Chapter: Ophthalmology: The Eyelids
Disorders of the Skin and Margin of the Eyelid
Disorders of the Skin and Margin of the Eyelid
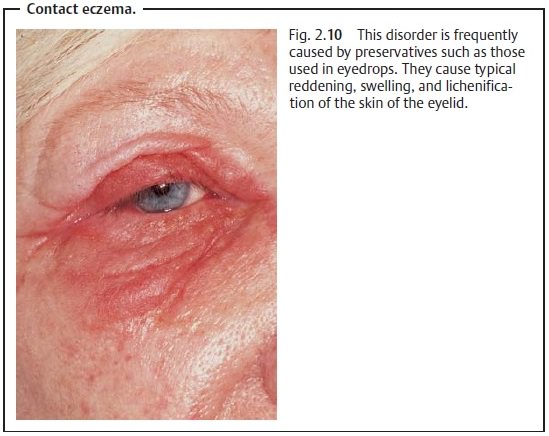
Contact Eczema
Epidemiology: Light-skinned patients and patients susceptible to allergy
arefrequently affected.
Etiology: Contact eczema is caused by an antigen – antibody reaction inpatients with intolerance to certain noxious substances. Cosmetics, adhesivebandages, or eyedrops and eye ointments are often responsible, particularlythe preservatives used in them such as benzalkonium chloride.
Symptoms: Reddening, swelling, lichenification, and severe itching of
theskin of the eyelid occur initially, followed by scaling of the indurated
skin with a sensation of tension (Fig. 2.10).
Treatment: This consists of eliminating the causative agent. (Allergy
testingmay be necessary.) Limited use of corticosteroids usually brings quick
relief of symptoms.
Prognosis: The prognosis is good if the cause can be identified.
Edema
Definition
This refers to swelling of the eyelid due to
abnormal collection of fluid in the subcutaneous tissue.
Epidemiology: Edema is a frequently encountered clinical symptom.
Etiology: The skin of the eyelid is affected intensively by infectious and
aller-gic processes. With the upper eyelid’s relatively thin skin and the loose
struc-ture of its subcutaneous
tissue, water can easily accumulate and cause edema.
Symptoms: Depending on the cause (Table 2.2), the intensity of swelling inthe eyelid will vary. The location of swelling is also influenced by gravity and can vary in intensity. For example, it may be more intense in the early morn-ing after the patient rises than in the evening (Fig. 2.11).
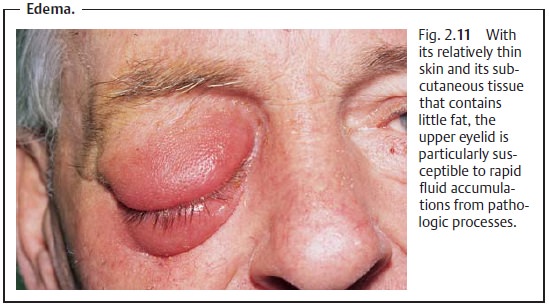
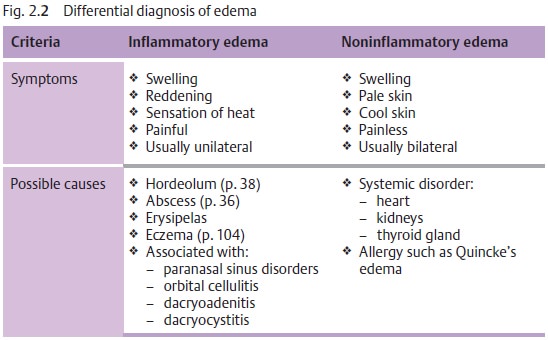
Table 2.2 shows the causes and differential diagnosis for inflammatory and noninflammatory edemas.
Treatment: This depends on the cause of the disorder.
Clinical course and prognosis: This depends on the underlying disorder.
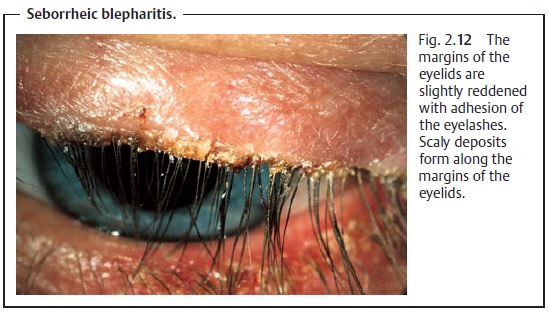
Seborrheic Blepharitis
Definition
This relatively frequent disorder is
characterized by scaly inflammation of the margins of the eyelids. Usually both
eyes are affected.
Etiology: There are oftenseveral
contributing causes. The constitution of theskin, seborrhea, refractive
anomalies, hypersecretion of the eyelid glands, and external stimuli such as
dust, smoke, and dry air in air-conditioned rooms often contribute to
persistent chronic inflammation.
Symptoms and diagnostic considerations: The margins of the eyelids usu-ally exhibit slight inflammatory changes such as
thickening. The eyelashes adhere due to the increased secretion from the glands
of the eyelids, and scalydeposits form
(Fig. 2.12). The disorder will often
be accompanied by chronicconjunctivitis.
Treatment: This depends on the cause of the disorder (see Etiology). Thescales and crusts can usually be softened with warm olive oil and then easily removed with a cotton-tipped applicator. In more severe cases, recommended treatment includes expressing the glands of the eyelid and local application of antibiotic ointment. Treatment with topical steroids may be indicated under certain conditions.
Prognosis: The prognosis is good although the clinical course of the
disorderis often quite protracted.
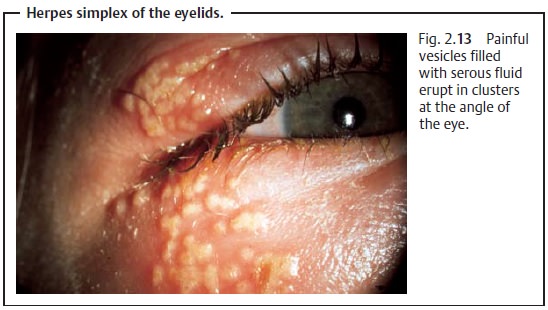
Herpes Simplex of the Eyelids
Definition
Acute, usually unilateral eyelid disorder
accompanied by skin and mucous membrane vesicles.
Etiology: Infection of the skin of the eyelids results when latent herpes
sim-plex viruses present in the tissue are activated by ultraviolet radiation. The virus spreads along sensory nerve fibers
from the trigeminal ganglion to the surface of the skin.
Symptoms: Typicalclustered eruptionsof
painfulvesiclesfilled with
serousfluid frequently occur at the junction of mucous membranes and skin (Fig.
2.13). Later the vesicles dry and
crusts form. Lesions heal without scar-ring. The disorder is usually
unilateral.
Treatment: Topical use of virostatic agents is indicated. The patient
shouldavoid intense ultraviolet radiation as a prophylactic measure against
recur-rence.
Prognosis: The prognosis is good, although the disorder frequently recurs.
Herpes Zoster Ophthalmicus
Definition
Facial rash caused by the varicella-zoster
virus.
Epidemiology: The disorder usually affects immunocompromised personsbetween
the ages of 40 and 60 who have underlying disorders.
Etiology: The disorder is caused by the varicella-zoster virus, which
initiallymanifests itself as chickenpox. If activation or reinfection occurs,
the latent neurotropic viruses present in the body can lead to the clinical
syndrome of herpes zoster ophthalmicus (Fig. 2.14).
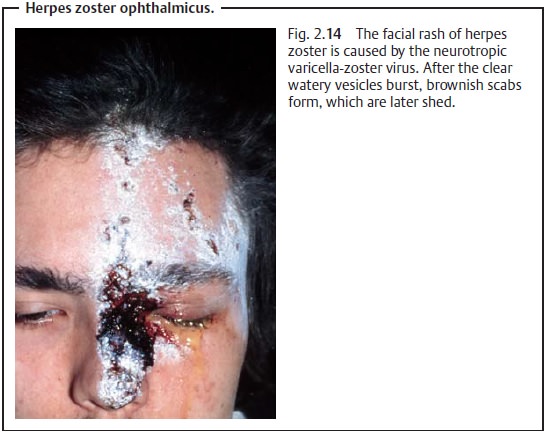
Symptoms: The incubation period is 7 – 18 days, after whichsevere painoccurs in the area supplied by the first branch of the trigeminal nerve (the ophthalmic nerve with its frontal, lacrimal, and nasociliary branches). Prodro-mal symptoms of erythema, swelling, photosensitivity, and lacrimation mayoccur before the characteristic clear watery vesicles appear. The vesicles burst and brownish scabs form, which are later shed. Blepharitis is also present in 50 – 70% of all cases. As herpes zoster usually affects immunocompromised persons, the patient should be examined for a possible underlying disorder.
The skin sensitivity at the tip of the nose
should be evaluated on both sides in the initial stage of the disorder.
Decreased sensitivity to touch suggests involvement of the nasociliary branch
of the ophthalmic nerve, which can lead to severe intraocular inflammation.
Treatment: This includes topical virostatic agents and systemic acyclovir.
Complications: Involvement of the nasociliary branch of the ophthalmicnerve can
lead to severe intraocular inflammation.
Prognosis: The skin lesions heal within three to four weeks; scars
mayremain. Often neuralgiform pain and hypesthesia may persist.
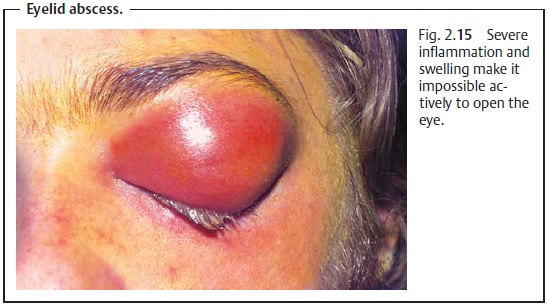
Eyelid Abscess
Definition
Circumscribed collection of pus with severe
inflammation, swelling, and sub-sequent fluctuation.
Etiology: An abscess of the upper or lower eyelid can form as a sequela
ofminor trauma, insect sting, or spread of inflammation from the paranasal
sinuses.
Symptoms: The severe inflammation and swelling often make it impossibleactively to open the eye (Fig. 2.15). The contents of the abscess can fluctuate during the clinical course of the disorder. Spontaneous perforation with pus drainage can occur.
Treatment: Oral or intravenous antibiotics and dry heat are indicated. A
stabincision can relieve tension at the onset of fluctuation.
Prognosis: The prognosis is generally good.
Orbital cellulitis or cavernous sinus
thrombosis can occasionally occur as a sequela of eyelid abscess, especially
when located at the medial angle of the eye. This represents a life-threatening
complication.
Tick Infestation of the Eyelids
Ticks have been known to infest the eyelids.
They are thought to be vectors of borreliosis and can cause encephalitis.
Treatment consists of mechanical removal of the parasites.
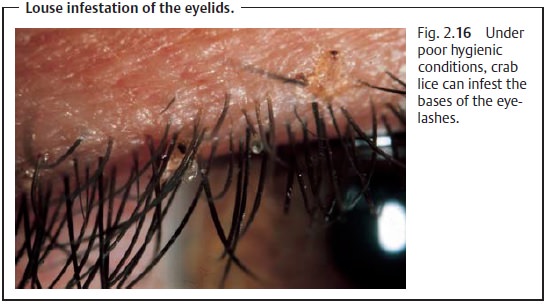
Louse Infestation of the Eyelids
This refers to infestation of the margin
of the eyelid with crab lice as a result of poor hygienic conditions. The small oval nits
frequently hang from the eye-lashes (Fig. 2.16), causing inflammation of the margin of the
eyelid with severe itching. Mechanical
removal with forceps is a time consuming but effec-tive treatment. Application of a 2% mercury precipitate
ointment over an extended period of time is also effective.
Related Topics