Chapter: Clinical Dermatology: Infections
Spirochaetal infections
Spirochaetal
infections
Syphilis
Cause
Infection with the causative organism, Treponemapallidum, may be congenital, acquired through trans-fusion with contaminated blood, or by accidental inoculation. The most important route, however, is through sexual contact with an infected partner.
Presentation
Congenital
syphilis. If there is a high standard ofantenatal care, syphilis in
the mother will be detected and treated during pregnancy, and congenital
syphilis will be rare. Otherwise, stillbirth is a common out-come, although
some children with congenital syphilis may develop the stigmata of the disease
only in late childhood.
Acquired
syphilis. The features of the different stagesare given in Fig.
14.6. After an incubation period (9ŌĆō90 days), a primary chancre develops at the
site of inoculation. Often this is genital, but oral and anal chancres are not
uncommon. A typical chancre is an ulcerated, although not painful, button-like
lesion of up to 1 cm in diameter accompanied by local lymphadenopathy.
Untreated it lasts about 6 weeks and then clears leaving an inconspicuous scar.
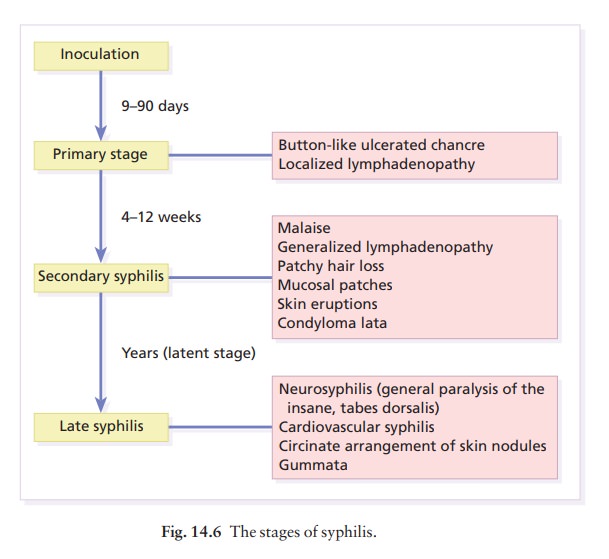
The secondary stage may be reached while the chancre is still subsiding. Systemic symptoms and a generalized lymphadenopathy usher in eruptions that at first are macular and inconspicuous, and later papular and more obvious. Lesions are distributed symmetrically and are of a coppery ham colour. Some-times they resemble pityriasis rosea. Classically, there are obvious lesions on the palms and soles. Annular lesions are also not uncommon. Condyloma lata are moist papules in the genital and anal areas. Other signs include a ŌĆśmoth-eatenŌĆÖ alopecia and mucous patches in the mouth.
The
skin lesions of late syphilis may be nodules that spread peripherally and clear
centrally, leaving a serpiginous outline. Gummas are granulomatous areas; in
the skin they quickly break down to leave punched-out ulcers that heal poorly,
leaving papery white scars.
Clinical course
Even
if left untreated, most of those who contract syphilis have no further problems
after the secondary stage has passed. Others develop the cutaneous or systemic
manifestations of late syphilis.
Differential diagnosis
The
skin changes of syphilis can mimic many oth skin diseases. Always consider the
following.
1 Chancre:
chancroid (multiple and painful), herpes simplex, anal fissure, cervical
erosions.
2 Secondary
syphilis:
ŌĆó
eruptionameasles, rubella, drug
eruptions, pity-riasis rosea, lichen planus, psoriasis;
ŌĆó condylomasagenital warts, haemorrhoids;
ŌĆó
oral lesionsaaphthous ulcers,
candidiasis.
3 Late
syphilis: bromide and iodide reactions, other granulomas, erythema induratum.
Investigations
The
diagnosis of syphilis in its infectious (primary and secondary) stages can be
confirmed using dark field microscopy to show up spirochaetes in smears from
chancres, oral lesions, or moist areas in a secondary eruption.
Serological
tests for syphilis become positive only some 5ŌĆō 6 weeks after infection (usually
a week or two after the appearance of the chancre). The traditional tests
[Wasswemann reaction (WR) and Venereal Dis-ease Research Laboratory (VDRL)]
have now been replaced by more specific ones [e.g. the rapid plasma reagin
(RPR) test and the fluorescent treponemal antibody/absorption (FTA/ABS) test].
These more sensitive tests do not become negative after treatment if an
infection has been present for more than a few months.
Treatment
This
should follow the current recommendations of the World Health Organization
(WHO). Penicillin is still the treatment of choice (e.g. for early syphilis
benzathine penicillin 1.2 million units given intramus-cularly into each
buttock at a single session, or pro-caine penicillin 600 000 units
intramuscularly daily for 12 days), with long-term high-dose oral erythromycin
and tetracycline being effective alternatives for those with penicillin
allergy. The use of long-acting penicillin injections overcomes the
ever-present danger of poor compliance with oral treatment. Every effort must
be made to trace and treat infected contacts.
Yaws
Yaws
is distributed widely across the poorer parts of the tropics. The spirochaete, Treponema
pallidum ssp. pertenue, gains its entry through skin
abrasions. After an incubation period of up to 6 months, the primary lesion, a
crusting and ulcerated papule known as the ŌĆśmother yawŌĆÖ, develops at the site
of inoculation; later it may enlarge to an exuberant raspberry-like swelling
which lasts for several months before healing to leave an atrophic pale scar.
In the secondary stage, other lesions may develop in any area but do so
especially around the orifices. They are not unlike the primary lesion but are
smaller and more numer-ous (ŌĆśdaughter yawsŌĆÖ). Hyperkeratotic plaques may appear
on the palms and soles. The tertiary stage is characterized by ulcerated
gummatous skin lesions, hyperkeratosis of the palms and soles, and a painful
periostitis that distorts the long bones. Serological tests for syphilis are
positive. Treatment is with penicillin.
Lyme disease
The
spirochaete Borrelia
burgdorferi is responsible for this condition, named after the town in
the USA where it was first recognized. It is transmitted to humans by ticks of
the genus Ixodes,
commonly harboured by deer. The site of the tick bite becomes the centre of a
slowly expanding erythematous ring (ŌĆśerythema migransŌĆÖ; Fig. 14.7). Later, many
annular non-scaly plaques may develop. In the USA, a few of those affected
develop arthritis and heart disease, both of which are less com-mon in European
cases. Other internal complications include meningitis and cranial nerve
palsies. Treated early, the condition clears well with a 21-day course of oral
amoxycillin or doxycycline: patients affected systemically need longer courses
of parenteral anti-biotics. Infection can be confirmed by serology, although
this is usually negative in the first few weeks after innoculation.

Related Topics