Chapter: Medical Surgical Nursing: Management of Patients With Intestinal and Rectal Disorders
Peritonitis - Acute Inflammatory Intestinal Disorders
PERITONITIS
Peritonitis is inflammation of the
peritoneum, the serous mem-brane lining the abdominal cavity and covering the
viscera. Usually, it is a result of bacterial infection; the organisms come
from diseases of the GI tract or, in women, from the internal reproductive
organs. Peritonitis can also result from external sources such as injury or
trauma (eg, gunshot wound, stab wound) or an inflammation that extends from an
organ outside the peritoneal area, such as the kid-ney. The most common
bacteria implicated are Escherichia
coli,Klebsiella, Proteus, and
Pseudomonas. Inflammation and paralyticileus are the direct effects of the
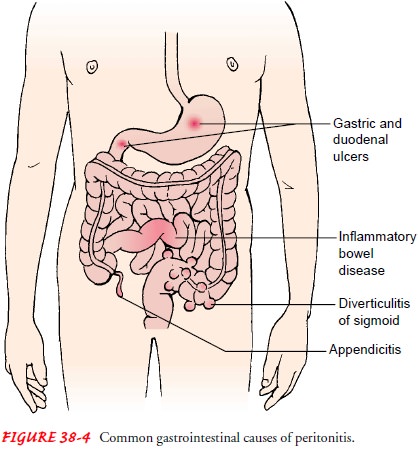
infection. Other common causes of peritonitis are appendicitis, perforated
ulcer, diverticulitis, and bowel perforation (Fig. 38-4). Peritonitis may also
be associated with abdominal surgical procedures and peritoneal dialysis
Pathophysiology
Peritonitis
is caused by leakage of contents from abdominal or-gans into the abdominal
cavity, usually as a result of inflamma-tion, infection, ischemia, trauma, or
tumor perforation. Bacterial proliferation occurs. Edema of the tissues
results, and exudation of fluid develops in a short time. Fluid in the
peritoneal cavity be-comes turbid with increasing amounts of protein, white
blood cells, cellular debris, and blood. The immediate response of the
intestinal tract is hypermotility, soon followed by paralytic ileus with an
accumulation of air and fluid in the bowel.
Clinical Manifestations
Symptoms
depend on the location and extent of the inflamma-tion. The early clinical
manifestations of peritonitis frequently are the symptoms of the disorder causing
the condition. At first, a diffuse type of pain is felt. The pain tends to
become constant, localized, and more intense near the site of the inflammation.
Movement usually aggravates it. The affected area of the abdomen becomes
extremely tender and distended, and the muscles become rigid. Rebound
tenderness and paralytic ileus may be present. Usually, nausea and vomiting
occur and peristalsis is diminished. The temperature and pulse rate increase,
and there is almost always an elevation of the leukocyte count.
Assessment and Diagnostic Findings
The
leukocyte count is elevated. The hemoglobin and hematocrit levels may be low if
blood loss has occurred. Serum electrolyte stud-ies may reveal altered levels
of potassium, sodium, and chloride.
An
abdominal x-ray is obtained, and findings may show air and fluid levels as well
as distended bowel loops. A CT scan of the abdomen may show abscess formation.
Peritoneal aspiration and culture and sensitivity studies of the aspirated
fluid may reveal infection and identify the causative organisms.
Complications
Frequently,
the inflammation is not localized and the whole ab-dominal cavity becomes
involved in a generalized sepsis. Sepsis is the major cause of death from
peritonitis. Shock may result from septicemia or hypovolemia. The inflammatory
process may cause intestinal obstruction, primarily from the development of
bowel adhesions.
The
two most common postoperative complications are wound evisceration and abscess
formation. Any suggestion from the pa-tient that an area of the abdomen is
tender or painful or “feels as if something just gave way” must be reported.
The sudden oc-currence of serosanguineous wound drainage strongly suggests
wound dehiscence.
Medical Management
Fluid,
colloid, and electrolyte replacement is the major focus of medical management.
The administration of several liters of an iso-tonic solution is prescribed.
Hypovolemia occurs because massive amounts of fluid and electrolytes move from
the intestinal lumen into the peritoneal cavity and deplete the fluid in the
vascular space.
Analgesics
are prescribed for pain. Antiemetics are adminis-tered as prescribed for nausea
and vomiting. Intestinal intubation and suction assist in relieving abdominal
distention and in pro-moting intestinal function. Fluid in the abdominal cavity
can cause pressure that restricts expansion of the lungs and causes
res-piratory distress. Oxygen therapy by nasal cannula or mask can promote
adequate oxygenation, but airway intubation and ven-tilatory assistance occasionally
are required.
Massive
antibiotic therapy is usually initiated early in the treatment of peritonitis.
Large doses of a broad-spectrum anti-biotic are administered intravenously
until the specific organism causing the infection is identified and the
appropriate antibiotic therapy can be initiated.
Surgical
objectives include removing the infected material and correcting the cause.
Surgical treatment is directed toward exci-sion (ie, appendix), resection with
or without anastomosis (ie, in-testine), repair (ie, perforation), and drainage
(ie, abscess). With extensive sepsis, a fecal diversion may need to be created.
Nursing Management
Ongoing
assessment of pain, vital signs, GI function, and fluid and electrolyte balance
is important. The nurse reports the nature of the pain, its location in the
abdomen, and any shifts in location. Ad-ministering analgesic medication and
positioning the patient for comfort are helpful in decreasing pain. The patient
is placed on the side with knees flexed; this position decreases tension on the
ab-dominal organs. Accurate recording of all intake and output and central
venous pressure assists in calculating fluid replacement. The nurse administers
and monitors closely intravenous fluids.
Signs
that indicate that peritonitis is subsiding include a de-crease in temperature
and pulse rate, softening of the abdomen, return of peristaltic sounds, passing
of flatus, and bowel move-ments. The nurse increases fluid and food intake
gradually and reduces parenteral fluids as prescribed. A worsening clinical
con-dition may indicate a complication, and the nurse must prepare the patient
for emergency surgery.
Drains
are frequently inserted during the surgical procedure, and the nurse must
observe and record the character of the drainage postoperatively. Care must be
taken when moving and turning the patient to prevent the drains from being
dislodged. It is also important for the nurse to prepare the patient and family
for dis-charge by teaching the patient to care for the incision and drains if
the patient will be sent home with the drains still in place.
Related Topics