Chapter: Ophthalmology: The Eyelids
Eyelids: Deformities
Deformities
Ptosis
Definition
Paralysis of the levator palpebrae muscle with
resulting drooping of one or both upper eyelids (from the Greek ptosis, a falling). The following forms
are differentiated according to their origin (see also Etiology):
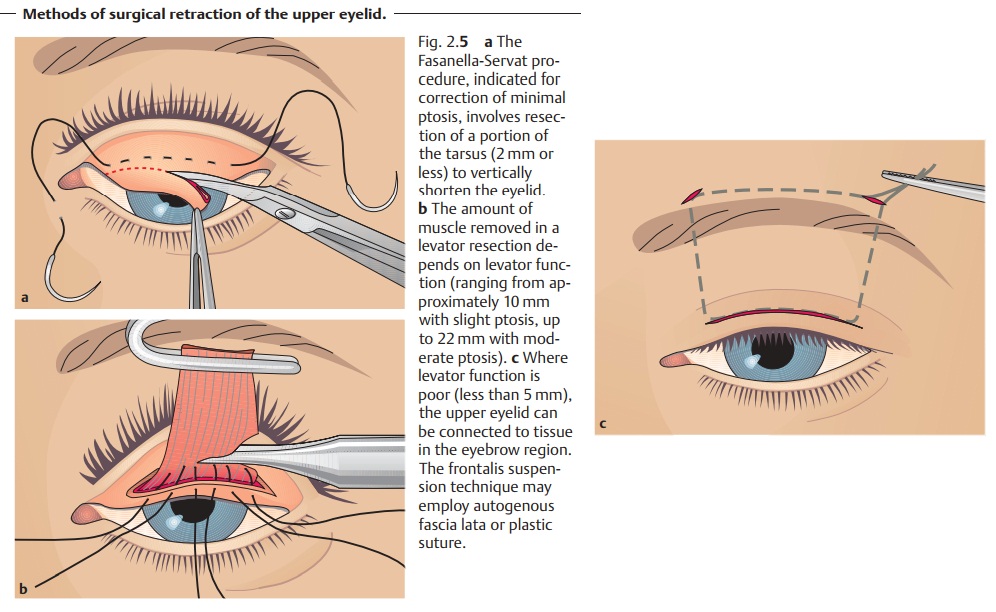
❖Congenital ptosis (Fig. 2.4).
❖ Acquired ptosis:
–
Paralytic ptosis.
–
Sympathetic ptosis.
–
Myotonic ptosis.
–
Traumatic ptosis.
Epidemiology.On the whole ptosis is a rare disorder.
Etiology: Ptosis may be congenital or acquired.
Congenital ptosis.The disorder is usually hereditary and is primarily auto-somal
dominant as opposed to recessive. The cause is frequently aplasia in the core of the
oculomotor nerve (neurogenic) that supplies the levator palpe-brae muscle;
less frequently it is attributable to an underdeveloped
levatorpalpebrae muscle (myogenic).
Acquired ptosis:
❖ Neurogenic causes:
–
Oculomotor palsy (paralytic ptosis).
– Lesions in the sympathetic nerve (sympathetic ptosis) is Horner’s palsy
(ptosis, miosis, and enophthalmos).
❖Myogenic ptosis: myasthenia gravis and myotonic
dystrophy.
❖ Traumatic ptosis can occur after injuries.
Symptoms.The drooping of the upper eyelid may beunilateral(usually a signof a neurogenic
cause) or bilateral (usually a sign
of a myogenic cause). A
characteristic feature of the unilateral
form is that the patient attempts to increase the palpebral fissure by
frowning (contracting the frontalis muscle). Congenital ptosis (Fig. 2.4)
generally affects one eye only; bilateral symptomsare observed far less
frequently (7%).
Diagnostic considerations: Congenital ptosis.The affected eyelid in generalis
underdeveloped. The skin of the upper eyelid is smooth and thin; the supe-rior
palpebral furrow is absent or ill-defined. A typical symptom is “lid lag” in which the upper eyelid does
not move when the patient glances down. Thisimportant
distinguishing symptom excludes acquired ptosis in differential diag-nosis. In
about 3% of all cases, congenital ptosis is associated with epicanthalfolds and
blepharophimosis (Waardenburg syndrome).
Congenital ptosis can occur in varying degrees
of severity and may be com-plicated by the presence of additional eyelid and
ocular muscle disorders such as strabismus.
Congenital ptosis in which the upper eyelid
droops over the center of the pupil always involves an increased risk of
amblyopia.
Acquired ptosis:
❖ Paralytic ptosis in oculomotor palsy is usually
unilateralwith the drooping eyelid covering the whole eye. Often there will be
other signs of palsy in the area supplied by the oculomotor nerve. In externaloculomotor palsy, only the
extraocular muscles are affected (mydriasis willnot be present), whereas in complete oculomotor palsy, the inner
ciliary muscle and the sphincter pupillae muscle are also affected (internal
oph-thalmoplegia with loss of accommodation, mydriasis, and complete loss of
pupillary light reflexes).
❖ Myasthenia gravis (myogenic ptosis that is often bilateral and
may beasymmetrical) is associated with abnormal fatigue of the
striatedvextraocular muscles. Ptosis typically becomes more severe as the day
goes on.
❖ Sympathetic ptosis occurs in Horner’s palsy (ptosis, miosis, and enophthal-mos).
Rapidly opening and closing the eyelids
provokes ptosis in myasthenia gravis and simplifies the diagnosis.
Treatment:
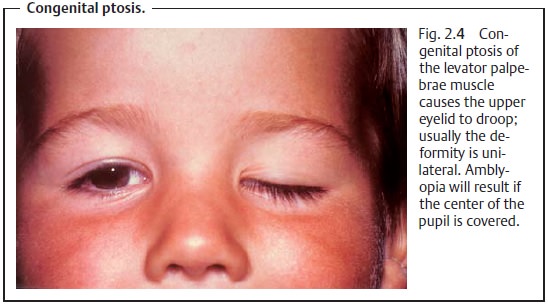
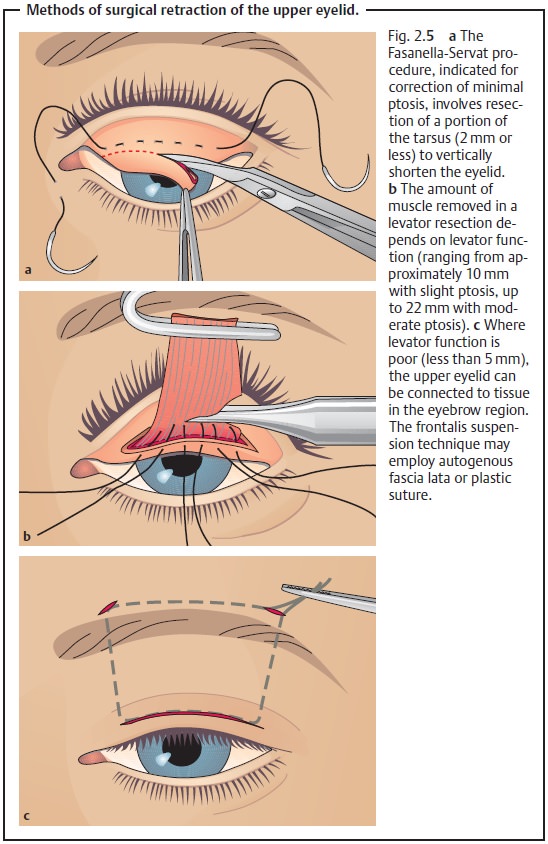
❖ Congenital ptosis: This involves surgical retraction of the upper eyelid(Fig. 2.5a – c), which should be undertaken as
quickly as possible when there is a risk of the affected eye developing a
visual impairment as a result of the ptosis.
❖ Acquired ptosis: Treatment depends on the cause. As palsies oftenresolvespontaneously, the patient should
be observed before resorting to surgica
intervention. Conservative treatment with
special eyeglasses may be suffi-cient even in irreversible cases.
Because of the risk of overcorrecting or
undercorrecting the disorder, several operations may be necessary.
Prognosis and complications: Prompt surgical intervention in congenitalptosis can prevent amblyopia. Surgical overcorrection of
the ptosis can lead to desiccation of the conjunctiva and cornea with ulceration as a result of incomplete
closure of the eyelids.
Entropion
Definition
Entropion is characterized by inward rotation
of the eyelid margin. The margin of the eyelid and eyelashes or even the outer
skin of the eyelid are in contact with the globe instead of only the
conjunctiva. The following forms are differ-entiated according to their origin
(see Etiology):
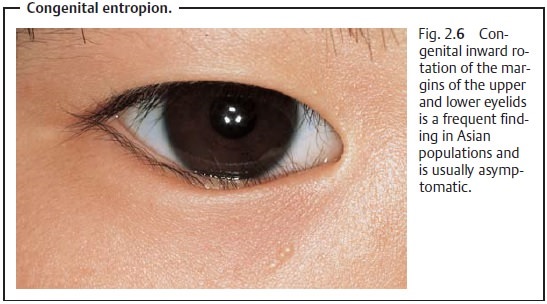
❖Congenital entropion (Fig. 2.6).
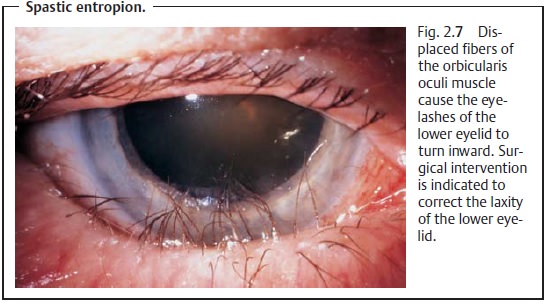
❖ Spastic entropion (Fig. 2.7).
❖ Cicatricial entropion.
Epidemiology: Congenital entropion occurs frequently among Asians but israre
among people of European descent, in whom the spastic and cicatricial forms are
more commonly encountered.
Etiology:
❖Congenital entropion: This results from fleshy thickening of the skin andorbicularis oculi muscle near the margin of the eyelid. Usually the lowereyelid is affected. This condition may persist into adulthood.
❖ Spastic entropion: Thisaffects
only the lower eyelid.A combination ofseveral pathogenetic factors of
varying severity is usually involved:
– The structures supporting the lower eyelid
(palpebral ligaments, tarsus, and eyelid retractor) may become lax with age,
causing the tarsus to tilt inward.
– This causes the fibers of the orbicularis
oculi muscle to override the normally superior margin of the eyelid,
intensifying the blepharospasm resulting from the permanent contact between the
eyelashes and the eyeball.
– Senile enophthalmos, usually occurring in
old age as a result of atrophy of the orbit fatty tissue, further contributes
to instability of the lower eyelid.
❖ Cicatricial entropion: This form of entropion is frequently the
result ofpostinfectious or post-traumatic tarsal contracture (such as trachoma;
burns and chemical injuries). Causes can also include allergic and toxic
reactions (pemphigus, Stevens-Johnson syndrome, and Lyell’s syndrome).
Symptoms and diagnostic considerations (see also etiology): Constantrubbing of the
eyelashes against the eyeball (trichiasis) represents a per-manent foreign-body
irritation of the conjunctiva which causes a blepharo-spasm (p. 93) that in
turn exacerbates the entropion. The chronically irritated conjunctiva is reddened,
and the eye fills with tears. Only congenital entropion is usually
asymptomatic.
Treatment:
❖ Congenital entropion: To the extent that any treatment is required,
it con-sists of measured, semicircular resection of skin and orbicularis oculi
muscle tissue that can be supplemented by everting sutures where indi-cated.
❖ Spastic entropion: Surgical management must be tailored to the
specificsituation. Usually treatment combines several techniques such as
shorten-ing the eyelid horizontally combined with weakening or diverting the
pre-tarsal fibers of the orbicularis oculi muscle and shortening the skin
verti-cally.
❖ Cicatricial entropion: The surgical management of this form is
identical tothat of spastic entropion.
An adhesive bandage may be applied to increase
tension on the eyelid for temporary relief of symptoms prior to surgery.
Prognosis and complications:
Congenital entropion is usually asymptomatic
and often resolves within the first few months of life.
❖ Spastic entropion: The prognosis is favorable with prompt
surgical inter-vention, although the disorder may recur. Left untreated,
spastic entropion entails a risk of damage to the corneal epithelium with
superin-fection which may progress to the complete clinical syndrome of a
serpigi-nous corneal ulcer.
❖ Cicatricial entropion: The prognosis is favorable with prompt
surgicalintervention (i.e., before any corneal changes occur).
Ectropion
Definition
Ectropion refers to the condition in which the
margin of the eyelid is turned away from the eyeball. This condition almost
exclusively affects the lower eye-lid. The following forms are differentiated
according to their origin (see also Etiology):
❖Congenital ectropion.
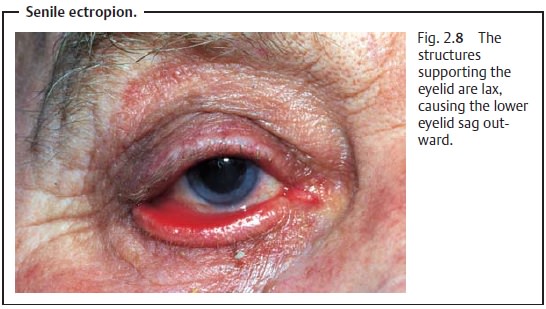
❖Senile ectropion.
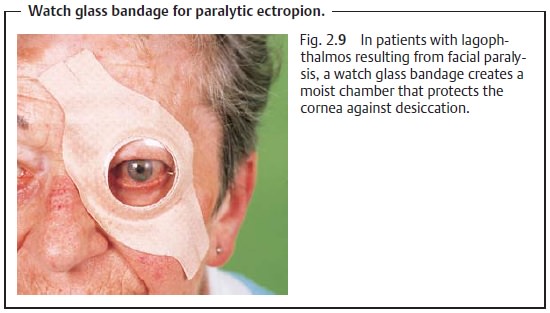
❖ Paralytic ectropion.
❖ Cicatricial ectropion.
Epidemiology: Senile ectropion is the most prevalent form; the paralytic
andcicatricial forms occur less frequently. Congenital ectropion is very rare
and is usually associated with other developmental anomalies of the eyelid and
face such as Franceschetti’s syndrome.
Etiology:
❖Congenital ectropion: See Epidemiology.
❖ Senile ectropion: The palpebral ligaments and tarsus may become
laxwith age, causing the tarsus to sag outward (Fig. 2.8).
❖ Paralytic ectropion: This is caused by facial paralysis with
resulting loss offunction of the orbicularis oculi muscle that closes the
eyelid.
❖ Cicatricial ectropion: Like cicatricial entropion, this form is usually asequela of infection or injury.
Symptoms and diagnostic considerations: Left untreated, incomplete clo-sure of the
eyelids can lead to symptoms associated with desiccation of the cornea
including ulceration from lagophthalmos. At the same time, the ever-sion of the
punctum causes tears to flow down across the cheek instead of draining into the
nose. Wiping away the tears increases the ectropion. This results in chronic
conjunctivitis and blepharitis.
Treatment:
❖Congenital ectropion: Surgery.
❖Senile ectropion: Surgery is indicated. A proven procedure is to
tighten thelower eyelid via a tarsal wedge resection followed by horizontal
tightening of the skin.
❖ Paralytic ectropion: Depending on the severity of the disorder,
artificialtear solutions, eyeglasses with an anatomic lateral protective
feature, or a “watch glass” bandage (Fig. 2.9) may be sufficient to prevent desiccation of the cornea. In
severe or irreversible cases, the lagophthalmos is treated surgically via a
lateral tarsorrhaphy.
❖ Cicatricial ectropion: Plastic surgery is often required to correct
the eyeliddeformity.
Prognosis: The prognosis is favorable when the disorder is treated
promptly.Sometimes several operations will be required. Surgery is more
difficult where scarring is present.
Trichiasis
Trichiasis refers to the rare postinfectious or post-traumatic inward turningof the eyelashes.
The deformity causes the
eyelashes to run against the con-junctiva and cornea, causing a permanent
foreign-body sensation, increased tear secretion, and chronic conjunctivitis.
The eyelash follicles can be oblit-erated by electrolysis. The disorder may
also be successfully treated by cryo-cautery epilation or surgical removal of
the follicle bed.
Blepharospasm
Definition
This refers to an involuntary spasmodic
contraction of the orbicularis oculi muscle supplied by the facial nerve.
Etiology: In addition to photosensitivity and increased tear
production,blepharospasm will also accompany inflammation or irritation of
the anteriorchamber. (Photosensitivity, epiphora, and blepharospasm form a
triad ofreactive clinical symptoms.) Causes of the disorder include extrapyramidaldisease such as
encephalitis or multiple sclerosis.
Trigeminal neuralgia or psy-chogenic
causes may also be present.
Symptoms: Clinical symptoms include spasmodically narrowed or
closedpalpebral fissures and lowered eyebrows.
Treatment: This depends on the cause of the disorder.Mild casescan be con-trolled well with muscle relaxants. Severe cases may require transection of the
fibers of the facial nerve supplying the orbicularis oculi muscle. The disorder
may also be successfully treated with repeated local injections of botulinum
toxin.
Prognosis: The prognosis isgoodwhere
acause-relatedtreatment is possible.Essential blepharospasm does not
respond well to treatment.
Related Topics