Chapter: Ophthalmology: Retina
Diabetic Retinopathy
Vascular Disorders
Diabetic Retinopathy
Definition
Diabetic retinopathy is an ocular
microangiopathy.
Epidemiology:
Diabetic retinopathy is one of the main causes of
acquiredblindness in the industrialized countries. Approximately 90% of all diabetic
patients have retinopathy after twenty years.
Pathogenesis and individual stages of diabetic retinopathy:
Diabetes mel-litus can lead to changes in almost every ocular
tissue. These include symp-toms of keratoconjunctivitis sicca, xanthelasma, mycotic
orbital infections, transitory refractory changes, cataract, glaucoma,
neuropathy of the optic nerve, oculomotor palsy. However, 90% of all visual impairments in diabetic patients are caused by
diabetic retinopathy. The most common international nomenclature used to
describe the various changes in diabetic retinopathy
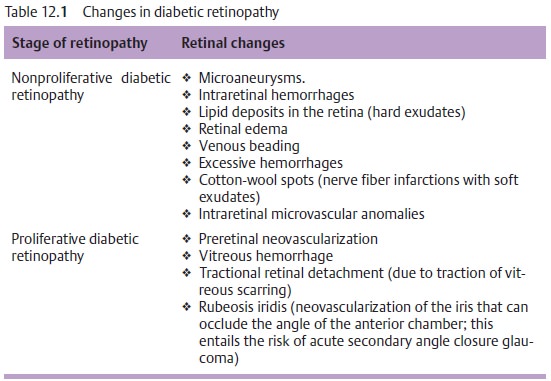
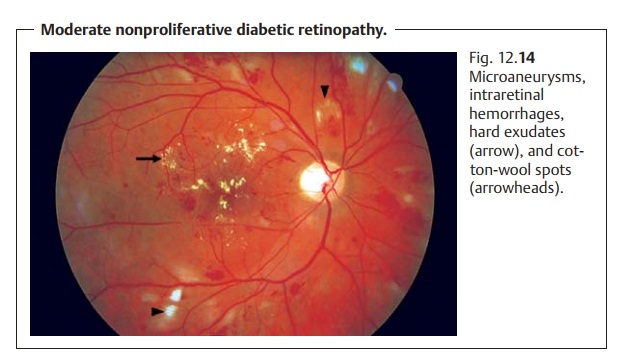
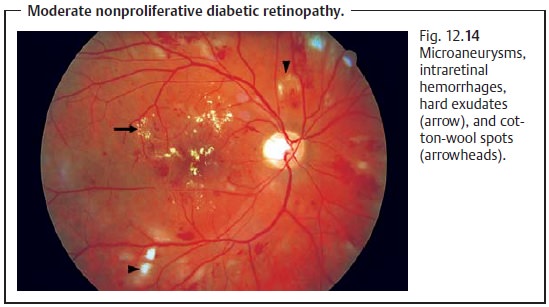
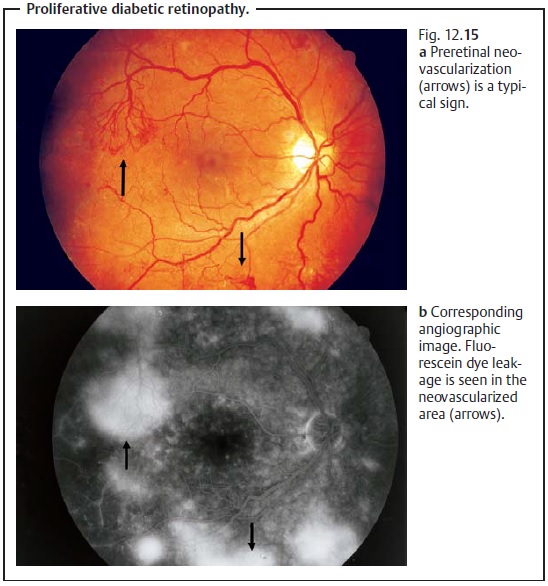
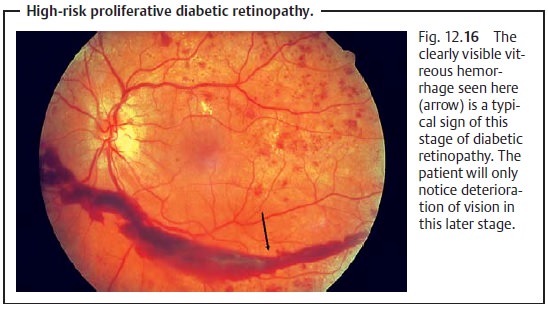
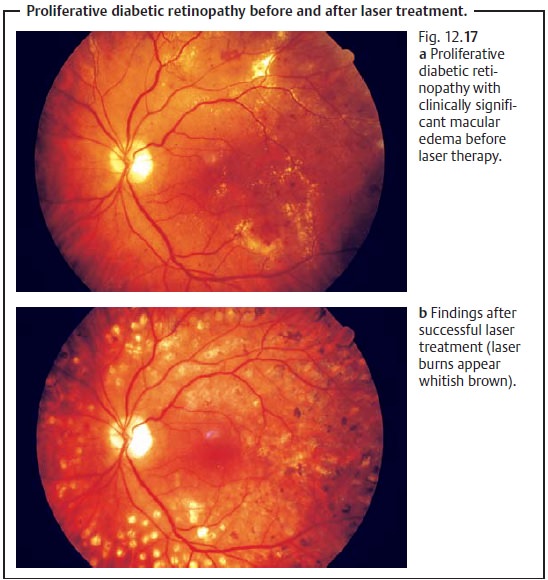
(Table 12.1) is based on the classification of the Diabetic Retinopathy Study. A distinction is made between nonproliferative stages (1. mild, 2. moderate, 3. severe; Fig. 12.14) and proliferative stages (1. non-high-risk 2. high-risk; Fig. 12.15–12.17).
Symptoms:
Diabetic retinopathy remains asymptomatic for a long time.
Onlyin the late stages with macular involvement or vitreous hemorrhage will the
patient notice visual impairment or suddenly go blind.
Diagnostic considerations:
Diabetic retinopathy and its various stages (seeTable 12.1) are diagnosed by stereoscopic examination of the fundus with the pupil dilated. Ophthalmoscopy and evaluation of stereoscopic fundus photographs represent the gold standard. Fluorescein angiography is used to determine if laser treatment is indicated. The presence of rubeosis iridis is confirmed or excluded in slit-lamp examination with a mobile pupil, i.e., without the use of a mydriatic, and by gonioscopy of the angle of the anterior chamber.
Differential diagnosis:
A differential diagnosis must exclude other vascularretinal
diseases, primarily hypertonic changes of the fundus (this is done by excluding
the underlying disorder).
Treatment:
Clinically significant macular edema, i.e., macular edema
thatthreatens vision, is managed with focal laser treatment at the posterior
pole. Proliferative diabetic retinopathy is treated with scatter
photocoagulation performed in three to five sessions.
Prophylaxis:
Failure to perform regular ophthalmologic screening
examina-tions in patients with diabetes mellitus is a negligent omission that
exposes patients to the risk of blindness. Therefore, all type II diabetics
should undergo ophthalmologic examination upon diagnosis of the disorder, and
type I diabetics should undergo ophthalmologic examination within five years of
the diagnosis. Thereafter, diabetic patients should undergo ophthal-mologic
examination once a year, or more often if diabetic retinopathy is present. Pregnant
patients should be examined once every trimester.
Clinical course and prognosis:
Optimum control of blood glucose can pre-vent or delay
retinopathy. However, diabetic retinopathy can occur despite optimum therapy.
Rubeosis iridis (neovascularization in the iris) in prolifera-tive diabetic
retinopathy is tantamount to loss of the eye as rubeosis iridis is a relentless
and irreversible process.
The risk of blindness due to diabetic retinopathy can be reduced by optimum control of blood glucose, regular ophthalmologic examina-tion, and timely therapy, but it cannot be completely eliminated.
Related Topics