Chapter: Medical Surgical Nursing: Management of Patients With Intestinal and Rectal Disorders
Diverticular Disease - Acute Inflammatory Intestinal Disorders
DIVERTICULAR
DISEASE
A diverticulum is a saclike outpouching
of the lining of the bowel that extends through a defect in the muscle layer.
Diverticula may occur anywhere along the GI tract. Diverticulosis exists when mul-tiple diverticula are present
without inflammation or symptoms. Diverticular disease of the colon is very
common in developed countries, and its prevalence increases with age. More than
35% of Americans older than 60 years of age have diverticulosis. The incidence
increases to 50% among those in the ninth decade of life (Keighley, 1999). Diverticulitis results when food and
bacteria retained in a diverticulum produce infection and inflammation that can
impede drainage and lead to perforation or abscess for-mation. Diverticulitis
is most common (95%) in the sigmoid colon. Approximately 20% of patients with
diverticulosis have di-verticulitis at some point. A congenital predisposition
is suspected when the disorder occurs in those younger than 40 years of age. A
low intake of dietary fiber is considered a predisposing factor, but the exact
cause is unknown. Diverticulitis may occur in acute at-tacks or may persist as
a continuing, smoldering infection. Most patients remain entirely asymptomatic.
The symptoms manifested generally result from its potential
complications—abscesses, fistu-las, obstruction, and hemorrhage.
Pathophysiology
A
diverticulum forms when the mucosa and submucosal layers of the colon herniate
through the muscular wall because of high intraluminal pressure, low volume in
the colon (ie, fiber-deficient contents), and decreased muscle strength in the
colon wall (ie, muscular hypertrophy from hardened fecal masses). Bowel
contents can accumulate in the diverticulum and decompose, causing inflammation
and infection. A diverticulum can become ob-structed and then inflamed if the
obstruction continues. The in-flammation tends to spread to the surrounding
bowel wall, giving rise to irritability and spasticity of the colon (ie,
diverticulitis). Ab-scesses develop and may eventually perforate, leading to
peritoni-tis and erosion of the blood vessels (arterial) with bleeding.
Clinical Manifestations
Chronic
constipation often precedes the development of diver-ticulosis by many years.
Frequently, no problematic symptoms occur with diverticulosis. Signs of acute
diverticulosis are bowel irregularity and intervals of diarrhea, abrupt onset
of crampy pain in the left lower quadrant of the abdomen, and a low-grade
fever. The patient may have nausea and anorexia, and some bloating or abdominal
distention may occur. With repeated local inflamma-tion of the diverticula, the
large bowel may narrow with fibrotic strictures, leading to cramps, narrow
stools, and increased con-stipation. Weakness, fatigue, and anorexia are common
symp-toms. With acute diverticulosis, the patient reports mild to severe pain
in the lower left quadrant. The condition, if untreated, can lead to
septicemia.
Assessment and Diagnostic Findings
A CT
scan is the procedure of choice and can reveal abscesses. Ab-dominal x-ray
findings may demonstrate free air under the di-aphragm if a perforation has
occurred from the diverticulitis. Diverticulosis may be diagnosed using barium
enema, which shows narrowing of the colon and thickened muscle layers. If there
are symptoms of peritoneal irritation and when the diag-nosis is
diverticulitis, barium enema is contraindicated because of the potential for
perforation.
A colonoscopy may be performed if there is no acute diver-ticulitis or after resolution of an acute episode to visualize the colon, determine the extent of the disease, and rule out other con-ditions. Laboratory tests that assist in diagnosis include a com-plete blood cell count, revealing an elevated leukocyte count, and elevated sedimentation rate.
Complications
Complications of diverticulitis include
peritonitis, abscess forma-tion, and bleeding. If an abscess develops, the
associated findings are tenderness, a palpable mass, fever, and leukocytosis.
An in-flamed diverticulum that perforates results in abdominal pain lo-calized
over the involved segment, usually the sigmoid; local abscess or peritonitis
follows. Abdominal pain, a rigid boardlike abdomen, loss of bowel sounds, and
signs and symptoms of shock occur with peritonitis. Noninflamed or slightly
inflamed diverticula may erode areas adjacent to arterial branches, causing
massive rectal bleeding.
Gerontologic Considerations
The
incidence of diverticular disease increases with age because of degeneration
and structural changes in the circular muscle layers of the colon and because
of cellular hypertrophy. The symptoms are less pronounced in the elderly than
in other adults. The elderly may not have abdominal pain until infection
occurs. They may delay re-porting symptoms because they fear surgery or are
afraid that they may have cancer. Blood in the stool is overlooked frequently,
espe-cially in the elderly, because of a failure to examine the stool or the
inability to see changes because of diminished vision.
Medical Management
DIETARY AND MEDICATION MANAGEMENT
Diverticulitis
can usually be treated on an outpatient basis with diet and medicine therapy.
When symptoms occur, rest, analgesics, and antispasmodics are recommended.
Initially, the diet is clear liquid until the inflammation subsides; then, a
high-fiber, low-fat diet is recommended. This type of diet helps to increase
stool volume, decrease colonic transit time, and reduce intraluminal pressure.
Antibiotics are prescribed for 7 to 10 days. A bulk-forming laxative also is
prescribed.
In
acute cases of diverticulitis with significant symptoms, hos-pitalization is
required. Hospitalization is often indicated for those who are elderly,
immunocompromised, or taking corticosteroids. Withholding oral intake,
administering intravenous fluids, and in-stituting nasogastric suctioning if
vomiting or distention occurs rests the bowel. Broad-spectrum antibiotics are
prescribed for 7 to 10 days. An opioid is prescribed for pain relief; morphine
is not used because it increases segmentation and intraluminal pressures. Oral
intake is increased as symptoms subside. A low-fiber diet may be necessary
until signs of infection decrease.
Antispasmodics
such as propantheline bromide (Pro-Banthine) and oxyphencyclimine (Daricon) may
be prescribed. Normal stools can be achieved by using bulk preparations
(Metamucil) or stool softeners (Colace), by instilling warm oil into the
rectum, or by in-serting an evacuant suppository (Dulcolax). Such a
prophylactic plan can reduce the bacterial flora of the bowel, diminish the
bulk of the stool, and soften the fecal mass so that it moves more easily
through the area of inflammatory obstruction.
SURGICAL MANAGEMENT
Although
acute diverticulitis usually subsides with medical man-agement, immediate
surgical intervention is necessary if complica-tions (eg, perforation,
peritonitis, abscess formation, hemorrhage, obstruction) occur. Alternatively,
when the acute episode of diver-ticulitis resolves, surgery may be recommended
to prevent repeated episodes. Two types of surgery are considered:
•
One-stage resection in which the inflamed area is
removed and a primary end-to-end anastomosis is completed
•
Multiple-staged procedures for complications such
as ob-struction or perforation (Fig. 38-3)
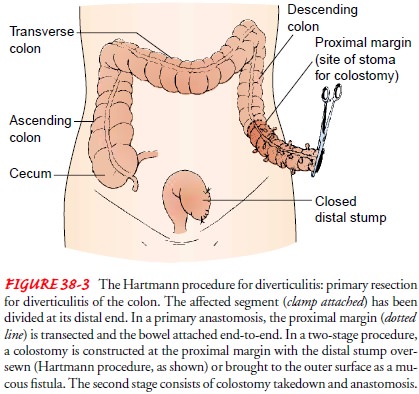
The
type of surgery performed depends on the extent of com-plications found during
surgery. When possible, the area of di-verticulitis is resected and the
remaining bowel is joined end to end (ie, primary resection and end-to-end
anastomosis). This is performed through traditional surgical or
laparoscopically as-sisted colectomy. A two-stage resection may be performed in
which the diseased colon is resected (as in a one-stage procedure) but no
anastomosis is performed; both ends of the bowel are brought out onto the
abdomen as stomas. This “double-barrel” colostomy is then reanastomosed in a
later procedure.
Related Topics