Chapter: Medical Surgical Nursing: Assessment and Management of Patients With Hepatic Disorders
Management of Patients With Hepatitis A Virus (HAV)
HEPATITIS
A VIRUS (HAV)
HAV accounts for 20% to 25% of cases of clinical hepatitis in the developed world. Hepatitis A, formerly called infectious hepatitis, is caused by an RNA virus of the Enterovirus family. The mode of transmission of this disease is the fecal–oral route, primarily through the ingestion of food or liquids infected by the virus. The virus has been found in the stool of infected patients before the onset of symptoms and during the first few days of illness. Typi-cally, a child or a young adult acquires the infection at school by poor hygiene, hand-to-mouth contact, or close contact at play. The virus is carried home, where haphazard sanitary habits spread it through the family. It is more prevalent in developing countries or in areas with overcrowding and poor sanitation. An infected food handler can spread the disease, and people can contract it by consuming water or shellfish from sewage-contaminated waters. Outbreaks have occurred in day care centers and institutions for the developmentally delayed because of lapses in hygiene. It is rarely, if ever, transmitted by blood transfusions. Hepatitis A can be transmitted during sexual activity; this is more likely with oral–anal contact, anal intercourse, and a greater number of sex partners (CDC, 2002).
The
incubation period is estimated to be 15 to 50 days, with an average of 30 days
(O’Grady et al., 2000). The illness may be prolonged, lasting 4 to 8 weeks. It
generally lasts longer and is more severe in those older than 40 years of age.
Recovery is the rule; hepatitis A rarely progresses to acute liver necrosis or
fulmi-nant hepatitis, terminating in cirrhosis of the liver or death. Hepatitis
A confers immunity against itself, but the person may contract other forms of
hepatitis. The mortality rate of hep-atitis A is approximately 0.5% for those
under 40 years of age and increases to 1% to 2% for those over 40. No carrier
state exists, and no chronic hepatitis is associated with hepatitis A. The
virus is present only briefly in the serum; by the time jaundice occurs, the
patient is likely to be noninfectious (O’Grady et al., 2000).
Clinical Manifestations
Many
patients are anicteric (without jaundice) and symptomless. When symptoms
appear, they are of a mild, flu-like upper respi-ratory tract infection, with
low-grade fever. Anorexia, an early symptom, is often severe. It is thought to
result from release of a toxin by the damaged liver or by failure of the
damaged liver cells to detoxify an abnormal product. Later, jaundice and dark
urine may become apparent. Indigestion is present in varying degrees, marked by
vague epigastric distress, nausea, heartburn, and flat-ulence. The patient may
also develop a strong aversion to the taste
of cigarettes or the presence of cigarette smoke and other strong odors.
These symptoms tend to clear as soon as the jaundice reaches its peak, perhaps
10 days after its initial appearance. Symptoms may be mild in children; in
adults, the symptoms may be more severe and the course of the disease
prolonged.
Assessment and Diagnostic Findings
The
liver and spleen are often moderately enlarged for a few days after onset;
otherwise, apart from jaundice, there are few physical signs. Hepatitis A
antigen may be found in the stool a week to 10 days before illness and for 2 to
3 weeks after symptoms appear. HAV antibodies are detectable in the serum, but
usually not until symptoms appear. Analysis of subclasses of immunoglobulins
can help determine whether the antibody represents acute or past infection.
Prevention
A
number of strategies exist to prevent transmission of HAV. Patients and their
families need to be made aware of these and encouraged to consider them if
recommended by their primary health care provider.
In
February 1995, the Food and Drug Administration ap-proved the first vaccine
against hepatitis A for use in the United States. Effective and safe HAV
vaccines include Havrix and Vagta (Koff, 2001). It is recommended that the
two-dose vac-cine be given to adults 18 years of age or older, with the second
dose 6 to 12 months after the first. Protection against hepatitis A develops
within several weeks after the first dose of the vac-cine. Children and
adolescents 2 to 18 years of age receive three doses, with the second dose 1 month
after the first and the third dose 6 to 12 months later. It is estimated that
protection against hepatitis A may last for at least 20 years (CDC, 1999). No
country has as yet recommended universal vaccination against hepatitis A.
Hepatitis A vaccine is recommended for travelers to locations where sanitation
and hygiene are unsatisfactory. Vac-cination is also recommended for those from
other high-risk groups (homosexual men, injection/intravenous drug users, staff
of day care centers, and health care personnel) (CDC, 2002). The vaccine has
also been used to interrupt community-wide out-breaks. As with other
vaccinations, precautions must be taken to ensure prevention, detection, and
treatment of hypersensitivity reactions to the vaccine.
Type A
hepatitis can be prevented in those not previously vaccinated by the
intramuscular administration of globulin dur-ing the incubation period, if
given within 2 weeks of exposure. This bolsters the person’s antibody
production and provides 6 to 8 weeks of passive immunity. Immune globulin may
suppress overt symptoms of the disease; the resulting subclinical case of
hepatitis A would produce active immunity to subsequent episodes of the virus.
Immune
globulin is also recommended for household members and sexual contacts of
people with hepatitis A. Susceptible people in the same household as the
patient are usually also infected by the time the diagnosis is made and should
receive immune globulin. Day care center and restaurant workers with exposure
to or infected with hepatitis A should also receive immune globulin to provide
passive immunity (CDC, 1999). Although rare, systemic reactions to immune
globulin may occur. Caution is required when anyone who has previously had
angioedema, hives, or other allergic reac-tions is treated with any human
immune globulin. Epinephrine should be available in case a systemic,
anaphylactic reaction occurs.
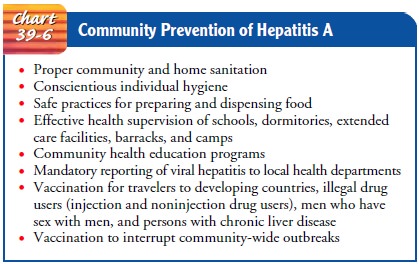
Preexposure
prophylaxis is recommended for those traveling to developing countries and
settings with poor or uncertain sanita-tion conditions but who do not have
sufficient time to acquire protection by administration of hepatitis A vaccine
(CDC, 1999). Community interventions for preventing hepatitis A are outlined in
Chart 39-6.
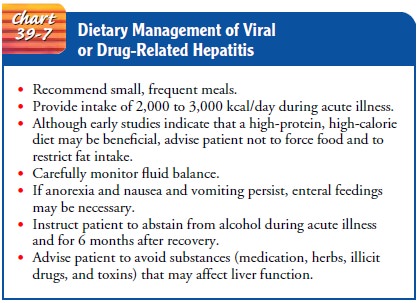
Medical Management
Bed rest
during the acute stage and a diet that is both acceptable to the patient and
nutritious are part of the treatment and nurs-ing care. During the period of
anorexia, the patient should receive frequent small feedings, supplemented, if
necessary, by IV fluids with glucose. Because this patient often has an
aversion to food, gentle persistence and creativity may be required to
stimulate the appetite. Optimal food and fluid levels are necessary to
counter-act weight loss and slow recovery. Even before the icteric phase,
however, many patients recover their appetites (Chart 39-7).
The
patient’s sense of well-being as well as laboratory test re-sults are generally
appropriate guides to bed rest and restriction of physical activity. Gradual
but progressive ambulation seems to hasten recovery, provided the patient rests
after activity and does not participate in activities to the point of fatigue.
Nursing Management
The patient is usually managed at home unless symptoms are se-vere. Therefore, the nurse assists the patient and family in coping with the temporary disability and fatigue that are common in hepatitis and instructs them to seek additional health care if the symptoms persist or worsen.
The patient and family also need specific guidelines about
diet, rest, follow-up blood work, and the importance of avoiding alcohol, as
well as sanitation and hygiene measures (particularly hand washing) to prevent
spread of the disease to other family members.
Specific
teaching to patients and families about reducing the risk of contracting
hepatitis A includes good personal hygiene, stressing careful hand washing
(after bowel movements and be-fore eating), and environmental sanitation (safe
food and water supply, as well as effective sewage disposal).
Related Topics