Chapter: Clinical Dermatology: Infections
Dermatophyte infections (ringworm) - Fungal infections
Fungal infections
Dermatophyte infections (ringworm)
Cause
Three
genera of dermatophyte fungi cause tinea infec-tions (ringworm).
•
Trichophytonaskin, hair and nail infections.
•
Microsporumaskin and hair.
•
Epidermophytonaskin and nails.
Dermatophytes
invade keratin only, and the inflam-mation they cause is due to metabolic
products of the fungus or to delayed hypersensitivity. In gen-eral, zoophilic
fungi (those transmitted to humans by animals) cause a more severe inflammation
than anthropophilic ones (spread from person to person).
Presentation and course
This
depends upon the site and on the strain of fungus involved.
Tinea pedis (athlete’s foot)
This
is the most common type of fungal infection in humans. The sharing of wash
places (e.g. in show-ers) and of swimming pools, predisposes to infection;
occlusive footwear encourages relapses.
Most
cases are caused by one of three organisms:
Trichophyton rubrum (the most common and the most stubborn), Trichophyton mentagrophytes var.
interdigitale
and Epidermophyton floccosum.
There
are three common clinical patterns.
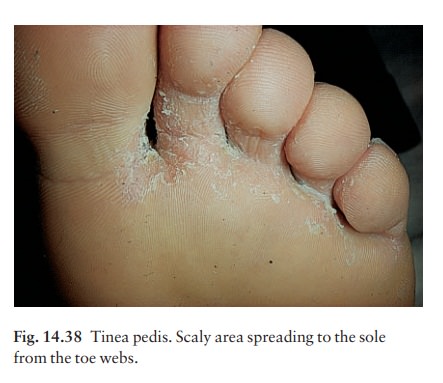
1 Soggy
interdigital scaling, particularly in the fourth and fifth interspace (all
three organisms; Fig. 14.38).
2 A diffuse
dry scaling of the soles (usuallyT. rubrum;Fig. 14.39).

3 Recurrent episodes of vesication (usuallyT. menta-grophytes var. interdigitale or E. floccosum).
Tinea of the nails
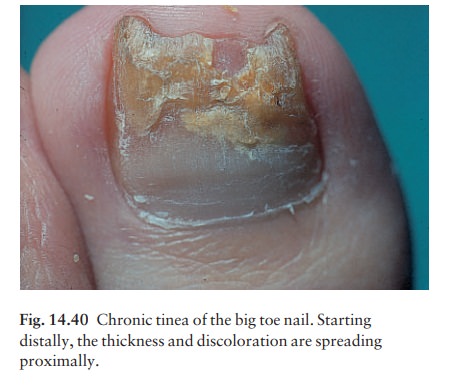
Toenail
infection is usually associated with tinea pedis. The initial changes occur at
the free edge of the nail, which becomes yellow and crumbly (Fig. 14.40).
Subungual hyperkeratosis, separation of the nail from its bed, and thickening
may then follow. Usually only a few nails are infected but rarely all are.
Fingernail lesions are similar, but less common, and are seldom seen without a
chronic T.
rubrum infection of the skin of the hands.
Tinea of the hands
This
is usually asymmetrical and associated with tinea pedis. T. rubrum
may cause a barely perceptible erythema of one palm with a characteristic
powdery scale in the creases.
Tinea of the groin
This
is common and affects men more often than women. The eruption is sometimes
unilateral or asymmetrical. The upper inner thigh is involved and lesions
expand slowly to form sharply demarcated plaques with peripheral scaling (Fig.
14.41). In con-trast to candidiasis of the groin area, the scrotum is usually
spared. A few vesicles or pustules may be seen within the lesions. The organisms
are the same as those causing tinea pedis.

Tinea of the trunk and limbs
Tinea
corporis is characterized by plaques with scal-ing and erythema most pronounced
at the periphery. A few small vesicles and pustules may be seen within them.
The lesions expand slowly and healing in the centre leaves a typical ring-like
pattern.
Tinea of the scalp (tinea capitis)
This
is usually a disease of children. The causative organism varies from country to
country.
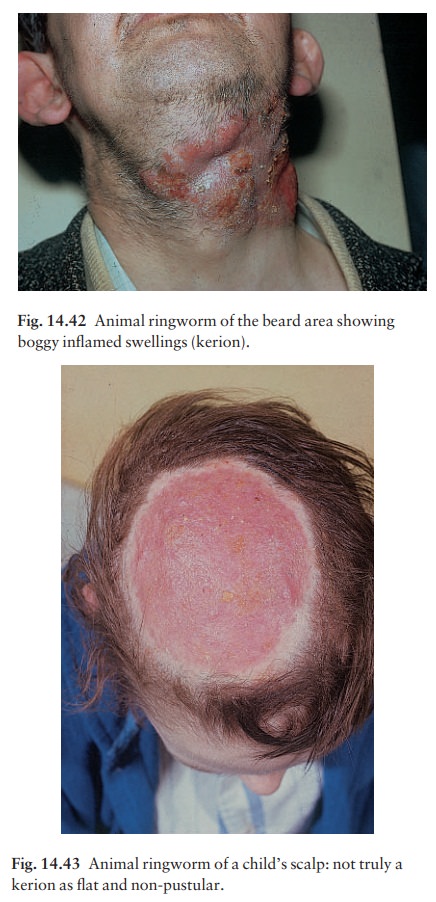
Fungi
coming from animal sources (zoophilic fungi) induce a more intense inflammation
than those spread from person to person (anthropophilic fungi). In ring-worm
acquired from cattle, for example, the boggy swelling, with inflammation,
pustulation and lymphad-enopathy, is often so fierce that a bacterial infection
is suspected; such a lesion is called a kerion and the hair loss associated
with it may be permanent. Tinea of the beard area is usually caused by
zoophilic species and shows the same features (Fig. 14.42). Anthropophilic
organisms cause bald rather scaly areas, with minimal
In favus, caused by Trichophyton
schoenleini, the picture is dominated by foul-smelling yellowish crusts
surrounding many scalp hairs, and sometimes leading to scarring alopecia.
Complications
1 Fierce animal ringworm of the scalp (Fig. 14.43) can lead to a permanent scarring alopecia.
2 A florid
fungal infection anywhere can inducevesication on the sides of the fingers and
palms (a trichophytide).
3 Epidemics
of ringworm occur in schools.
4 The
usual appearance of a fungal infection can be masked by mistreatment with
topical steroids (tinea incognito; Fig. 14.44).

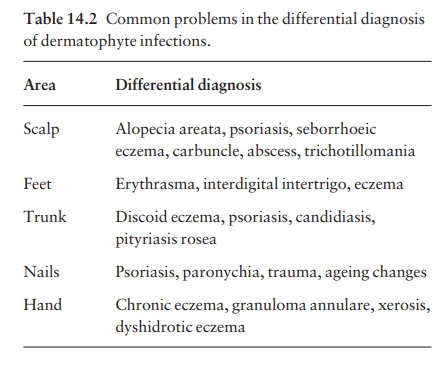
Differential diagnosis
This
varies with the site. Some of the more common problems are listed in Table
14.2.
Investigations
The microscopic examination of a skin scraping, nail clipping or plucked hair is a simple procedure.
The scraping
should be taken from the scaly margin of a lesion, with a small curette or a
scalpel blade, and clippings/scrapings from the most crumbly part of a nail.
Broken hairs should be plucked with tweezers. Specimens are cleared in
potassium hydrox-ide. Branching hyphae can easily be seen (see Fig. 3.7) using
a scanning (Ă— 10) or
low-power (Ă— 25)
objective lens, with the iris diaphragm almost closed, and the condenser racked
down. Hyphae may also be seen within a cleared hair shaft, or spores may be
noted around it.
Cultures should
be carried out in a mycology orbacteriology laboratory. Transport medium is not
necessary, and specimens should be sent in folded black paper. The report may
take as long as a month; microscopy is much quicker.
Wood’s
light (ultraviolet light) examination of thescalp usually reveals
a green fluorescence of the hairs in Microsporum audouini and M. canis
infections. The technique is useful for screening children in insti-tutions
where outbreaks of tinea capitis still some-times occur, but some fungi (e.g. Trichophytontonsurans)
do not fluoresce.
Treatment
Local
This
is all that is needed for minor skin infections. The more recent imidazole
preparations (e.g. miconazole and clotrimazole) and the allylamines such as
terbina-fine, have largely superseded time-honoured remedies such as benzoic
acid ointment (Whitfield’s ointment) and tolnaftate. They should be applied
twice daily. Magenta paint (Castellani’s paint), although highly coloured, is
helpful for exudative or macerated areas in body folds or toe webs. Occasional
dusting with an antifungal powder is useful to prevent relapses.
Topical
nail preparations. Many patients now pre-fer to avoid
systemic treatment. For them a nail lacquer containing amorolfine is worth a
trial. It should be applied once or twice a week for 6 months; it is effective
against stubborn moulds such as Hendersonula and Scopulariopsis.
Both amorolfineand tioconazole nail solutions can be used as adjuncts to
systemic therapy .
Systemic
This
is needed for tinea of the scalp or of the nails, and for widespread or chronic
infections of the skin that have not responded to local measures.
Terbinafine
has now
largelysuperceded griseofulvin. It acts by inhibiting fungal squalene epoxidase
and does not interact with the cytochrome P-450 system. It is fungicidal and so
cures chronic dermatophyte infections more quickly and more reliably than
griseofulvin. For tinea capitis in children, for example, a 4-week course of
terbinafine is as effective as an 8-week course of griseofulvin. Cure rates of
70–90% can be expected for infected fingernails after a 6-week course of
terbinafine, and for infected toenails after a 3-month course. It is not
effective in pityriasis versicolor or Candida
infections.
Griseofulvin
was for manyyears the
drug of choice for chronic dermatophyte infections. It has proved to be a safe
drug, but treat-ment may have to be stopped because of persistent headache,
nausea, vomiting or skin eruptions. The drug should not be given in pregnancy
or to patients with liver failure or porphyria. It interacts with coumarin
anticoagulants, the dosage of which may have to be increased. Its effectiveness
falls if barbitur-ates are being taken at the same time.
Griseofulvin
is fungistatic and treatment for infected nails has to be prolonged (an average
of 12 months for fingernails, and at least 18 months for toe-nails). The
disappointing results for toenail infections seen in some 30 – 40% of cases can
be improved by the concomitant use of topical nail preparations .
Itraconazole
(Formulary 2) is now pre-ferred to ketoconazole, which
occasionally damages the liver, and is a reasonable alternative to terbinafine
and griseofulvin if these are contraindicated. It is effective in tinea
corporis, cruris and pedis; and also in nail infections, although without a
licence for this use in many countries. Fungistatic rather than fun-gicidal, it
interferes with the cytochrome P-450 sys-tem, so a review of any other
medication being taken is needed before a prescription is issued. Its wide
spectrum makes it useful also in pityriasis versicolor and candidiasis.
Related Topics