Chapter: Clinical Dermatology: Infections
Mycobacterial infections
Mycobacterial
infections
Tuberculosis
Most
infections in the UK are caused by Mycobac-terium tuberculosis.
Mycobacterium bovis infection,endemic in cattle, can be
spread to humans by milk, but human infection with this organism is now rare in
countries where cattle have been vaccinated against tuberculosis and the milk
is pasteurized. The steady decline of tuberculosis in developed countries has
been reversed in some areas where AIDS is especially prevalent. Dormant
tuberculosis of the skin can also be reactivated by systemic corticosteroids,
immuno-suppresants and new anti TNF biological agents.
Inoculation tuberculosis
Lupus vulgaris (Fig. 14.8) can follow the inoculation of tubercle bacilli into the skin of a person with high immunity, the direct spread of the organism from an underlying infected lymph node, or blood-borne spread from a pulmonary lesion. Lesions occur most often around the head and neck. A reddish-brown scaly plaque slowly enlarges, and can damage deeper tissues such as cartilage, leading to ugly mutilation. Scarring and contractures may follow.
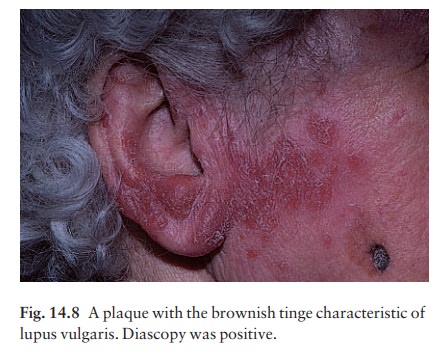
Diascopy shows up the characteristic brownish ŌĆśapple
jellyŌĆÖ nodules and the clinical dia-gnosis should be confirmed by a biopsy. A
warty variant exists.
Scrofuloderma
The
skin overlying a tuberculous lymph node or joint may become involved in the
process. The subsequent mixture of lesions (irregular puckered scars, fistulae
and abscesses) is most commonly seen in the neck.
Tuberculides
A
number of skin eruptions have, in the past, been attributed to a reaction to
internal foci of tuberculosis. Of these, the best authenticatedaby finding
mycobac-terial DNA by polymerase chain reaction (PCR)a are the ŌĆśpapulonecrotic
tuberculidesŌĆÖarecurring crops of firm dusky papules, which may ulcerate,
favouring the points of the knees and elbows.
Erythema induratum (BazinŌĆÖs disease)
In
erythema induratum, deep purplish ulcerating nodules occur on the backs of the
lower legs, usually in women with a poor ŌĆśchilblainŌĆÖ type of circulation.
Sometimes this is associated with a tuberculous focus elsewhere. Erythema
nodosum may also be the result of
tuberculosis elsewhere.
Investigations
Biopsy
for:
ŌĆó
microscopy (tuberculoid granulomas);
ŌĆó
bacteriological culture; and
ŌĆó
detection of mycobacterial DNA by
PCR. Mantoux test.
Treatment
The
treatment of all types of cutaneous tuberculosis should be with a full course
of a standard multidrug antituberculosis regimen. There is no longer any excuse
for the use of one drug alone.
Prevention
Outbreaks
of pulmonary tuberculosis are reminders that this disease has not yet been
conquered and that vigilance is important. Bacillus CalmetteŌĆōGu├®rin (BCG)
vaccination of schoolchildren, immunization of cattle and pasteurization of
milk remain the most effective protective measures.
Leprosy
Cause
Mycobacterium
leprae was discovered by Hansen in1874, but has still not been
cultured in
vitro, although it can be made to grow in some animals
(armadillos, mouse foot-pads, etc.). In humans the main route of infection is
through nasal droplets from cases of lepro-matous leprosy although,
interestingly, some cases have occurred in Louisiana from eating infected
armadillos.
Epidemiology
Some
15 million people suffer from leprosy. Most live in the tropics and subtropics,
but the ease of modern travel means that some cases are seen in northern Europe
and the USA.
Presentation
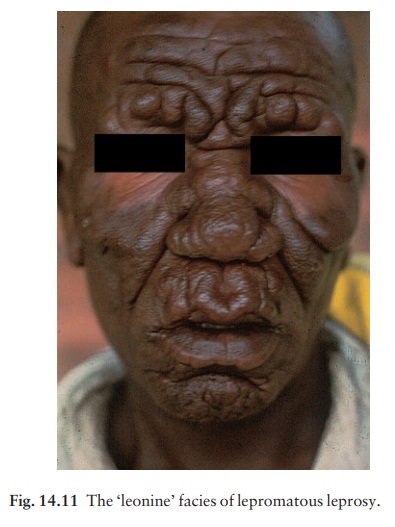
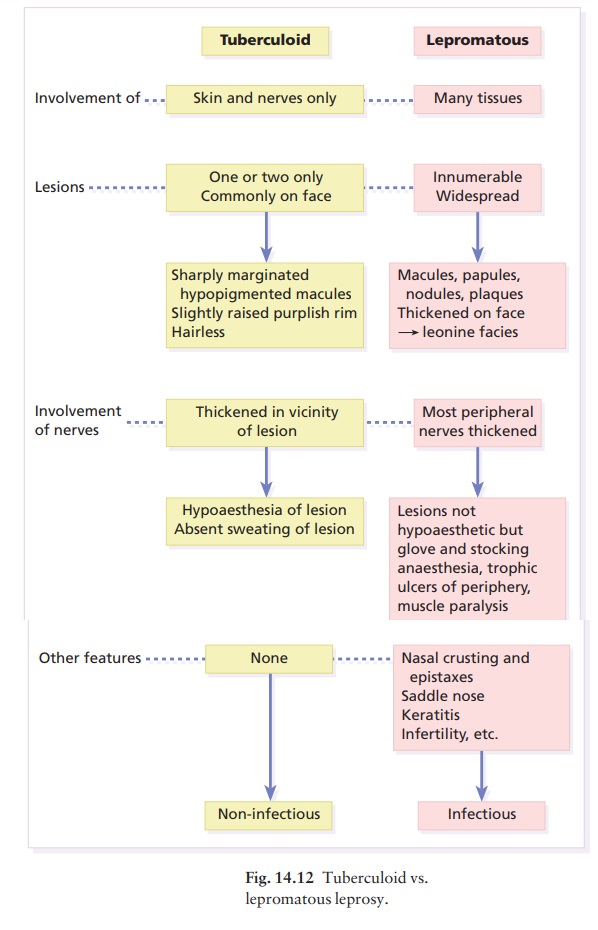
The
range of clinical manifestations and complications depends upon the immune
response of the patient (Fig. 14.9). Those with a high resistance develop a
paucibacillary tuberculoid type (Fig. 14.10) and those with
low resistance a multibacillary lepromatous type. Nerve thickening is earlier
and more marked in the tuberculoid than lepromatous type (Fig. 14.11). Between
the extremes lies a spectrum of reactions clas
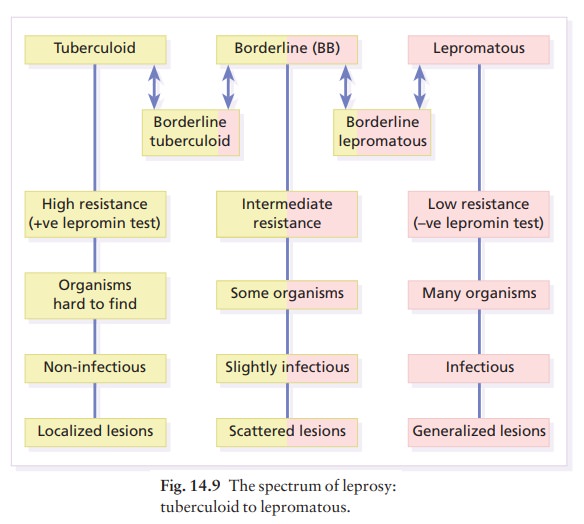

Those most like the tuberculoid type are known as borderline
tuberculoid (BT) and those nearest to the lepromatous type as borderline
lepromatous (BL). The clinical differences between the two polar types are
given in Fig. 14.12.
Differential diagnosis
Tuberculoid
leprosy. Consider the followingain noneof which is there any loss
of sensation.
ŌĆó Vitiligo
aloss of pigment is usually complete.
ŌĆó
Pityriasis versicolor ascrapings
show mycelia and spores.
ŌĆó
Pityriasis albaaa common cause of
scaly hypopig-mented areas on the cheeks of children.
ŌĆó
Postinflammatory depigmentation of
any cause.
Lepromatous
leprosy. Widespread leishmaniasis canclosely simulate lepromatous
leprosy. The nodules seen in neurofibromatosis and mycosis fungoides, and
multiple sebaceous cysts, can cause confusion, as can the acral deformities
seen in yaws and systemic sclerosis. Leprosy is a great imitator.
Investigations
ŌĆó
Biopsy of skin or sensory nerve.
ŌĆó
Skin or nasal smears, with
ZiehlŌĆōNielsen or Fit├® stains, will show up the large number of organisms seen
in the lepromatous type.
ŌĆó
Lepromin test. This is of no use in
the diagnosis of leprosy but, once the diagnosis has been made, it will help to
decide which type of disease is present (positive in tuberculoid type).
Treatment
The
emergence of resistant strains of M. leprae means that it is no longer wise to
treat leprosy with dapsone alone. It should now be used in combination,
usu-ally with rifampicin, and also with clofazimine for lepromatous leprosy. A
brief period of isolation is needed only for patients with infectious
lepromatous leprosy; with treatment they quickly become non-infectious and can
return to the community. How-ever, their management should remain in the hands
of physicians with a special interest in the disease. Tuberculoid forms are
usually treated for 6ŌĆō12 months; multibacillary leprosy needs treatment for at
least 2 years.
Special
care is needed with the two types of lepra reaction that can occur during
treatment:
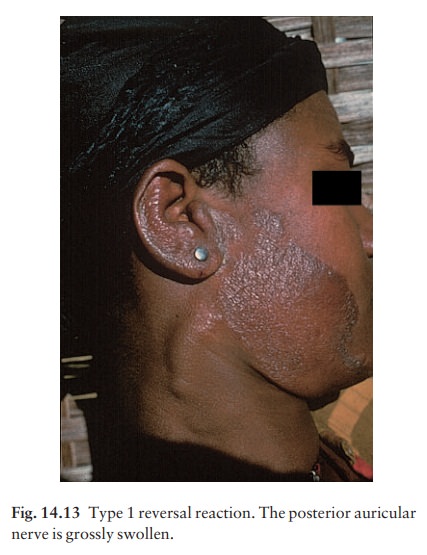
ŌĆó Type 1 (reversal) reactions are seen mainly in border-line tuberculoid disease (Fig. 14.13). Lesions become red and angry, and pain and paralysis follow neural inflammation. Treatment is with salicylates, chloro-quine, non-steroidal and steroidal anti-inflammatory drugs.
ŌĆó
Type 2 reactions are common in
lepromatous leprosy and include erythema nodosum, nerve palsies,
lymphadenopathy, arthritis, iridocyclitis, epididymo-orchitis and proteinuria.
They are treated with the drugs used for type 1 reactions, and also with
thalidomide.
The
household contacts of lepromatous patients are at risk of developing leprosy
and should be followed up. Child contacts may benefit from prophylactic therapy
and BCG inoculation.
Related Topics