Chapter: Clinical Dermatology: Infections
Other mycobacterial infections
Other
mycobacterial infections
Mycobacteria are widespread in nature, living as environmental saprophytes. Some can infect humans.
Mycobacterium marinum
Mycobacterium
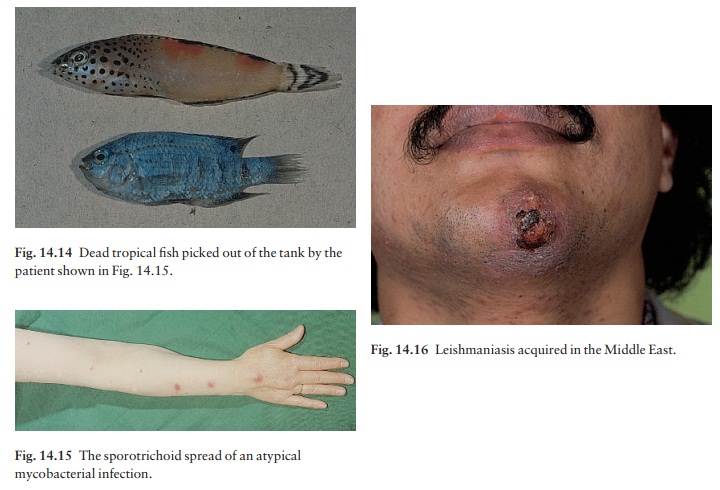
marinum lives in water. Human infec-tions have occurred in epidemics
centred on infected swimming pools. Another route of infection is through minor
skin breaches in those who clean out tropical fish tanks (Fig. 14.14). After a
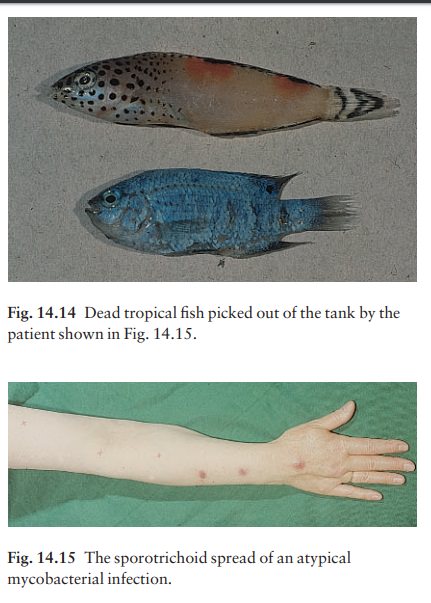
3-week incubation period, an indolent abscess or ulcerated nodule forms at the
site of inoculation; later nodules may develop along the draining lymphatics
(sporotrichoid spread; Fig. 14.15). The lesions heal spontan-eously, but
slowly. Resolution may be speeded by an 8-week course of trimethoprim/sulfamethoxazole
or minocycline. Should these fail, rifampicin in combination with ethambutol
is worth a trial.
Mycobacterium ulcerans
Infections are confined to certain humid tropical areas where the organism lives on the vegetation, and are most common in Uganda (Buruli ulcers). The necrotic spreading ulcers, with their undermined edges, are usually found on the legs. Drug therapy is often dis-appointing and the treatment of choice is probably the surgical removal of infected tissue.
Leishmaniasis
Leishmania
organisms are protozoa whose life cycle includes stages in phlebotomus flies,
from which they are transmitted to humans. Different species, in differ-ent geographical
areas, cause different clinical pictures.
ŌĆó
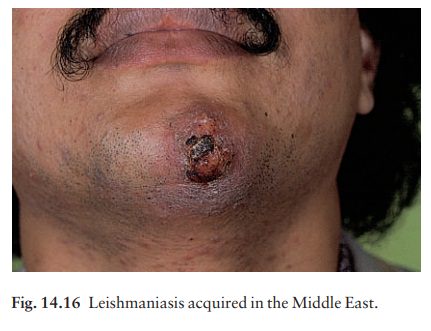
Leishmania tropica is found
around the Mediter-ranean coast and in southern Asia; it causes chronically
discharging skin nodules (oriental sores; Fig. 14.16).
ŌĆó
Leishmania donovani causes
kala-azar, a dis-ease characterized by fever, hepatosplenomegaly and anaemia.
The skin may show an irregular darkening, particularly on the face and hands.
ŌĆó
Leishmania mexicana and
braziliensis are foundin South and Central America. They also cause deep
sores, but up to 40% of those infected with L. braziliensis
develop ŌĆśepisodicŌĆÖ, destructive metastaticlesions in the
mucosa of the nose or month.
Diagnosis
This
is confirmed by:
ŌĆó
histologyaamastigote parasites,
granulomatous reaction;
touch smearaamastigote parasites;
ŌĆó
culture; and
ŌĆó
polymerase chain reaction tests.
Treatment
Single
nodules often resolve spontaneously and may not need treatment. Destructive
measures, including cryotherapy, are sometimes used for localized skin lesions.
Oral zinc sulphate (5 mg/kg/day for 4 weeks) showed promising results in a
recent Indian trial.
Intralesional
or intravenous antimony compounds are still the treatment of choice for most
types of leish-maniasis, e.g. sodium stibogluconate (20 mg/kg/day for 20 days)
with regular blood tests and electrocar-diographic monitoring.
Related Topics