (inserting
the needle and then pulling back on the plunger to assess for blood being drawn
into the syringe) is generally not recommended with self-injection of insulin.
Many patients who have been using insulin for an ex-tended period have
eliminated this step from their insulin injec-tion routine with no apparent
adverse effects.
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care.
Adherence to
the therapeutic planis the most important goal of self-care the patient must
master. Patients who are having difficulty adhering to the diabetes treatment
plan must be approached with care and understand-ing. Using scare tactics (such
as threats of blindness or ampu-tation if the patient does not adhere to the
treatment plan) or making
the patient feel guilty is not productive and may inter-fere with establishing
a trusting relationship with the patient. Judgmental actions, such as asking
the patient if he or she has “cheated” on the diet, only promote feelings of
guilt and low self-esteem.
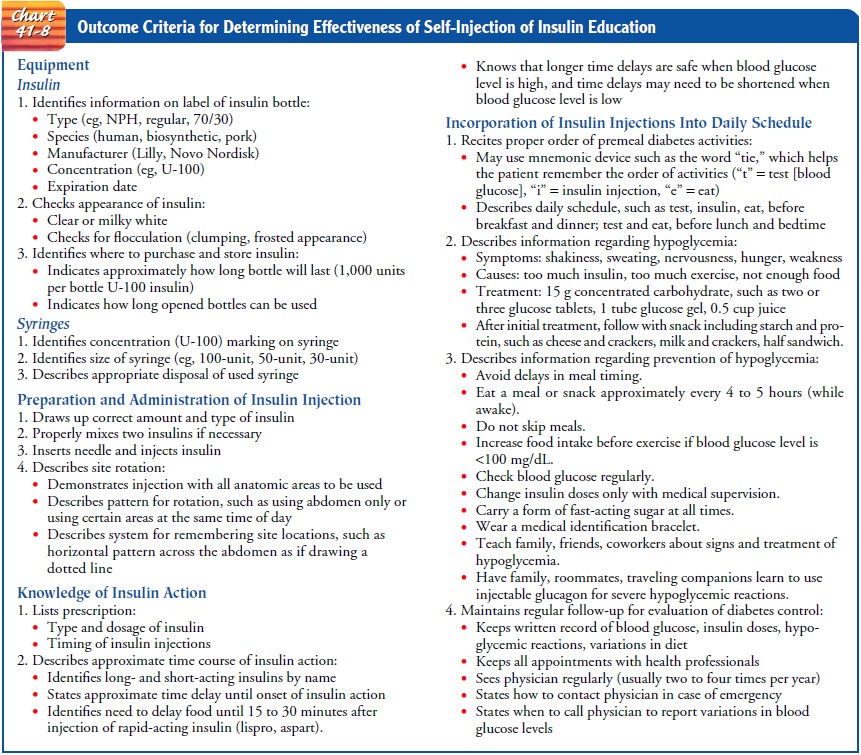
If
problems exist with glucose control or with the develop-ment of preventable
complications, it is important to distinguish among nonadherence, knowledge
deficit, and self-care deficit. It should not be assumed that problems with
diabetes management are related to nonadherence. The patient may simply have for-gotten
or never learned certain information. The problem may be correctable simply
through providing complete information and ensuring that the patient
comprehends the information. Chart 41-8 details how to evaluate the
effectiveness of self-injection of insulin.
If
knowledge deficit is not the problem, certain physical or emotional factors may
be impairing the patient’s ability to per-form self-care skills. For example,
decreased visual acuity may impair the patient’s ability to administer insulin
accurately, measure the blood glucose level, or inspect the skin and feet. In
addition, decreased joint mobility (especially in the elderly) im-pairs the
ability to inspect the bottom of the feet. Emotional factors such as denial of
the diagnosis or depression may impair the patient’s ability to carry out
multiple daily self-care mea-sures. In other circumstances, family, personal,
or work prob-lems may be of higher priority to the patient. The patient facing
competing demands for time and attention may benefit from assistance in
establishing priorities. It is also important to assess the patient for
infection or emotional stress that may lead to el-evated blood glucose levels
despite adherence to the treatment regimen.
The
following approaches by the nurse are helpful for pro-moting self-care
management skills:
•
Address any underlying factors (eg, knowledge
deficit, self-care deficit, illness) that may affect diabetic control.
•
Simplify the treatment regimen if it is too
difficult for the patient to follow.
•
Adjust the treatment regimen to meet patient
requests (eg, adjust diet or insulin schedule to allow increased flexi-bility
in meal content or timing).
•
Establish a specific plan or contract with the
patient with simple, measurable goals.
•
Provide positive reinforcement of self-care
behaviors per-formed instead of focusing on behaviors that were neglected (eg,
positively reinforce blood glucose tests that were per-formed instead of
focusing on the number of missed tests).
•
Help the patient to identify personal motivating
factors rather than focusing on wanting to please the doctor or nurse.
•
Encourage the patient to pursue life goals and
interests; dis-courage an undue focus on diabetes.
Continuing Care.
As discussed, continuing care of the patientwith diabetes is critical in managing and preventing complica-tions. The degree to which the client interacts with health care providers to obtain ongoing care depends on many factors. Age, socioeconomic level, existing complications, type of diabetes, and comorbid conditions all may dictate the frequency of follow-up vis-its. Many patients with diabetes may be seen by home health nurses for diabetic education, wound care, insulin preparation, or assistance with glucose monitoring. Even patients who achieve excellent glucose control and have no complications can expect to see their primary health care provider at least twice a year for ongoing evaluation.
In
addition to follow-up care with health professionals, par-ticipation in support
groups is encouraged for those who have had diabetes for many years as well as
those who are newly diag-nosed. Such participation may assist the patient and
family in coping with changes in lifestyle that occur with the onset of
diabetes and with its complications. Those who participate in support groups
often have an opportunity to share valuable in-formation and experiences and to
learn from others. Support groups provide an opportunity for discussion of
strategies to deal with diabetes and its management and to clarify and verify
infor-mation with the nurse or other health care professionals. Partici-pation
in support groups may help patients and their families to become more
knowledgeable about diabetes and its management and may promote adherence to the
management plan. Another very important role of the nurse is to remind the
patient about the importance of participating in other health promotion
activ-ities and recommended health screening.
Related Topics