Chapter: Medical Surgical Nursing: Management of Patients With Intestinal and Rectal Disorders
Constipation - Abnormalities of Fecal Elimination
Abnormalities of Fecal Elimination
Changes
in patterns of fecal elimination are symptoms of func-tional disorders or
disease of the GI tract. The most common changes seen are constipation,
diarrhea, and fecal incontinence. The nurse should be aware of the possible
causes and thera-peutic management of these problems and of nursing manage-ment
techniques. Education is important for patients with these abnormalities.
CONSTIPATION
Constipation is a term used to describe an abnormal
infrequencyor irregularity of defecation, abnormal hardening of stools that
makes their passage difficult and sometimes painful, a decrease in stool
volume, or retention of stool in the rectum for a prolonged period. Any
variation from normal habits may be considered a problem.
Constipation
can be caused by certain medications (ie, tran-quilizers, anticholinergics,
antidepressants, antihypertensives, opioids, antacids with aluminum, and iron);
rectal or anal disor-ders (eg, hemorrhoids, fissures); obstruction (eg, cancer
of the bowel); metabolic, neurologic, and neuromuscular conditions (eg,
diabetes mellitus, Hirschsprung’s disease, Parkinson’s dis-ease, multiple
sclerosis); endocrine disorders (eg, hypothy-roidism, pheochromocytoma); lead
poisoning; and connective tissue disorders (eg, scleroderma, lupus
erythematosus). Consti-pation is a major problem for patients taking opioids
for chronic pain. Diseases of the colon commonly associated with constipation
are irritable bowel syndrome (IBS) and diverticular disease. Constipation can
also occur with an acute disease process in the abdomen (eg, appendicitis).
Other
causes include weakness, immobility, debility, fatigue, and an inability to
increase intra-abdominal pressure to facilitate the passage of stools, as
occurs with emphysema. Many people de-velop constipation because they do not
take the time to defecate or they ignore the urge to defecate. In the United
States, consti-pation is also a result of dietary habits (ie, low consumption
of fiber and inadequate fluid intake), lack of regular exercise, and a
stress-filled life.
Perceived
constipation can also be a problem. This subjective problem occurs when an
individual’s bowel elimination pattern is not consistent with what he or she
perceives as normal. Chronic laxative use is attributed to this problem and is
a major health concern in the United States, especially among the elderly
population.
Pathophysiology
The
pathophysiology of constipation is poorly understood, but it is thought to
include interference with one of three major func-tions of the colon: mucosal
transport (ie, mucosal secretions fa-cilitate the movement of colon contents),
myoelectric activity (ie, mixing of the rectal mass and propulsive actions), or
the processes of defecation. Any of the causative factors previously identified
can interfere with any of these three processes.
The
urge to defecate is stimulated normally by rectal disten-tion, which initiates
a series of four actions: stimulation of the in-hibitory rectoanal reflex,
relaxation of the internal sphincter muscle, relaxation of the external
sphincter muscle and muscles in the pelvic region, and increased
intra-abdominal pressure. Interference with any of these processes can lead to
constipation.If all organic causes are eliminated, idiopathic constipation is
diagnosed.
If the
urge to defecate is ignored, the rectal mucous membrane and musculature become
insensitive to the presence of fecal masses, and consequently, a stronger
stimulus is required to produce the necessary peristaltic rush for defecation.
The ini-tial effect of fecal retention is to produce irritability of the colon,
which at this stage frequently goes into spasm, especially after meals, giving
rise to colicky midabdominal or low abdominal pains. After several years of
this process, the colon loses muscular tone and becomes essentially
unresponsive to normal stimuli. Atony or decreased muscle tone occurs with
aging. This also leads to constipation because the stool is retained for longer
periods.
Clinical Manifestations
Clinical
manifestations include abdominal distention, borborygmus (ie, gurgling or
rumbling sound caused by passage of gas through the intestine), pain and
pressure, decreased appetite, headache, fa-tigue, indigestion, a sensation of
incomplete emptying, straining at stool, and the elimination of small-volume,
hard, dry stools.
Assessment and Diagnostic Findings
Chronic
constipation is usually considered idiopathic, but sec-ondary causes should be
excluded. In patients with severe, in-tractable constipation, further
diagnostic testing is needed (Wong, 1999). The diagnosis of constipation is
based on results of the pa-tient’s history, physical examination, possibly a
barium enema or sigmoidoscopy, and stool testing for occult blood. These tests
are completed to determine whether this symptom results from spasm or narrowing
of the bowel. Anorectal manometry (ie, pressure studies) may be performed to
determine malfunction of the mus-cle and sphincter. Defecography and bowel
transit studies can also assist in the diagnosis.
Complications
Complications of constipation include
hypertension, fecal im-paction, hemorrhoids and fissures, and megacolon.
Increased arte-rial pressure can occur with defecation. Straining at stool,
which results in the Valsalva maneuver (ie, forcibly exhaling with the glot-tis
closed), has a striking effect on arterial blood pressure. During active
straining, the flow of venous blood in the chest is temporar-ily impeded
because of increased intrathoracic pressure. This pres-sure tends to collapse
the large veins in the chest. The atria and the ventricles receive less blood,
and consequently less is delivered by the systolic contractions of the left
ventricle. The cardiac output is decreased, and there is a transient drop in
arterial pressure. Almost immediately after this period of hypotension, a rise
in arterial pres-sure occurs; the pressure is elevated momentarily to a point
far ex-ceeding the original level (ie, rebound phenomenon). In patients with
hypertension, this compensatory reaction may be exaggerated greatly, and the
peaks of pressure attained may be dangerously high—sufficient to rupture a
major artery in the brain or elsewhere.
Fecal
impaction occurs when an accumulated mass of dry feces cannot be expelled. The
mass may be palpable on digital examina-tion, may produce pressure on the
colonic mucosa that results in ulcer formation, and frequently may cause
seepage of liquid stools.
Hemorrhoids
and anal fissures can develop as a result of con-stipation. Hemorrhoids develop as a result of
perianal vascular congestion caused by straining. Anal fissures may result from
the passage of the hard stool through the anus, tearing the lining of the anal
canal.
Megacolon
is a dilated and atonic colon caused by a fecal mass that obstructs the passage
of colon contents. Symptoms include constipation, liquid fecal incontinence,
and abdominal disten-tion. Megacolon can lead to perforation of the bowel.
Gerontologic Considerations
Physician
visits for constipation are more frequent by individuals 65 years of age or
older (Yamada et al., 1999). Elderly people re-port problems with constipation
five times more frequently than younger people. A number of factors contribute
to this increased frequency. People who have loose-fitting dentures or have
lost their teeth have difficulty chewing and frequently choose soft, processed
foods that are low in fiber. Convenience foods, also low in fiber, are widely
used by those who have lost interest in eating. Some older people reduce their
fluid intake if they are not eating regular meals. Lack of exercise and
prolonged bed rest also con-tribute to constipation by decreasing abdominal
muscle tone and intestinal motility as well as anal sphincter tone. Nerve
impulses are dulled, and there is decreased sensation to defecate. Many older
people who overuse laxatives in an attempt to have a daily bowel movement become
dependent on them.
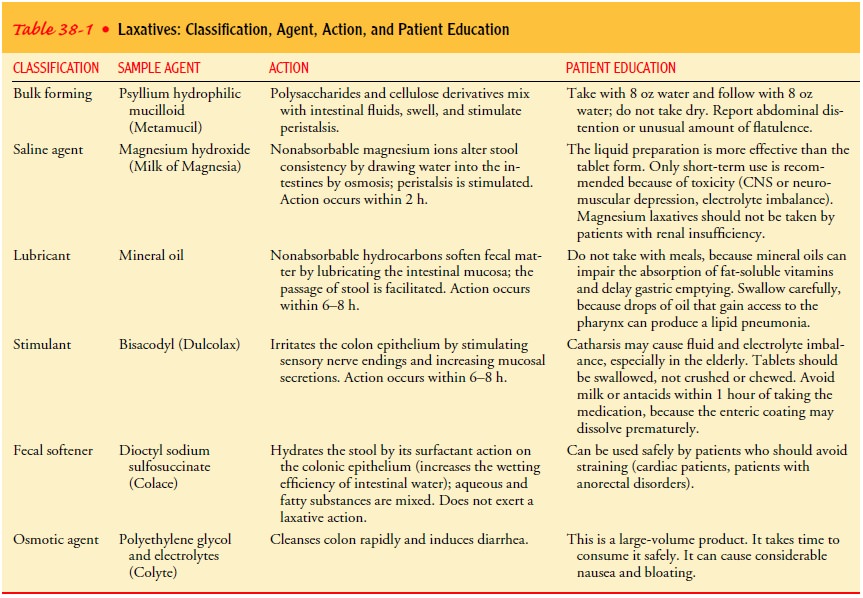
Medical Management
Treatment
is aimed at the underlying cause of constipation and includes education, bowel
habit training, increased fiber and fluid intake, and judicious use of
laxatives. Management may also in-clude discontinuing laxative abuse. Routine
exercise to strengthen abdominal muscles is encouraged. Biofeedback is a
technique that can be used to help patients learn to relax the sphincter
mecha-nism to expel stool. Daily addition to the diet of 6 to 12 tea-spoonfuls
of unprocessed bran is recommended, especially for the treatment of
constipation in the elderly. If laxative use is necessary, one of the following
may be prescribed: bulk-forming agents, saline and osmotic agents, lubricants,
stimulants, or fecal soften-ers. The physiologic action and patient education
information re-lated to these laxatives are identified in Table 38-1. Enemas
and rectal suppositories are generally not recommended for constipa-tion and
should be reserved for the treatment of impaction or for preparing the bowel
for surgery or diagnostic procedures. If long-term laxative use is necessary, a
bulk-forming agent may be pre-scribed in combination with an osmotic laxative.
Doctors
prescribe the use of specific medications to enhance colonic transit by
increasing propulsive motor activity. Further studies are being carried out on
cholinergic agents (eg, bethane-chol), cholinesterase inhibitors (eg,
neostigmine), and prokinetic agents (eg, metoclopramide) to determine the role
these agents can play in treating constipation (Yamada et al., 1999).
Nursing Management
The
nurse elicits information about the onset and duration of con-stipation,
current and past elimination patterns, the patient’s ex-pectation of normal
bowel elimination, and lifestyle information (eg, exercise and activity level,
occupation, food and fluid intake, and stress level) during the health history
interview. Past medical and surgical history, current medications, and laxative
and enema use are important, as is information about the sensation of rectal
pressure or fullness, abdominal pain, excessive straining at defeca-tion, and
flatulence.
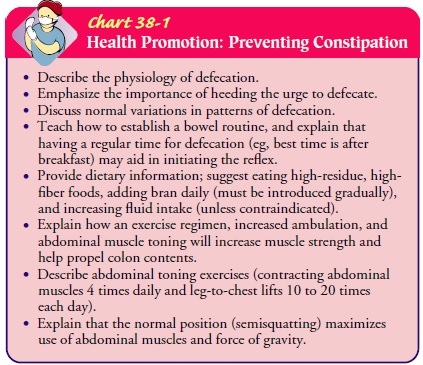
Patient
education and health promotion are important functions of the nurse (Chart
38-1). After the health history is obtained, the nurse sets specific goals for
teaching. Goals for the patient include restoring or maintaining a regular
pattern of elimination, ensur-ing adequate intake of fluids and high-fiber
foods, learning about methods to avoid constipation, relieving anxiety about
bowel elimination patterns, and avoiding complications.
Related Topics