Chapter: Medical Surgical Nursing: Assessment and Management of Patients With Diabetes Mellitus
Diabetes Management: Exercise
EXERCISE
Benefits
Exercise
is extremely important in managing diabetes because of its effects on lowering
blood glucose and reducing cardiovascular risk factors. Exercise lowers the
blood glucose level by increasing the uptake of glucose by body muscles and by
improving insulin utilization. It also improves circulation and muscle tone.
Resis-tance (strength) training, such as weight lifting, can increase lean
muscle mass, thereby increasing the resting metabolic rate. These effects are
useful in diabetes in relation to losing weight, easing stress, and maintaining
a feeling of well-being. Exercise also alters blood lipid levels, increasing
levels of high-density lipoproteins and decreasing total cholesterol and
triglyceride levels. This is es-pecially important to the person with diabetes
because of the in-creased risk of cardiovascular disease (Creviston &
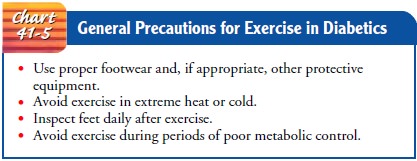
Quinn, 2001). General guidelines for exercise in diabetes are presented in
Chart 41-5.
Exercise Precautions
Patients
who have blood glucose levels exceeding 250 mg/dL (14 mmol/L) and who have
ketones in their urine should not begin exercising until the urine tests
negative for ketones and the blood glucose level is closer to normal.
Exercising with elevated blood glu-cose levels increases the secretion of
glucagon, growth hormone, and catecholamines. The liver then releases more
glucose, and the result is an increase in the blood glucose level (ADA,
Phys-ical Activity/Exercise and Diabetes Mellitus, 2003).
The physiologic decrease in circulating insulin that normally occurs with exercise cannot occur in patients treated with insulin. Initially, the patient who requires insulin should be taught to eat a 15-g carbohydrate snack (a fruit exchange) or a snack of com-plex carbohydrate with a protein before engaging in moderate ex-ercise, to prevent unexpected hypoglycemia. The exact amount of food needed varies from person to person and should be de-termined by blood glucose monitoring. Some patients find that they do not require a pre-exercise snack if they exercise within 1 to 2 hours after a meal. Other patients may require extra food re-gardless of when they exercise. If extra food is required, it need not be deducted from the regular meal plan.Another potential problem for patients who take insulin is hypoglycemia that occurs many hours after exercise. To avoid postexercise hypoglycemia, especially after strenuous or prolonged exercise, the patient may need to eat a snack at the end of the ex-ercise session and at bedtime and monitor the blood glucose level more frequently.
In addition, it may be necessary to have the pa-tient reduce the
dosage of insulin that peaks at the time of exer-cise. Patients who are
capable, knowledgeable, and responsible can learn to adjust their own insulin
doses. Others need specific instructions on what to do when they exercise.
Patients
participating in extended periods of exercise should test their blood glucose
levels before, during, and after the exercise pe-riod, and they should snack on
carbohydrates as needed to main-tain blood glucose levels (ADA, Physical
Activity/Exercise and Diabetes Mellitus, 2003). Other participants or observers
should be aware that the person exercising has diabetes, and they should know
what assistance to give if severe hypoglycemia occurs.
In
obese people with type 2 diabetes, exercise in addition to dietary management
both improves glucose metabolism and en-hances loss of body fat. Exercise
coupled with weight loss im-proves insulin sensitivity and may decrease the
need for insulin or oral agents. Eventually, the patient’s glucose tolerance
may return to normal. The patient with type 2 diabetes who is not taking
in-sulin or an oral agent may not need extra food before exercise.
Exercise Recommendations
People
with diabetes should exercise at the same time (preferably when blood glucose
levels are at their peak) and in the same amount each day. Regular daily
exercise, rather than sporadic exercise, should be encouraged. Exercise
recommendations must be altered as necessary for patients with diabetic
complications such as retinopathy, autonomic neuropathy, sensorimotor
neuropathy, and cardiovascular disease (ADA, Physical Activity/Exercise and
Dia-betes Mellitus, 2003). Increased blood pressure associated with ex-ercise
may aggravate diabetic retinopathy and increase the risk of a hemorrhage into
the vitreous or retina. Patients with ischemic heart disease risk triggering
angina or a myocardial infarction, which may be silent. Avoiding trauma to the
lower extremities is especially important in the patient with numbness related
to neuropathy.
In
general, a slow, gradual increase in the exercise period is en-couraged. For
many patients, walking is a safe and beneficial form of exercise that requires
no special equipment (except for proper shoes) and can be performed anywhere.
People with diabetes should discuss an exercise program with their physician
and un-dergo a careful medical evaluation with appropriate diagnostic studies
before beginning an exercise program (ADA, Physical Activity/Exercise and
Diabetes Mellitus, 2003; Creviston & Quinn, 2001; Flood & Constance,
2002).
For
patients who are older than 30 years and who have two or more risk factors for
heart disease, an exercise stress test is rec-ommended. Risk factors for heart
disease include hypertension, obesity, high cholesterol levels, abnormal
resting electrocardio-gram, sedentary lifestyle, smoking, male gender, and a
family his-tory of heart disease.
Gerontologic Considerations
Physical
activity that is consistent and realistic is beneficial to the elderly person
with diabetes. Physical fitness in the elderly popu-lation with diabetes may
lead to less chronic vascular disease and an improved quality of life (ADA,
Physical Activity/Exercise and Diabetes Mellitus, 2003). Advantages of exercise
in this popula-tion include a decrease in hyperglycemia, a general sense of
well-being, and the use of ingested calories, resulting in weight reduction.
Because there is an increased incidence of cardiovascu-lar problems in the
elderly, a pattern of gradual, consistent exer-cise should be planned that does
not exceed the patient’s physical capacity. Physical impairment from other
chronic diseases must also be considered. In some cases a physical therapy
evaluation may be warranted with the goal of determining exercises specific to
the patient’s needs and abilities. Tools such as the “Armchair Fitness” video
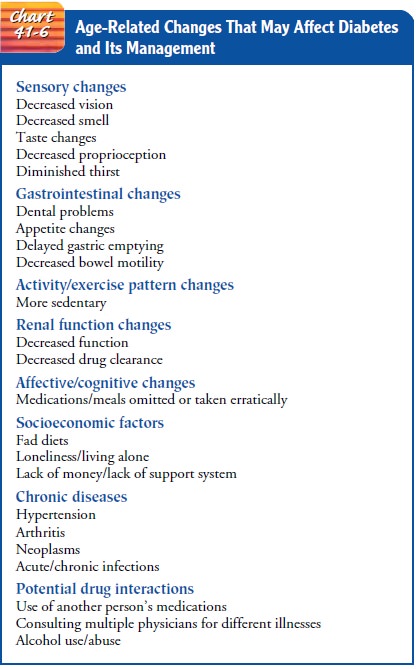
may be helpful. For more information about age-related changes that affect
diabetes management see Chart 41-6.
Related Topics