Chapter: Clinical Dermatology: Infections
Viral infections: Viral warts
Viral infections
The
viral infections dealt with here are those that are commonly seen in
dermatology clinics. A textbook of infectious diseases should be consulted for
details of systemic viral infections, many of which, like measles and German
measles, have their own specific rashes.
Viral warts
Most
people will have a wart at some time in their lives. Their prevalence is
highest in childhood, and they affect an estimated 4 ŌĆō5% of schoolchildren in
the UK.
Cause
Warts are caused by the human papilloma virus (HPV), which has still not been cultured in vitro.
Nevertheless, more
than 70 ŌĆśtypesŌĆÖ of the virus have been recognized by DNA sequencing; each has
its own range of clin-ical manifestations. HPV-1, 2 and 4, for example, are
found in common warts, whereas HPV-3 is found in plane warts, and HPV-6, 11, 16
and 18 are most common in genital warts. Infections occur when wart virus in
skin scales comes into contact with breaches in the skin or mucous membranes.
Presentation
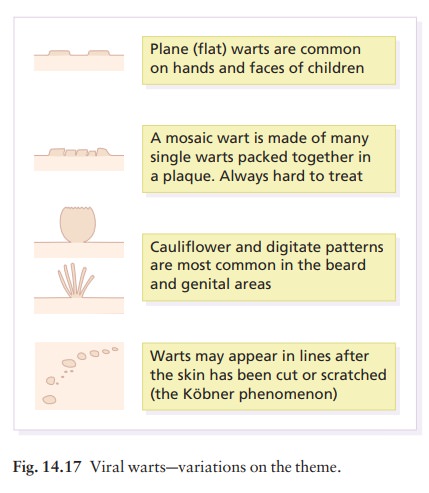
Warts
adopt a variety of patterns (Fig. 14.17), some of which are described below.
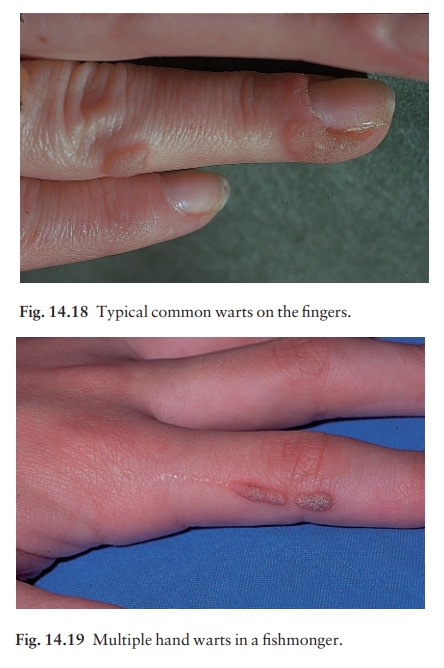
Common
warts (Figs 14.18 and 14.19). The first signis a smooth
skin-coloured papule, often more easily felt than seen. As the lesion enlarges,
its irregular hyper-keratotic surface gives it the classic ŌĆśwartyŌĆÖ appearance.
Common warts usually occur on the hands but are also often on the face and genitals.
They are more often multiple than single. Pain is rare.
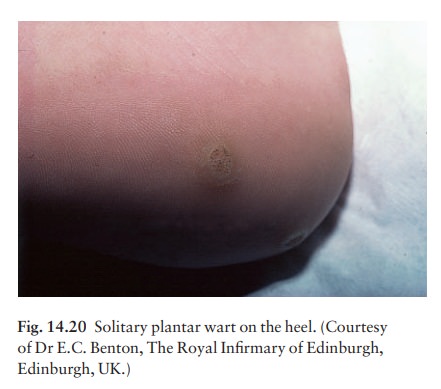
Plantar warts. These have a rough surface, which pro-trudes only slightly from the skin and is surrounded by a horny collar (Fig. 14.20). On paring, the presence of bleeding capillary loops allows plantar warts to be distinguished from corns. Often multiple, plantar warts can be painful.
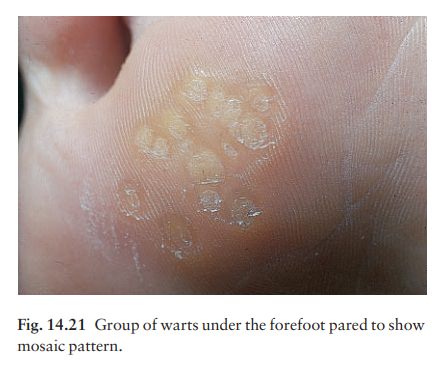
Mosaic
warts (Fig. 14.21). These rough marginatedplaques are made up of
many small tightly packed but discrete individual warts. They are most common
on the soles but are also seen on palms and around fingernails. Usually they
are not painful.
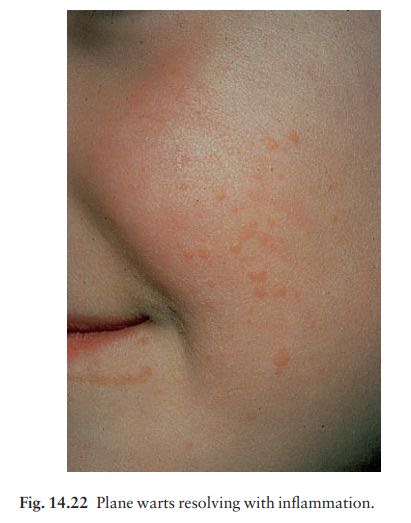
Plane warts (Fig. 14.22). These smooth flat-toppedpapules are most common on the face and brow, and on the backs of the hands. Usually skin-coloured or light brown, they become inflamed as a result of an immunological reaction, just before they resolve spontaneously. Lesions are multiple, painless and, like common warts, are sometimes arranged along a scratch line.
Facial
warts. These are most common in the beardarea of adult males and
are spread by shaving. A digitate appearance is common. Lesions are often ugly
but are painless.
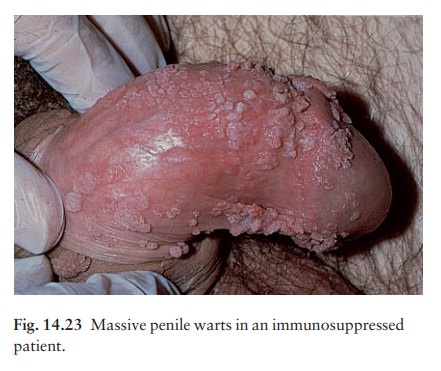
Anogenital
warts (condyloma acuminata) (Fig. 14.23).Papillomatous
cauliflower-like lesions, with a moist macerated vascular surface, can appear
anywhere in this area. They may coalesce to form huge lesions causing
discomfort and irritation. The vaginal and anorectal mucosae may be affected. The
presence of anogenital warts in children raises the spectre of sexual abuse,
but is usually caused by autoinoculation from common warts elsewhere.
Course
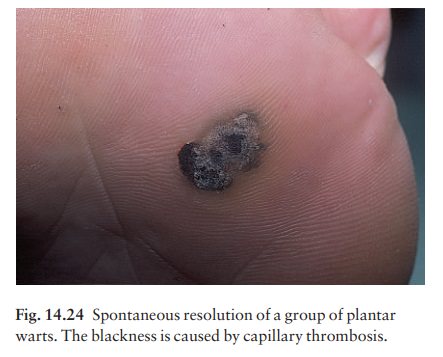
Warts resolve spontaneously in the healthy as the immune response overcomes the infection. This hap-pens within 6 months in some 30% of patients, and within 2 years in 65%. Such spontaneous resolution, sometimes heralded by a punctate blackening caused by capillary thrombosis (Fig. 14.24), leaves no trace. Mosaic warts are notoriously slow to resolve and often resist all treatments. Warts persist and spread in immunocompromised patients (e.g. those on immuno-suppressive therapy or with lymphoreticular disease).
Seventy
per cent of renal allograft recipients will have warts 5 years after
transplantation.
Complications
1 Some
plantar warts are very painful.
2 Epidermodysplasia
verruciformis is a rare inherited disorder in which there is a universal wart
infection, usually with HPV of unusual types. An impairment of cell-mediated
immunity is commonly found and ensuing
carcinomatous change frequently occurs. 3
Malignant change is otherwise rare, although infec-tions with HPV of
certain genital strains predispose to cervical and penile carcinoma. HPV
infections in immunocompromised patients (e.g. renal allograft recipients) have
also been linked with skin cancer, especially on light-exposed areas.
Differential diagnosis
Most
warts are easily recognized. The following must be ruled out.
ŌĆó
Molluscum contagiosum are
smooth,dome-shaped and pearly, with central umbilication.
ŌĆó
Plantar corns are found on pressure areas; there
isno capillary bleeding on paring. They have a central keratotic core and are
painful.
ŌĆó
Granuloma annulare lesions have a smoothsurface, as the lesions are
dermal; and their outline is often annular.
Condyloma
lata are seen in syphilis. They are rarebut should not be
confused with condyloma acuminata (warts). The lesions are flatter, greyer and
less well defined. If in doubt, look for other signs of secondary syphilis and
carry out serological tests.
ŌĆó
Amelanotic melanomas and other epithelial malig-nancies can
present as verrucose nodulesathose inpatients over the age of 40 years should
be examined with special care. Mistakes have been made in the past.
Treatment
Many
warts give no trouble, need no treatment and will go away by themselves.
Otherwise treatment will depend on the type of wart. In general terms,
destruc-tion by cryotherapy is less likely to cause scars than excision or
electrosurgery.
Palmoplantar warts
Home
treatment is best, with one of the many wart paints now available. Most contain
salicylic acid (12ŌĆō20%). The success rate is good if the patient is prepared to
persist with regular treatment. Paints should be applied once daily, after
moistening the warts in hot water for at least 5 min. After drying, dead tissue
and old paint are removed with an emery board or pumice stone. Enough paint to
cover the surface of the wart, but not the surround-ing skin, is applied and
allowed to dry. Warts on the plantar surface should be covered with plasters
although this is not necessary elsewhere. Side-effects are rare if these
instructions are followed. Wart paints should not be applied to facial or
anogenital skin, or to patients with adjacent eczema.
If
no progress is being made after the regular and correct use of a salicylic acid
wart paint for 12 weeks, then a paint containing formaldehyde or glutaraldehyde
is worth trying. A useful way of dealing with multiple small plantar warts is for
the area to be soaked for 10 min each night in a 4% formalin solution, although
a few patients become allergic to this.
Cryotherapy with liquid nitrogen (at ŌĆō196┬░C) is more effective than the less cold, dry ice or dimethyl ether/propane techniques. However, it is painful. A cotton-tipped applicator dipped into liquid nitrogen is applied to the wart until a small frozen halo appears in the surrounding normal skin (Fig. 14.25). The human papilloma virus, and also other viruses such as HIV, can survive in stored liquid nitrogen and so, once used, a bud should not be dipped back into the flask. Treatment with a liquid nitrogen spray gun does not increases the clearance rate of plantar warts but not of hand warts.
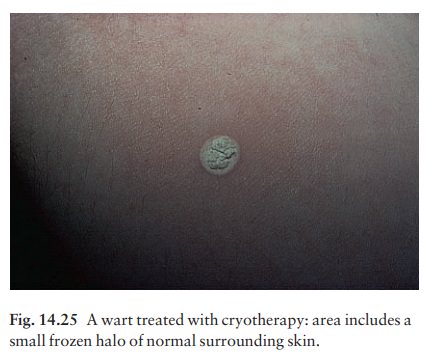
If further
treatments are necessary, the optimal interval is 3 weeks. The cure rate is
higher if plantar warts are pared before they are frozen, but this makes no
difference to warts elsewhere. If there has been no improvement after four or
five treatments there is little to be gained from further freezings.
A
few minutes tuition from a dermatologist will help practitioners wishing to
start cryotherapy. Blisters should not be provoked intentionally, but occur
from time to time, and will not alarm patients who have been forewarned.
Anogenital warts
Women
with anogenital warts, or who are the part-ners of men with anogenital warts,
should have their cervical cytology checked regularly as the wart virus can
cause cervical cancer.
The
focus has shifted towards self-treatment using podophyllotoxin (0.5% solution
or 0.15% cream) or imiquimod (5% cream). Both are irritants and should be used
carefully according to the manufacturerŌĆÖs instruc-tions. Imiquimod is an immune
response modifier that induces keratinocytes to produce cytokines, leading to
wart regression, and may help to build cell-mediated immunity for longlasting
protection. It is applied as a thin layer three times weekly and washed off
with a mild soap 6ŌĆō10 h after application. Podophyllin paint (15%) is used much
less often now. It should be applied carefully to the warts and allowed to dry
before powdering with talcum. On the first occasion it should be washed off
with soap and water after 2 h but, if there has been little discomfort, this
can be increased stepwise to 6 h. Treatment is best carried out weekly by a
doctor or nurse, but not by the pati-ent. Podophyllin must not be used in
pregnancy. Cryotherapy, electrosurgery and laser treatment are all effective
treatments in the clinic.
Facial common warts
These
are best treated with electrocautery or a hyfrecator, but also surrender to
careful cryotherapy. Scarring is an unwanted complication. Shaving, if
essential, should be with a brushless foam and a dis-posable razor.
Plane warts
On
the face these are best left untreated and the patient or parent can be
reasonably assured that spontaneous resolution will occur. When treatment is
demanded, the use of a wart paint or imiquimod cream is reason-able. Gentle
cryotherapy of just a few warts may help to induce immunity.
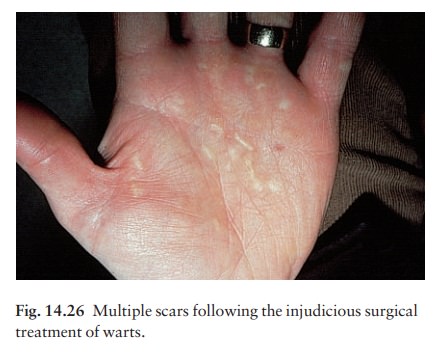
Solitary, stubborn or painful warts
These
can be removed under local anaesthetic with a curette, although cure is not
assured with this or any other method, and a scar often follows. Surgical
excision is never justifiable (Fig. 14.26). Bleomycin can also be injected into
such warts with success but this treatment should only be undertaken by a
specialist.
Related Topics