Chapter: Clinical Anesthesiology: Regional Anesthesia & Pain Management: Chronic Pain Management
Pathophysiology of Chronic Pain
PATHOPHYSIOLOGY OF CHRONIC PAIN
Chronic pain may be caused by a combina-tion of peripheral, central, and
psychological mechanisms. Sensitization of nociceptors plays a major role in
the origin of pain associated with peripheral mechanisms, such as chronic
musculo-skeletal and visceral disorders.
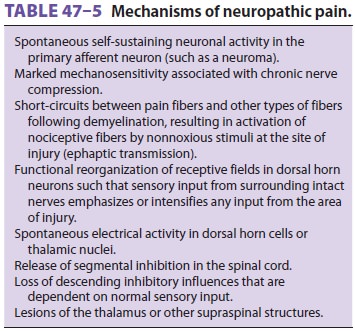
Neuropathic pain involves peripheral–central
and central neural mechanisms that are complex and generally associated with
partial or complete lesions of peripheral nerves, dorsal root ganglia, nerve
roots, or more central structures (Table 47–5).
Peripheral mechanisms include spontaneous dis-charges; sensitization of
receptors to mechanical, thermal, and chemical stimuli; and up-regulation of
adrenergic receptors. Neural inflammation may also be present. Systemic
administration of local anesthetics and anticonvulsants has been shown to
suppress the spontaneous firing of sensitized or traumatized neurons. This
observation is supported by the efficacy of agents such as lidocaine,
mexi-letine, and carbamazepine in many patients with neuropathic pain. Central
mechanisms include loss of segmental inhibition, wind-up of WDR neurons,
spontaneous discharges in deafferentated neurons, and reorganization of neural
connections.
The sympathetic nervous system appears to play a major role in some
patients with chronic pain. The efficacy of sympathetic nerve blocks in some of
these patients supports the concept of sympa-thetically maintained pain.
Painful disorders that often respond to sympathetic blocks include com-plex
regional pain syndrome, deafferentation syn-dromes due to nerve avulsion or
amputations, and postherpetic neuralgia. However, the simplistic theory of
heightened sympathetic activity resulting in vasoconstriction, edema, and
hyperalgesia fails to account for the warm and erythematous phase observed in
some patients. Similarly, clinical and experimental observations do not satisfactorily
sup-port the theory of ephaptic transmission between pain fibers and
demyelinated sympathetic fibers.
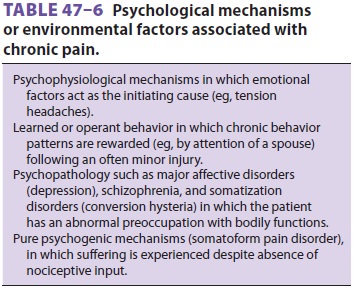
Psychological mechanisms or environmental factors are rarely the sole
mechanisms for chronic pain but are commonly seen in combination with other
mechanisms (Table 47–6).
Related Topics