Chapter: Clinical Dermatology: Infections
Pityriasis versicolor
Pityriasis
versicolor
Cause
The
old name, tinea versicolor, should be dropped as the disorder is caused by
commensal yeasts (Pityro-sporum orbiculare) and not
by dermatophyte fungi.Overgrowth of these yeasts, particularly in hot humid
conditions, is responsible for the clinical lesions.
Carboxylic
acids released by the organisms inhibit the increase in pigment production by
melanocytes that occurs normally after exposure to sunlight. The term
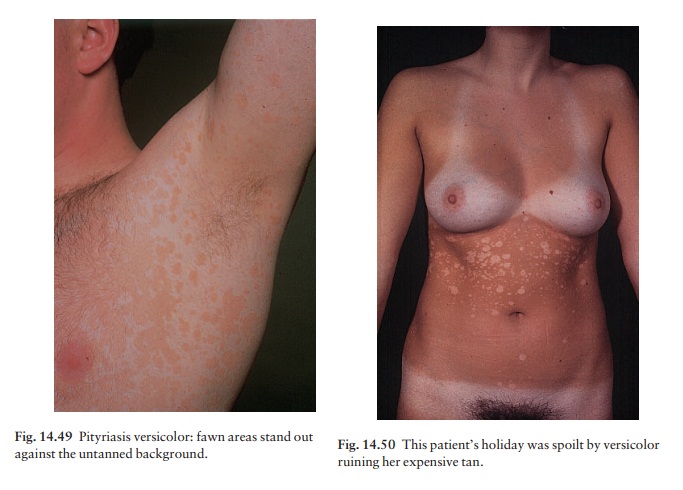
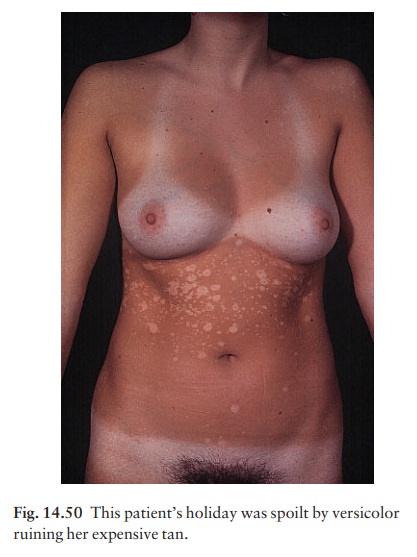
ŌĆśversicolorŌĆÖ refers to the way in which the super-ficial scaly patches, fawn or
pink on non-tanned skin (Fig. 14.49), become paler than the surrounding skin
after exposure to sunlight (Fig. 14.50). The condition should be regarded as
non-infectious.

Presentation and course
The fawn or depigmented areas, with their slightly branny scaling and fine wrinkling, look ugly. Other- wise they are symptom-free or only slightly itchy. Lesions are most common on the upper trunk but can become widespread. Untreated lesions persist, and depigmented areas, even after adequate treatment, are slow to regain their former colour. Recurrences are common.
Differential diagnosis
In
vitiligo, the border is clearly defined, scal-ing is absent, lesions are
larger, the limbs and face are often affected, and depigmentation is more
complete; however, it may sometimes be hard to distinguish vitiligo from the
pale non-scaly areas of treated versi-color. Seborrhoeic eczema of the trunk
tends to be more erythematous, and is often confined to the presternal or
interscapular areas. Pityriasis alba often affects the cheeks. Pityriasis
rosea, tinea corporis, secondary syphilis and erythrasma seldom cause real confusion.
Investigations
Scrapings,
prepared and examined as for a dermato-phyte infection, show a mixture of short
branched hyphae and spores (a ŌĆśspaghetti and meat-ballsŌĆÖ appearance). Culture
is not helpful.
Treatment
A
topical preparation of one of the imidazole group of antifungal drugs
(Formulary 1) can be applied at night to all affected areas for 2ŌĆō 4 weeks.
Equally effective, but messier and more irritant, is a 2.5% selenium sulphide
mixture in a detergent base (Selsun shampoo). This should be lathered on to the
patches after an evening bath, and allowed to dry. Next morning it should be
washed off. Three applica-tions at weekly intervals are adequate. A shampoo
containing ketoconazole is now available (Formulary 1) and is less messy, but
just as effective as the selenium ones. Alternatively, selenium sulphide lotion
(USA) can be applied for 10 min, rinsed off and re-applied daily for 1 week.
For widespread or stub-born infections systemic itraconazole (200 mg daily for
7 days) has been shown to be curative, but interac-tions with other drugs must
be avoided (Formulary 2). Recurrence is common after any treatment.
Related Topics