Chapter: Medical Surgical Nursing: Management of Patients With Intestinal and Rectal Disorders
Conditions of Malabsorption - Abnormalities of Fecal Elimination
CONDITIONS
OF MALABSORPTION
Malabsorption is the inability of the digestive system to
absorbone or more of the major vitamins (especially vitamin B12), min-erals (ie, iron
and calcium), and nutrients (ie, carbohydrates, fats, and proteins).
Interruptions in the complex digestive process may occur anywhere in the
digestive system and cause decreased ab-sorption. Diseases of the small
intestine are the most common cause of malabsorption.
Pathophysiology
The
conditions that cause malabsorption can be grouped into the following
categories:
•
Mucosal (transport) disorders causing generalized
mal-absorption (eg, celiac sprue, regional enteritis, radiation enteritis)
•
Infectious diseases causing generalized
malabsorption (eg, small bowel bacterial overgrowth, tropical sprue, Whipple’s
disease)
•
Luminal problems causing malabsorption (eg, bile
acid defi-ciency, Zollinger-Ellison syndrome, pancreatic insufficiency)
•
Postoperative malabsorption (eg, after gastric or
intestinal resection)
•
Disorders that cause malabsorption of specific
nutrients (eg, disaccharidase deficiency leading to lactose intolerance)
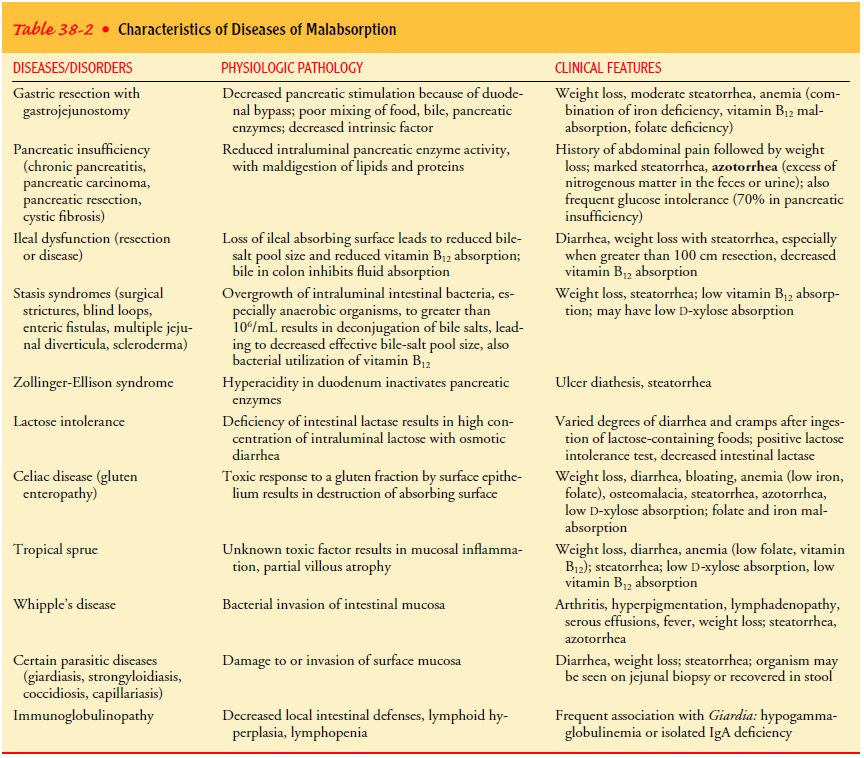
Table
38-2 lists the clinical and pathologic aspects of malabsorptive diseases.
Clinical Manifestations
The
hallmarks of malabsorption syndrome from any cause are di-arrhea or frequent,
loose, bulky, foul-smelling stools that have in-creased fat content and are
often grayish. Patients often have associated abdominal distention, pain,
increased flatus, weakness, weight loss, and a decreased sense of well-being.
The chief result of malabsorption is malnutrition, manifested by weight loss
and other signs of vitamin and mineral deficiency (eg, easy bruising,
osteoporosis, anemia). Patients with a malabsorption syndrome, if untreated,
become weak and emaciated because of starvation and dehydration. Failure to
absorb the fat-soluble vitamins A, D, and K causes a corresponding
avitaminosis.
Assessment and Diagnostic Findings
Several
diagnostic tests may be prescribed, including stool studies for quantitative
and qualitative fat analysis, lactose tolerance tests, D-xylose absorption tests, and Schilling tests. The
hydrogen breath test that is used to evaluate carbohydrate absorption is
performed if carbohydrate malabsorption is suspected. En-doscopy with biopsy of
the mucosa is the best diagnostic tool. Biopsy of the small intestine is
performed to assay enzyme activity or to identify infection or destruction of
mucosa. Ultrasound studies, CT scans, and x-ray findings can reveal pancreatic
or intestinal tumors that may be the cause. A complete blood cell count is used
to detect anemia. Pancreatic function tests can assist in the diagnosis of
specific disorders.
Medical Management
Intervention
is aimed at avoiding dietary substances that ag-gravate malabsorption and at
supplementing nutrients that have been lost. Common supplements are
water-soluble vitamins (eg, B12, folic acid), fat-soluble vitamins (ie, A, D, and
K), and minerals (eg, calcium, iron). Primary disease states may be man-aged
surgically or nonsurgically. Dietary therapy is aimed at re-ducing gluten
intake in patients with celiac sprue. Folic acid supplements are prescribed for
patients with tropical sprue. Anti-biotics (eg, tetracycline, ampicillin) are
sometimes needed in the treatment of tropical sprue and bacterial overgrowth
syndromes. Antidiarrheal agents may be used to decrease intestinal spasms.
Parenteral fluids may be necessary to treat dehydration.
Nursing Management
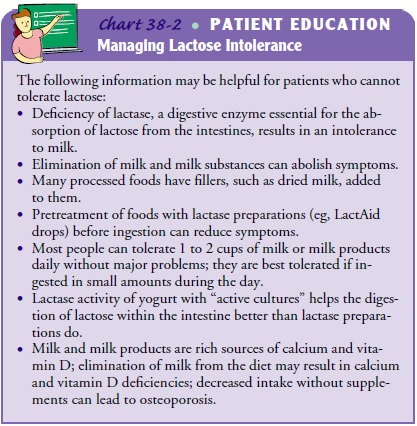
The
nurse provides patient and family education regarding diet and the use of
nutritional supplements (Chart 38-2). It is impor-tant to monitor patients with
diarrhea for fluid and electrolyte imbalances. The nurse conducts ongoing
assessments to deter-mine if the clinical manifestations related to the
nutritional deficits have abated. Patient education includes information about
the risk of osteoporosis related to malabsorption of calcium.
Related Topics