Chapter: Clinical Dermatology: Infections
Bacterial infections: The resident flora of the skin
Bacterial infections
The resident flora of the skin
The
surface of the skin teems with micro-organisms, which are most numerous in
moist hairy areas, rich in sebaceous glands. Organisms are found, in clusters,
in irregularities in the stratum corneum and within the hair follicles. The
resident flora is a mixture of harm-less and poorly classified staphylococci,
micrococci and diphtheroids. Staphylococcus epidermidis and
aerobic diphtheroids predominate on the surface, and anaerobic diphtheroids
(proprionibacteria sp.) deep in the hair follicles. Several species of
lipophilic yeasts also exist on the skin. The proportion of the differ-ent
organisms varies from person to person but, once established, an individualŌĆÖs
skin flora tends to remain stable and helps to defend the skin against outside
pathogens by bacterial interference or anti-biotic production. Nevertheless,
overgrowth of skin diphtheroids can itself lead to clinical problems.
Trichomycosis axillaris
This
is a common condition, seen, if looked for, in up to one-quarter of adult
males. The axillary hairs become beaded with concretions, usually yellow, made
up of colonies of commensal diphtheroids. Clothing becomes stained in the
armpits. Topical antibiotic ointments, or shaving, will clear the condition.
Pitted keratolysis
The
combination of unusually sweaty feet and occlusive shoes encourages the growth
of diphtheroid
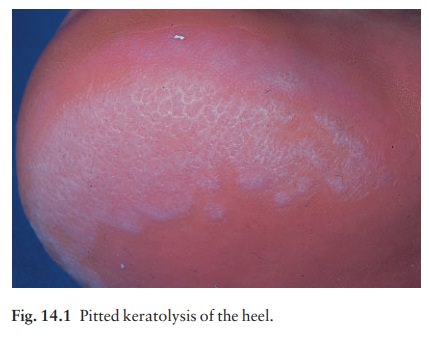
The result is a cribriform pattern of fine punched-out
depressions on the plantar surface (Fig. 14.1), coupled with an unpleasant
smell (of methane-thiol). Fusidic acid or mupirocin ointment is usually
effective. Occlusive footwear should be replaced by sandals and cotton socks if
possible.
Erythrasma
Some
diphtheroid members of the skin flora pro-duce porphyrins when grown in a
suitable medium; as a result their colonies fluoresce coral pink under WoodŌĆÖs
light. Overgrowth of these strains is some-times the cause of symptom-free
macular wrinkled slightly scaly pink, brown or macerated white areas, most
often found in the armpits or groins, or between the toes. In diabetics, larger
areas of the trunk may be involved. Diagnosis is helped by the fact that these
areas also fluoresce coral pink with WoodŌĆÖs light. Topical fusidic acid or
miconazole will clear the condition.
Staphylococcal infections
Staphylococcus
aureus is not part of the residentflora of the skin other than in a
minority who carry it in their nostrils, perineum or armpits. Carriage rates
vary with age. Nasal carriage is almost invariable in babies born in hospital,
becomes less frequent during infancy, and rises again during the school years
to the adult level of roughly 30%. Rather fewer carry the organism in the
armpits or groin. Staphylococci can also multiply on areas of diseased skin
such as eczema, often without causing obvious sepsis. A minor breach in the
skinŌĆÖs defences is probably neces-sary for a frank staphylococcal infection to
establish itself; some strains are particularly likely to cause skin sepsis.
Impetigo
Cause
Impetigo
may be caused by staphylococci, strepto-cocci, or by both together. As a useful
rule of thumb, the bullous type is usually caused by Staphylococcusaureus,
whereas the crusted ulcerated type is causedby ╬▓-haemolytic
strains of streptococci. Both are highly contagious.
Presentation A thin-walled flaccid clear blister
forms, and may become pustular before rupturing to leave an extend-ing area of
exudation and yellowish crusting (Fig. 14.2). Lesions are often multiple,
particularly around the face. The lesions may be more obviously bullous in
infants. A follicular type of impetigo (superficial folliculitis) is also
common.

Course
The
condition can spread rapidly through a family or class. It tends to clear slowly
even without treatment.
Complications
Streptococcal impetigo can trigger an acute glomerulonephritis.
Differential diagnosis
Herpes
simplex may become impetiginized, as may eczema. Always think of a possible
underlying cause such as this. Recurrent impetigo of the head and neck, for
example, should prompt a search for scalp lice.
Investigation and treatment
The
diagnosis is usually made on clinical grounds. Swabs should be taken and sent
to the laboratory for culture, but treatment must not be held up until the
results are available. Systemic antibiotics (such as flucloxacillin,
erythromycin or cephalexin (cefalexin)) are needed for severe cases or if a
nephritogenic strain of strepto-coccus is suspected (penicillin V). For minor
cases the removal of crusts and a topical antibiotic such as neo-mycin, fusidic
acid (not available in the USA), mupirocin or bacitracin will suffice.
Ecthyma
This
term describes ulcers forming under a crusted surface infection. The site may
have been that of an insect bite or of neglected minor trauma. The bacterial
pathogens
and their treatment are similar to those of impetigo; however, in contrast to
impetigo, ecthyma heals with scarring.
Furunculosis (boils)
Cause
A
boil is an acute pustular infection of a hair follicle, usually with Staphylococcus
aureus. Adolescent boys are especially susceptible to them.
Presentation and course
A
tender red nodule enlarges, and later may discharge pus and its central ŌĆścoreŌĆÖ
before healing to leave a scar. Fever and enlarged draining nodes complete the
picture. Most patients have one or two boils only, and then clear; a few suffer
from a tiresome sequence of boils (chronic furunculosis).
Complications
Cavernous sinus thrombosis is an unusual complication of boils on the central face. Septicaemia may occur but is rare.
Differential diagnosis
The
diagnosis is straightforward but hidradenitis suppurativa should be considered if only the groin and
axillae are involved.
Investigations in chronic furunculosis
ŌĆó
General examination: look for
underlying skin dis-ease (e.g. scabies, pediculosis, eczema).
ŌĆó Test the urine for sugar. Full blood count.
ŌĆó
Culture swabs from lesions, and
carrier sites (nostrils, perineum) of the patient and immediate family.
ŌĆó
Immunological evaluation only if the
patient has recurrent or unusual internal infections too.
Treatment
Acute
episodes will respond to an appropriate anti-biotic; incision speeds healing.
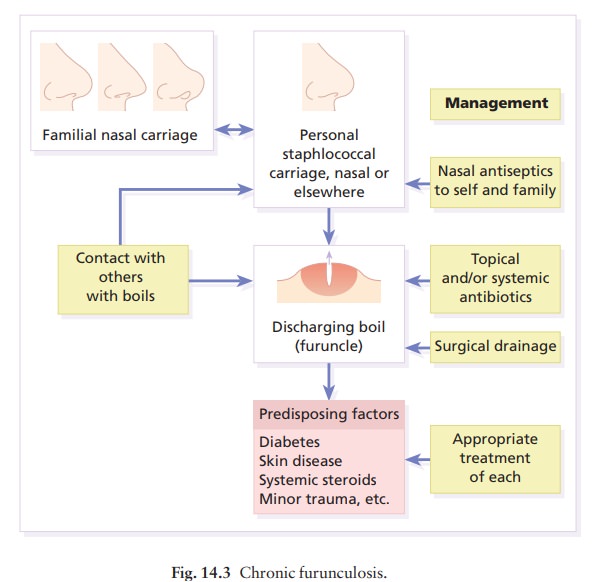
In
chronic furunculosis (Fig. 14.3):
ŌĆó
Treat carrier sites such as the nose
and groin twice daily for 6 weeks with an appropriate topical antiseptic or
antibiotic (e.g. chlorhexidine solution, mupirocin cream or clindamycin solution).
Treat family carriers in the same way.
ŌĆó
Treat lesions with a topical
antibiotic. In stubborn cases add 6 weeks of a systemic antibiotic chosen to
cover organismŌĆÖs proven sensitivities.
ŌĆó Daily bath using an antiseptic soap.
ŌĆó
Improve hygiene and nutritional
state, if faulty.
Carbuncle
A
group of adjacent hair follicles becomes deeply infected with Staphylococcus
aureus, leading to a swollen painful suppurating area discharging
pus from several points. The pain and systemic upset are greater than those of a
boil. Diabetes must be excluded. Treatment needs both topical and systemic
antibiotics. Incision and drainage has been shown to speed up healing, although
it is not always easy when there are multiple deep pus-filled pockets.
Con-sider the possibility of a fungal kerion
in unresponsive carbuncles.
Scalded skin syndrome
In
this condition the skin changes resemble a scald. Erythema and tenderness are
followed by the loosen-ing of large areas of overlying epidermis (Fig. 14.4).

In children
the condition is usually caused by a staphylo-coccal infection elsewhere (e.g.
impetigo or conjunct-ivitis). Organisms in what may be only a minor local
infection release a toxin (exfoliatin) that causes a split to occur high in the
epidermis. With systemic anti-biotics the outlook is good.
This
is in contrast to toxic epidermal necrolysis, which is usually drug-induced.
The damage to the epi-dermis in toxic epidermal necrolysis is full thickness,
and a skin biopsy will distinguish it from the scalded skin syndrome.
Toxic shock syndrome
A
staphylococcal toxin is also responsible for this con-dition, in which fever, a
rashausually a widespread erythemaaand sometimes circulatory collapse are
fol-lowed a week or two later by characteristic desquama-tion, most marked on
the fingers and hands. Many cases have followed staphylococcal overgrowth in
the vagina of women using tampons. Systemic antibiotics and irrigation of the
infected site are needed.
Related Topics