Chapter: Clinical Anesthesiology: Regional Anesthesia & Pain Management: Chronic Pain Management
Cervical, Thoracic & Lumbar Medial Branch Blocks
Cervical, Thoracic,& Lumbar Medial Branch Blocks
A. Indications
These blocks may be utilized in patients with back pain to assess the
contribution of lumbar facet (zyg-apophyseal) joint disease. Corticosteroids
are com-monly injected with the local anesthetic when the intraarticular
technique is chosen. The cervical, tho-racic, or lumbar facet joints may be
injected for diag-nostic and potentially therapeutic purposes.
B. Anatomy
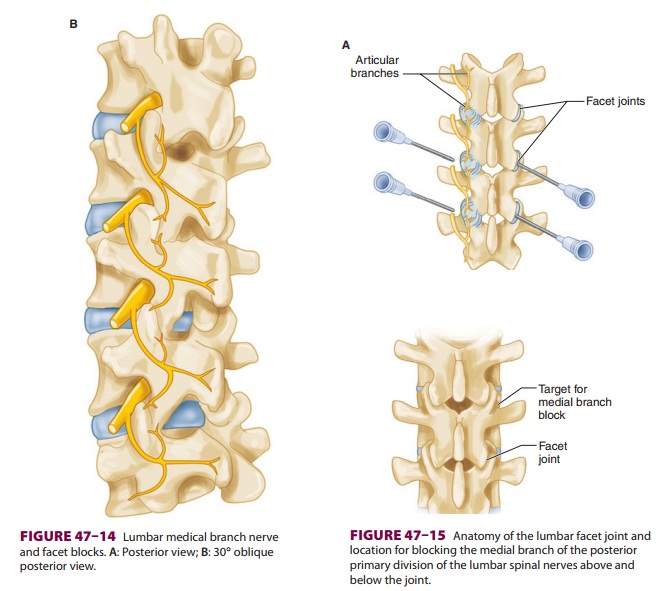
Each facet joint is innervated by the medial
branches of the posterior primary division of the spinal nerves above and below
the joint (Figure 47–14). Thus,
every joint is supplied by two or more adjacent spi-nal nerves. Each
medial branch crosses the upper border of the lower transverse process running
in a groove between the root of the transverse process and the superior
articular process.
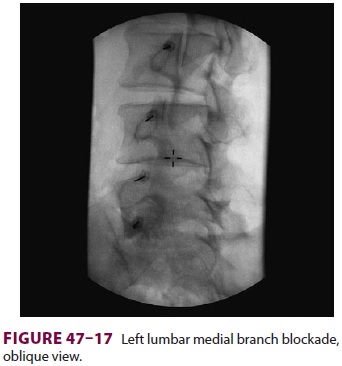
C. Technique
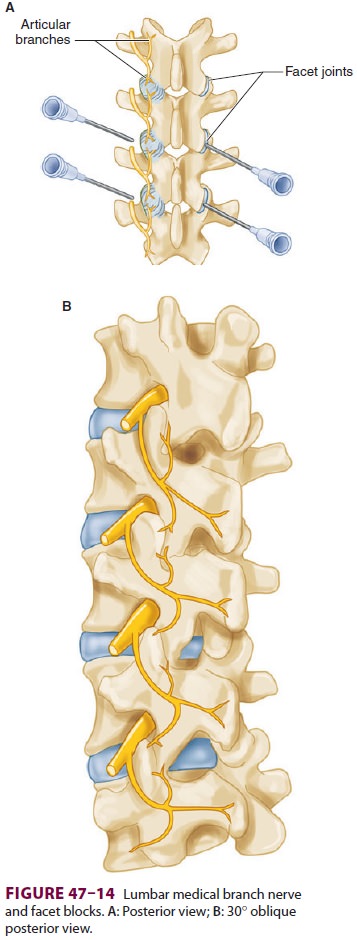
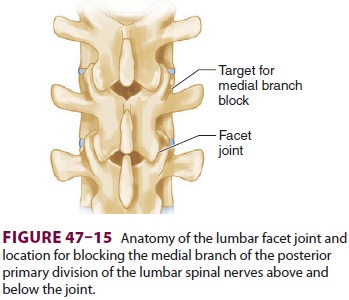
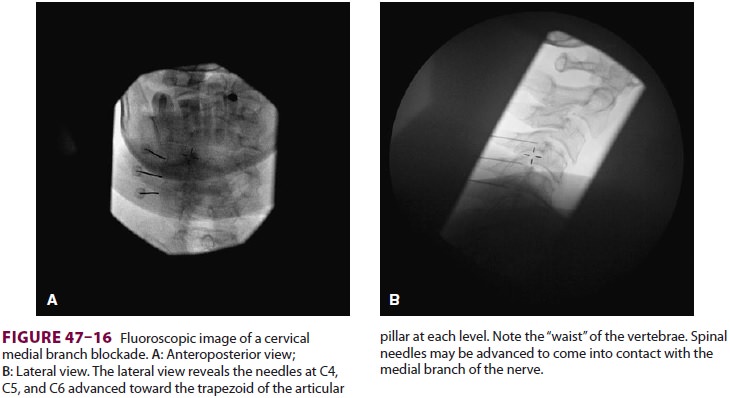
These blocks are performed under fluoroscopic
guidance with the patient in a prone position, or in some cases, the lateral
position for cervical proce-dures. A posterior–anterior view facilitates
visualiza-tion of the spine for lumbar medial branch blocks. A 10-cm 22-gauge
needle is inserted 3–4 cm lateral to the spinous process at the desired level
and directed anteriorly toward the junction of the transverse pro-cess and the
superior articular process to block the medial branch of the posterior division
of the spinal nerve (Figures 47–15
through 47–17).Alternatively, local anesthetic with or
without corticosteroid may be directly injected into the facet joint.
Positioning the patient prone and using an oblique fluoroscopic view
facilitates identification of the joint space. Correct placement of the needle
may be confirmed by injecting radiopaque contrast prior to injection of local
anesthetic. Total injection volumes should ideally be limited to less than 1 mL
in order to prevent rupture of the joint capsule.
D. Complications
Injection into a dural sleeve results in a subarach-noid block, whereas injection near the spinal nerve root results in sensory and motor block at that level. Because the joint normally has a small volume, larger injections can cause rupture of the joint capsule.
If a patient achieves improved pain control after a diagnostic block, he or she may be considered for radiofrequency ablation of the medial branch. There is debate about whether a second, confirma-tory diagnostic block should be performed prior to radiofrequency ablation. Injection of steroid may be considered before or after radiofrequency abla-tion to theoretically decrease the chance for post-procedural neuritis.
Related Topics