Chapter: Medical Surgical Nursing: Assessment and Management of Patients With Diabetes Mellitus
Foot and Leg Problems - Long Term Complications of Diabetes
FOOT
AND LEG PROBLEMS
From
50% to 75% of lower extremity amputations are performed on people with
diabetes. More than 50% of these amputations are thought to be preventable,
provided patients are taught foot care measures and practice them on a daily
basis (ADA, Preven-tive Foot Care in People With Diabetes, 2003). Complications
of diabetes that contribute to the increased risk of foot infections include:
• Neuropathy: Sensory neuropathy leads to
loss of pain and pressure sensation, and autonomic neuropathy leads to
in-creased dryness and fissuring of the skin (secondary to de-creased
sweating). Motor neuropathy results in muscular atrophy, which may lead to
changes in the shape of the foot.
• Peripheral vascular disease: Poor
circulation of the lower ex-tremities contributes to poor wound healing and the
devel-opment of gangrene.
• Immunocompromise: Hyperglycemia impairs
the ability of specialized leukocytes to destroy bacteria. Thus, in poorly
controlled diabetes, there is a lowered resistance to certain infections.
The typical sequence of events in the development of a dia-betic foot ulcer begins with a soft tissue injury of the foot, for-mation of a fissure between the toes or in an area of dry skin, or formation of a callus (Fig. 41-10). Injuries are not felt by the pa-tient with an insensitive foot and may be thermal (eg, from using heating pads, walking barefoot on hot concrete, or testing bath water with the foot), chemical (eg, burning the foot while using caustic agents on calluses, corns, or bunions), or traumatic (eg, injuring skin while cutting nails, walking with an undetected for-eign object in the shoe, or wearing ill-fitting shoes and socks).
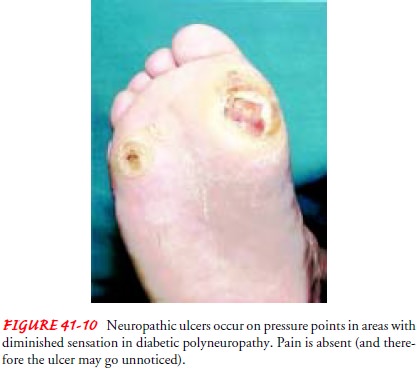
If the
patient is not in the habit of thoroughly inspecting both feet on a daily
basis, the injury or fissure may go unnoticed until a serious infection has
developed. Drainage, swelling, redness (from cellulitis) of the leg, or
gangrene may be the first sign of foot problems that the patient notices.
Treatment of foot ulcers involves bed rest, antibiotics, and débridement. In
addition, con-trolling glucose levels, which tend to increase when infections
occur, is important for promoting wound healing. In patients with peripheral
vascular disease, foot ulcers may not heal because of the decreased ability of
oxygen, nutrients, and antibiotics to reach the injured tissue. Amputation may
be necessary to prevent the spread of infection.
Foot
assessment and foot care instructions are most important when caring for
patients who are at high risk for developing foot infections. Some of the
high-risk characteristics include:
·
Duration of diabetes more than 10 years
·
Age older than 40 years
·
History of smoking
·
Decreased peripheral pulses
·
Decreased sensation
·
Anatomic deformities or pressure areas (eg,
bunions, calluses, hammer toes)
·
History of previous foot ulcers or amputation
Management
Teaching
patients proper foot care is a nursing intervention that can prevent costly,
painful, and debilitating complications. Pre-ventive foot care begins with
careful daily assessment of the feet. The feet must be inspected on a daily
basis for any redness, blis-ters, fissures, calluses, ulcerations, changes in
skin temperature, and the development of foot deformities (ie, hammer toes,
bunions). For patients with visual impairment or decreased joint mobility
(especially the elderly), use of a mirror to inspect the bottom of the feet or
the help of a family member in foot in-spection may be necessary. The interior
surfaces of shoes should be inspected for any rough spots or foreign objects.
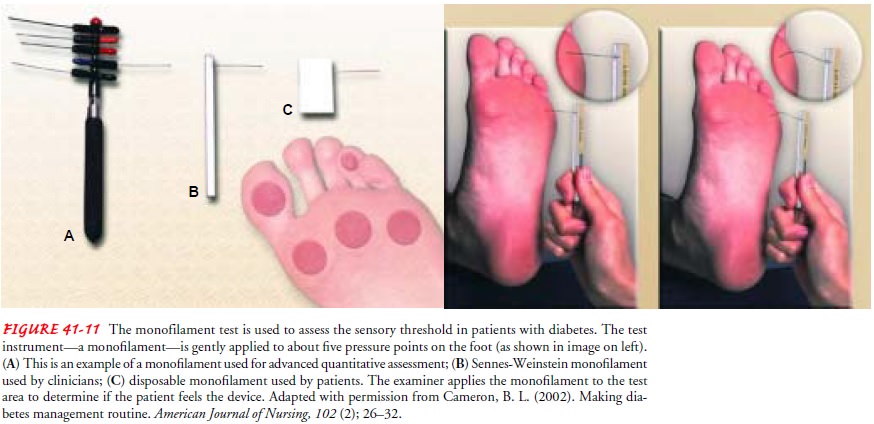
In
addition to the daily visual and manual inspection of the feet, the feet should
be examined during every health care visit or at least once per year (more
often if there is an increase in the pa-tient’s risk) by a podiatrist,
physician, or nurse (Fritschi, 2001). Patients with neuropathy should also
undergo evaluation of neuro-logic status using a monofilament device by an
experienced ex-aminer (Fig. 41-11). Patients with pressure areas, such as
calluses, or thick toenails should see the podiatrist routinely for treatment
of calluses and trimming of nails.
Additional
aspects of preventive foot care that are taught to the patient and family include
the following:
· Properly bathing,
drying, and lubricating the feet, taking care not to allow moisture (water or
lotion) to accumulate between the toes
· Wearing closed-toe shoes
that fit well. Podiatrists can pro-vide patients with inserts (orthotics) to
remove pressure from pressure points on the foot. New shoes should be bro-ken
in slowly (ie, worn for 1 to 2 hours initially, with grad-ual increases in the
length of time worn) to avoid blister formation. Patients with bony deformities
may need extra-wide shoes or extra-depth shoes. High-risk behaviors should be
avoided, such as walking barefoot, using heating pads on the feet, wearing
open-toed shoes, soaking the feet, and shaving calluses.
· Trimming toenails
straight across and filing sharp corners to follow the contour of the toe
(American Association of Diabetes Educators, 1998). If patients have visual
deficits or thickened toenails, a podiatrist should cut the nails.
· Reducing risk factors,
such as smoking and elevated blood lipids, that contribute to peripheral
vascular disease
· Avoiding home remedies
or over-the-counter agents or self-medicating to treat foot problems (Fritschi,
2001)
Blood
glucose control is important for avoiding decreased re-sistance to infections
and for preventing diabetic neuropathy. The patient may be referred by the
physician to a wound care center for managing persistent wounds of the feet or
legs. Many wound care centers provide diabetes education; however, the patient
needs to discuss recommendations for treating wounds with his or her own
physician, as well as raising any questions about diabetes management.
Related Topics