Chapter: Ophthalmology: Retina
Retinal Detachment
Degenerative Retinal Disorders
Retinal Detachment
Definition
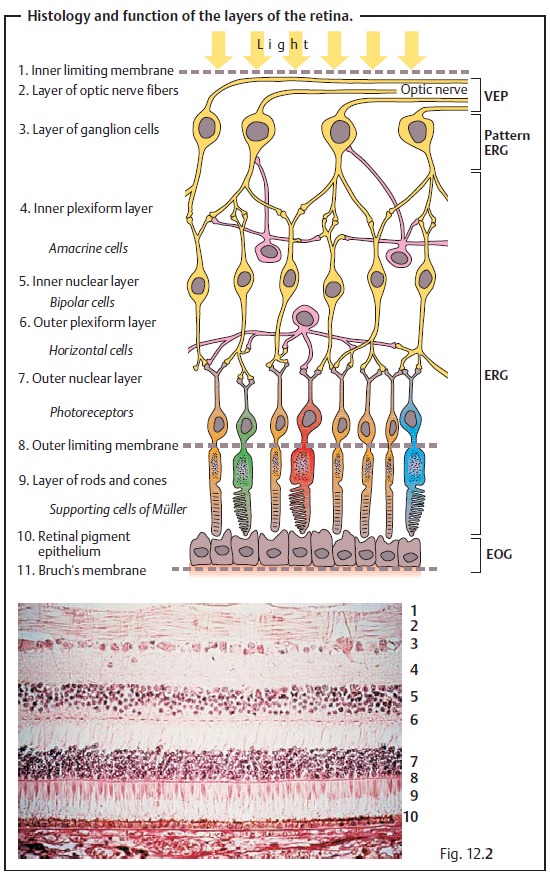
Retinal detachment refers to the separation of
the neurosensory retina (see Fig. 12.2a)
from the underlying retinal pigment epithelium, to which normally it is loosely
attached. This can be classified into four types:
âť– Rhegmatogenous retinal detachment results from a tear, i.e., a break inthe
retina.
âť– Tractional retinal detachment results from traction, i.e., from
vitreousstrands that exert tensile forces on the retina (see proliferative
vitreoreti-nopathy and complicated retinal detachment).
âť– Exudative retinal detachment is caused by fluid. Blood, lipids, or
serousfluid accumulates between the neurosensory retina and the retinal
pig-ment epithelium. Coats’ disease is a typical example.
âť– Tumor-related retinal detachment.
Primary retinal detachment usually results from a tear. In rare cases, second-ary retinal detachment may also result from a tear due to
other disorders orinjuries. Combinations of both are also possible but rare.
Proliferative vitreore-tinopathy frequently develops from a chronic retinal
detachment.
Epidemiology:
Although retinal detachments are relatively rarely encoun-tered
in ophthalmologic practice, they are clinically highly significant as they can
lead to blindness if not treated immediately.
Rhegmatogenous retinal detachment (most frequent form): Approxi-mately 7% of all adults have
retinal breaks. The incidence of this finding increases with advanced age. The peak incidence is
between the fifth and seventh decades of life. This indicates the significance
of posterior vitreous detachment (separation of the vitreous body from inner
surface of the retina; also age-related) as a cause of retinal detachment. The
annual incidence of retinal detachment is one per 10 000 persons; the
prevalence is about 0.4% in the elderly. There is a known familial disposition,
and retinal detachment also occurs in conjunction with myopia. The prevalence of retinal detachment with emmetropia
(normal vision) is 0.2 % compared with 7% in the presence of severe myopia
exceeding minus 10 diopters.
Exudative, tractional, and tumor-related retinal detachments areencountered far less frequently.
Etiology:
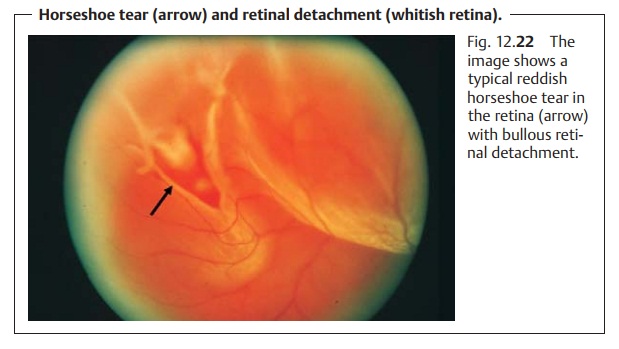
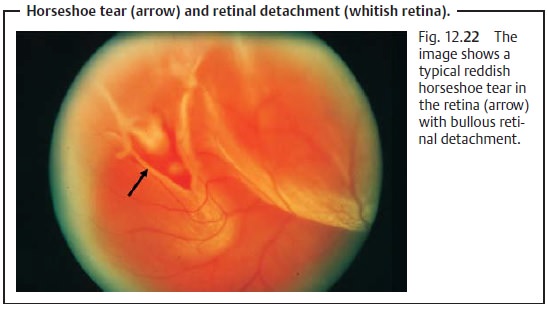
Rhegmatogenous retinal detachment.This disorder develops froman existing break in the retina. Usually this break is in the peripheral retina, rarely in the macula (Fig. 12.22). Two types of breaks are distinguished:
âť– Round breaks: A portion of the retina has been completely torn out due to
aposterior vitreous detachment.
âť– Horseshoe tears: The retina is only slightly torn.
Not every retinal break leads to retinal
detachment. This will occur only where the liquified vitreous body separates,
and vitreous humor penetrates beneath the retina through the tear. The retinal
detachment occurs when the forces of adhesion can no longer withstand this
process. Tractional forces (tensile forces) of the vitreous body (usually
vitreous strands) can also cause retinal detachment with or without synchysis.
In this and every other type of retinal detachment, there is a dynamic interplay of tractional and
adhesiveforces. Whether the retina will detach depends on which of these
forces isstronger.
Tractional retinal detachment.This develops from the tensile forces exertedon the retina by
preretinal fibrovascular strands (see proliferative vitreoreti-nopathy)
especially in proliferative retinal diseases such as diabetic reti-nopathy.
Exudative retinal detachment.The primary cause of this type is the break-down of the inner or
outer blood – retina barrier, usually as a result of a vascu-lar disorder such
as Coats’ disease. Subretinal fluid with or without hard exu-date accumulates
between the neurosensory retina and the retinal pigment epithelium.
Tumor-related retinal detachment.Either the transudate from the tumorvasculature or the mass of
the tumor separates the retina from its underlying tissue.
Symptoms:
Retinal detachment can remain asymptomatic for a long time.
Inthe stage of acute posterior vitreous detachment, the patient will notice flashes of light (photopsia) and floaters, black points that move with
thepatient’s gaze. A posterior vitreous detachment that causes a retinal tear
may also cause avulsion of a retinal vessel. Blood from this vessel will then
enter the vitreous body. The patient will perceive this as “black rain,” numerous slowly falling
small black dots. Another symptom is a dark
shadow in thevisual field. This occurs when the retina detaches. The
patient will perceive afalling curtain or a rising wall, depending on whether
the detachment is supe-rior or inferior. A break in the center of the retina
will result in a sudden and significant loss
of visual acuity, which will include metamorphopsia (image distortion) if
the macula is involved.
Diagnostic considerations:
The lesion is diagnosed by stereoscopic exami-nation of the
fundus with the pupil dilated. The detached retina will be white and edematous
and will lose its transparency. Ophthalmoscopy will reveal a bullous retinal
detachment; in rhegmatogenous retinal
detachment, a bright red retinal break will also be visible (see Fig. 12.22). The tears in rheg-matogenous
retinal detachment usually occur in the superior half of the ret-ina in a
region of equatorial degeneration. In tractional
retinal detachment, the bullous detachment will be accompanied by
preretinal gray strands. In exudative
retinal detachment, one will observe the typical picture of
serousdetachment; the exudative retinal detachment will generally be
accom-panied by massive fatty deposits and often by intraretinal bleeding.
The tumor-related retinal
detachment (as can occur with
a malignant melanoma) either leads to secondary retinal detachment over the
tumor or at some distance from the tumor in the inferior peripheral retina.
Ultrasound studies can help confirm the diagnosis where retinal findings are
equivocal or a tumor is suspected.
An inferior retinal detachment at some
distance from the tumor is a sign that the tumor is malignant.
Differential diagnosis:
Degenerativeretinoschisisis
the primary disorderthat should be excluded as it can also involve rhegmatogenous
retinal detach-ments in rare cases. A retinal detachment may also be confused
with a choroidal detachment. Fluid accumulation in the choroid, due to
inflam-matory choroidal disorders such as Vogt-Koyanagi-Harada syndrome, causes
the retinal pigment epithelium and neurosensory retina to bulge outward. These
forms of retinal detachment have a greenish dark brown color in con-trast to
the other forms of retinal detachment discussed here.
Treatment:
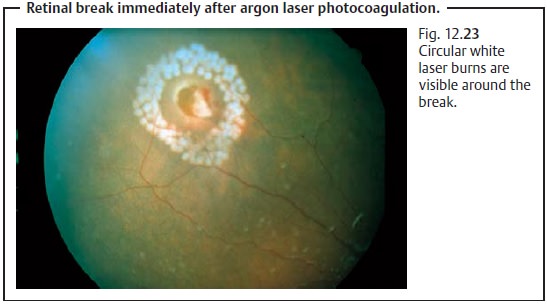
Retinal breaks with minimal circular retinal detachment can betreated with argon laser coagulation (Fig. 12.23). The retina surrounding the break is fused to the underlying tissue whereas the break itself is left open. The scars resulting from argon laser therapy are sufficient to prevent any further retinal detachment.
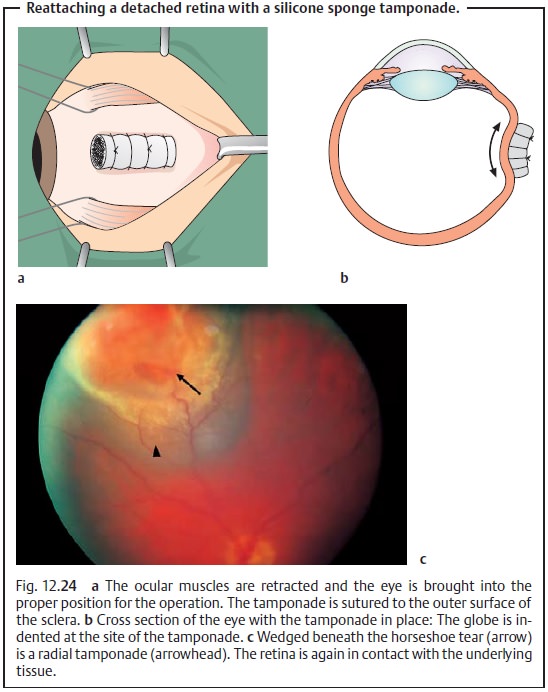
More extensive
retinal detachments are usually treated with a retinal tamponade with an
elastic silicone sponge that is sutured to the outer surface of the sclera, a so-called
budding procedure (Fig. 12.24a – c). It can be sutured either in a radial position (perpendicular
to the limbus) or parallel to the limbus. This indents the wall of the globe at
the retinal break and brings the portion of the retina in which the break is
located back into contact with the retinal pigment epithelium. The indentation
also reduces the traction of the vitreous body on the retina. An artifical scar is created to stabilize the restored contact between the
neurosensory retina and retinal pigment epithelium. This is achieved with a
cryoprobe. After a successful operation, this scar prevents recurring retinal
detachment. Where there are several retinal breaks or the break cannot be
located, a silicone cer-clage is applied to the globe as a circumferential buckling procedure.
The pro-cedures described up until now apply to uncomplicated retinal detachments, i.e., without proliferative
vitreoretinopathy. Suturing a retinal tamponade with silicone sponge may also
be attempted initially in a complicated
retinaldetachment with proliferative vitreoretinopathy. If this treatment
isunsuccessful, the vitreoretinal proliferations are excised, and a vitrectomy isperformed in which the
vitreous body is replaced with Ringer’s solution, gas,or silicone oil. These
fluids tamponade the eye from within.
Prophylaxis:
High-risk patients above the age of 40 with a positive
familyhistory and severe myopia should be regularly examined by an
ophthalmolo-gist, preferably once a year.
Clinical course and prognosis:
About 95% of rhegmatogenous retinaldetachments can be treated successfully with surgery. Where there has been macular involvement (i.e., the initial detachment included the macula), a loss of visual acuity will remain. The prognosis for the other forms of retinaldetachment is usually poor, and they are often associated with significantloss of visual acuity.
Related Topics