Chapter: Medical Surgical Nursing: Management of Patients With Intestinal and Rectal Disorders
Nursing Process: The Patient With Colorectal Cancer
NURSING
PROCESS:THE PATIENT WITH COLORECTAL CANCER
Assessment
The nurse completes a health history to obtain information about fatigue, abdominal or rectal pain (eg, location, frequency, dura-tion, association with eating or defecation), past and present elim-ination patterns, and characteristics of stool (eg, color, odor, consistency, presence of blood or mucus).
Additional informa-tion includes a history of IBD
or colorectal polyps, a family his-tory of colorectal disease, and current
medication therapy. The nurse identifies dietary habits, including fat and
fiber intake, as well as amounts of alcohol consumed. The nurse describes and
documents a history of weight loss.
Assessment
includes auscultating the abdomen for bowel sounds and palpating the abdomen
for areas of tenderness, dis-tention, and solid masses. Stool specimens are
inspected for char-acter and presence of blood.
Diagnosis
NURSING DIAGNOSES
Based
on the assessment data, the major nursing diagnoses may include the following:
ŌĆó
Imbalanced nutrition, less than body requirements,
related to nausea and anorexia
ŌĆó
Risk for deficient fluid volume related to vomiting
and de-hydration
ŌĆó
Anxiety related to impending surgery and the diagnosis
of cancer
ŌĆó
Risk for ineffective therapeutic regimen management
re-lated to knowledge deficit concerning the diagnosis, the sur-gical
procedure, and self-care after discharge
ŌĆó
Impaired skin integrity related to the surgical
incisions (ab-dominal and perianal), the formation of a stoma, and fre-quent
fecal contamination of peristomal skin
ŌĆó
Disturbed body image related to colostomy
ŌĆó
Ineffective sexuality patterns related to presence
of ostomy and changes in body image and self-concept
COLLABORATIVE PROBLEMS/POTENTIAL COMPLICATIONS
Potential
complications that may develop include the following:
ŌĆó
Intraperitoneal infection
ŌĆó
Complete large bowel obstruction
ŌĆó
GI bleeding
ŌĆó
Bowel perforation
ŌĆó
Peritonitis, abscess, and sepsis
Planning and Goals
The
major goals for the patient may include attainment of opti-mal level of
nutrition; maintenance of fluid and electrolyte bal-ance; reduction of anxiety;
learning about the diagnosis, surgical procedure, and self-care after
discharge; maintenance of optimal tissue healing; protection of peristomal
skin; learning how to ir-rigate the colostomy and change the appliance;
expressing feel-ings and concerns about the colostomy and the impact on himself
or herself; and avoidance of complications.
PREPARING THE PATIENT FOR SURGERY
The patient anticipating surgery for colorectal cancer has many concerns, needs, and fears. He or she may be physically debili-tated and emotionally distraught with concern about lifestyle changes after surgery, prognosis, ability to perform in established roles, and finances. Priorities for nursing care include preparing the patient physically for surgery, providing information about postoperative care, including stoma care if a colostomy is to be created, and supporting the patient and family emotionally.
Physical
preparation for surgery involves building the patientŌĆÖs stamina in the days
preceding surgery and cleansing and steriliz-ing the bowel the day before
surgery. If the patientŌĆÖs condition permits, the nurse recommends a diet high
in calories, protein, and carbohydrates and low in residue for several days
before surgery to provide adequate nutrition and minimize cramping by
decreasing excessive peristalsis. A full-liquid diet may be pre-scribed 24 to
48 hours before surgery to decrease bulk. If the pa-tient is hospitalized in
the days preceding surgery, PN may be required to replace depleted nutrients,
vitamins, and minerals. In some instances, PN may be given at home before
surgery. Anti-biotics such as sulfonamides, neomycin, and cephalexin are
ad-ministered the day before surgery to reduce intestinal bacteria. The bowel
is cleansed with laxatives, enemas, or colonic irriga-tions the evening before
and the morning of surgery.
For
the patient who is very ill and hospitalized, the nurse measures and records
intake and output, including vomitus, to provide an accurate record of fluid
balance. The patientŌĆÖs intake of oral food and fluids may be restricted to
prevent vomiting. The nurse administers antiemetics as prescribed. Full or
clear liquids may be tolerated, or the patient may be allowed nothing by mouth.
A nasogastric tube may be inserted to drain accumulated fluids and prevent
abdominal distention. The nurse monitors the ab-domen for increasing distention,
loss of bowel sounds, and pain or rigidity, which may indicate obstruction or
perforation. It also is important to monitor intravenous fluids and
electrolytes. Monitoring serum electrolyte levels can detect the hypokalemia
and hyponatremia that occur with GI fluid loss. The nurse observes for signs of
hypovolemia (eg, tachycardia, hypotension, decreased pulse volume), assesses
hydration status, and reports decreased skin turgor, dry mucous membranes, and
concentrated urine.
The nurse assesses the patientŌĆÖs knowledge about the diagno-sis, prognosis, surgical procedure, and expected level of func-tioning after surgery. It is important to include information about the physical preparation for surgery, the expected appear-ance and care of the wound, the technique of ostomy care (if ap-plicable), dietary restrictions, pain control, and medication management in the teaching plan (see Plan of Nursing Care 38-1). If the patient will be admitted the day of surgery, the physicianŌĆÖs office may arrange for the patient to be seen by an enterostomal therapist in the days preceding surgery.
The therapist
helps determine the optimal site for the stoma and provides teaching about
care. If the patient is hospitalized before the day of surgery, the staff
enterostomal therapist is involved in the pre-operative teaching. All
procedures are explained in language the patient understands.
PROVIDING EMOTIONAL SUPPORT
Patients
anticipating bowel surgery for colorectal cancer may be very anxious. They may
grieve about the diagnosis, the impend-ing surgery, and possible permanent
colostomy. Patients under-going surgery for a temporary colostomy may express
fears and concerns similar to those of a person with a permanent stoma. All
members of the health care team, including the enterostomal therapy nurse,
should be available for assistance and support. The nurseŌĆÖs role is to assess
the patientŌĆÖs anxiety level and coping mechanisms and suggest methods for
reducing anxiety such as deep-breathing exercises and visualizing a successful
recovery from surgery and cancer. Other supportive measures include pro-viding
privacy and teaching relaxation techniques to the patient. Time is set aside to
listen to the patient who wishes to talk, cry, or ask questions. The nurse can
arrange a meeting with a spiritual advisor if the patient desires or with the
physicians if the patient wishes to discuss the treatment or prognosis. To
promote patient comfort, the nurse projects a relaxed, professional, and
empa-thetic attitude. See Nursing Research Profile 38-1 about the importance of
spiritual well-being for patients with colorectal cancer.
The patient undergoing a colostomy may find the anticipated changes in body image and lifestyle profoundly disturbing. Be-cause the stoma is located on the abdomen, the patient may think that everyone will be aware of the ostomy. The nurse helps reduce this fear by presenting facts about the surgical procedure and the creation andmanagement of the ostomy. If the patient is recep-tive, the nurse can use diagrams, photographs, and appliances to explain and clarify. Because the patient is experiencing emotional stress, the nurse may need to repeat some of the information. The nurse provides time for the patient and family to ask questions; the nurseŌĆÖs acceptance and understanding of the patientŌĆÖs concerns and feelings convey a caring, competent attitude that promotes confidence and cooperation. Consultation with an enterostomal therapist during the preoperative period can be extremely helpful, as can speaking with a person who is successfully managing a colostomy. The United Ostomy Association provides useful in-formation about living with an ostomy through literature, lec-tures, and exhibits. Visiting services by qualified members and rehabilitation services for new ostomy patients are provided.
PROVIDING POSTOPERATIVE CARE
Postoperative
nursing care for patients undergoing colon resec-tion or colostomy is similar
to nursing care for any abdominal surgery patient, including pain management
dur-ing the immediate postoperative period. The nurse also monitors the patient
for complications such as leakage from the site of the anastomosis, prolapse of
the stoma, perforation, stoma retraction, fecal impaction, skin irritation, and
pulmonary complications as-sociated with abdominal surgery. The nurse assesses
the abdomen for returning peristalsis and assesses the initial stool
characteris-tics. It is important to help patients with a colostomy out of bed
on the first postoperative day and encourage them to begin par-ticipating in
managing the colostomy.
MAINTAINING OPTIMAL NUTRITION
The
nurse teaches all patients undergoing surgery for colorectal cancer about the
health benefits to be derived from consuming a healthy diet. The diet is
individualized as long as it is well bal-anced and does not cause diarrhea or
constipation. The return to normal diet is rapid.
A
complete nutritional assessment is important for patients with a colostomy. The
patient avoids foods that cause excessive odor and gas, including foods in the
cabbage family, eggs, fish, beans, and high-cellulose products such as peanuts.
It is important to determine whether the elimination of specific foods is
causing any nutritional deficiency. Nonirritating foods are substituted for
those that are restricted so that deficiencies are corrected. The nurse advises
the patient to experiment with an irritating food sev-eral times before
restricting it, because an initial sensitivity may de-crease with time. The
nurse can help the patient identify any foods or fluids that may be causing
diarrhea, such as fruits, high-fiber foods, soda, coffee, tea, or carbonated
beverages. Paregoric, bis-muth subgallate, bismuth subcarbonate, or
diphenoxylate with at-ropine (Lomotil) help control the diarrhea. For
constipation, prune or apple juice or a mild laxative is effective. The nurse
sug-gests fluid intake of at least 2 L of fluid per day.
PROVIDING WOUND CARE
The
nurse frequently examines the abdominal dressing during the first 24 hours
after surgery to detect signs of hemorrhage. It is im-portant to help the
patient splint the abdominal incision during coughing and deep breathing to
lessen tension on the edges of the incision. The nurse monitors temperature,
pulse, and respiratory rate for elevations, which may indicate an infectious
process. If the patient has a colostomy, the stoma is examined for swelling
(slight edema from surgical manipulation is normal), color (a healthy stoma is
pink or red), discharge (a small amount of ooz-ing is normal), and bleeding (an
abnormal sign).
If the
malignancy has been removed using the perineal route, the perineal wound is
observed for signs of hemorrhage. This wound may contain a drain or packing,
which is removed grad-ually. Bits of tissue may slough off for a week. This
process is hastened by mechanical irrigation of the wound or with sitz baths
performed two or three times each day initially. The condition of the perineal
wound and any bleeding, infection, or necrosis are documented.
MONITORING AND MANAGING COMPLICATIONS
The
patient is observed for signs and symptoms of complications. It is important to
frequently assess the abdomen, including de-creasing or changing bowel sounds
and increasing abdominal girth, to detect bowel obstruction. The nurse monitors
vital signs for increased temperature, pulse, and respirations and for
decreased blood pressure, which may indicate an intra-abdominal infectious
process. It is important to report rectal bleeding im-mediately because it
indicates hemorrhage. The nurse monitors hematocrit and hemoglobin levels and
administers blood com-ponent therapy as prescribed. Any abrupt change in
abdominal pain is reported promptly. Elevated white blood cell counts and
temperature or symptoms of shock are reported because they may indicate sepsis.
The nurse administers antibiotics as prescribed.
Pulmonary
complications are always a concern with abdomi-nal surgery; patients older than
50 years of age are at risk, espe-cially if they are or have been receiving sedatives
or are being maintained on bed rest for a prolonged period. Two primary
pul-monary complications are pneumonia and atelectasis. Frequent activity (eg,
turning the patient from side to side every 2 hours), deep breathing, coughing,
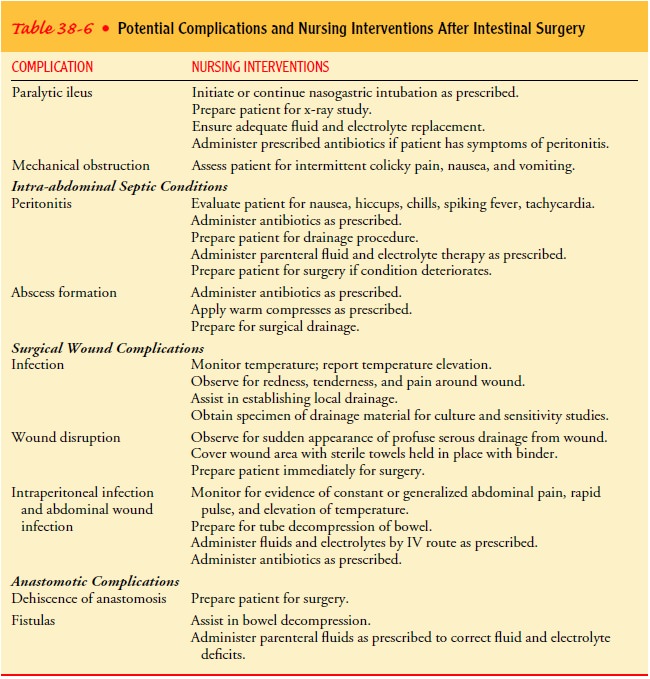
and early ambulation can reduce the risks for these complications. Table 38-6
lists possible postoper-ative complications.
The
incidence of complications related to the colostomy is about one half that seen
with an ileostomy. Some common com-plications are prolapse of the stoma
(usually from obesity), per-foration (from improper stoma irrigation), stoma
retraction, fecal impaction, and skin irritation. Leakage from an anastomotic
site can occur if the remaining bowel segments are diseased or weak-ened.
Leakage from an intestinal anastomosis causes abdominal distention and
rigidity, temperature elevation, and signs of shock. Surgical repair is
necessary.
REMOVING AND APPLYING THE COLOSTOMY APPLIANCE
The
colostomy begins to function 3 to 6 days after surgery. The nurse manages the
colostomy and teaches the patient about its care until the patient can take
over. The nurse teaches skin care and how to apply and remove the drainage
pouch. Care of the peristomal skin is an ongoing concern because excoriation or
ul-ceration can develop quickly. The presence of such irritation makes adhering
the ostomy appliance difficult, and adhering the ostomy appliance to irritated
skin can worsen the skin condition. The effluent discharge and the degree to
which it is irritating vary with the type of ostomy. With a transverse
colostomy, the stool is soft and mushy and irritating to the skin. With a
descending or sigmoid colostomy, the stool is fairly solid and less irritating
to the skin. Other skin problems include yeast infections and aller-gic
dermatitis.
If the
patient wants to bathe or shower before putting on the clean appliance,
micropore tape applied to the sides of the pouch will keep it secure during
bathing. To remove the appliance, the patient assumes a comfortable sitting or
standing position and gently pushes the skin down from the faceplate while
pulling the pouch up and away from the stoma. Gentle pressure prevents the skin
from being traumatized and any liquid fecal contents from spilling out. The
nurse advises the patient to protect the peri-stomal skin by then washing the
area gently with a moist, soft cloth and a mild soap. Soap acts as a mild
abrasive agent to re-move enzyme residue from fecal spillage. The patient
should re-move any excess skin barrier. While the skin is being cleansed, a
gauze dressing can cover the stoma, or a vaginal tampon can be inserted gently
to absorb excess drainage. After cleansing, the pa-tient pats the skin
completely dry with a gauze pad, taking care not to rub the area. The patient
can lightly dust nystatin (Myco-statin) powder on the peristomal skin if
irritation or yeast growth is present.
Smoothly applying the drainage appliance for a secure fit re-quires practice and a well-fitting appliance. Patients can choose from a wide variety of appliances, depending on their individual needs.
The stoma is measured to determine the correct size for the pouch; the pouch
opening should be about 0.3 cm (1Ōüä8 in) larger than the stoma. After the skin is
cleansed according to the previously described procedure, the patient applies
the peristomal skin barrier (ie, wafer, paste, or powder). Mild skin irritation
may require dusting the skin with karaya or Stomahesive powder be-fore
attaching the pouch. The patient removes the backing from the adherent surface
of the appliance, and places the bag down over the stoma for 30 seconds. The
patient empties or changes the drainage appliance when it is one-third to
one-fourth full so that the weight of its contents does not cause the appliance
to sep-arate from the adhesive disk and spill the contents. Most appli-ances
are disposable and odor resistant; commercially prepared deodorizers are
available.
For
some patients, colostomy appliances are not always nec-essary. As soon as the
patient has learned a routine for evacua-tion, bags may be dispensed with, and
a closed ostomy appliance or a simple dressing of disposable tissue (often
covered with plastic wrap) is used, held in place by an elastic belt. Except
for gas and a slight amount of mucus, nothing escapes from the colostomy
opening between irrigations. Colostomy plugs that expand on insertion to
prevent passage of flatus and feces are available.
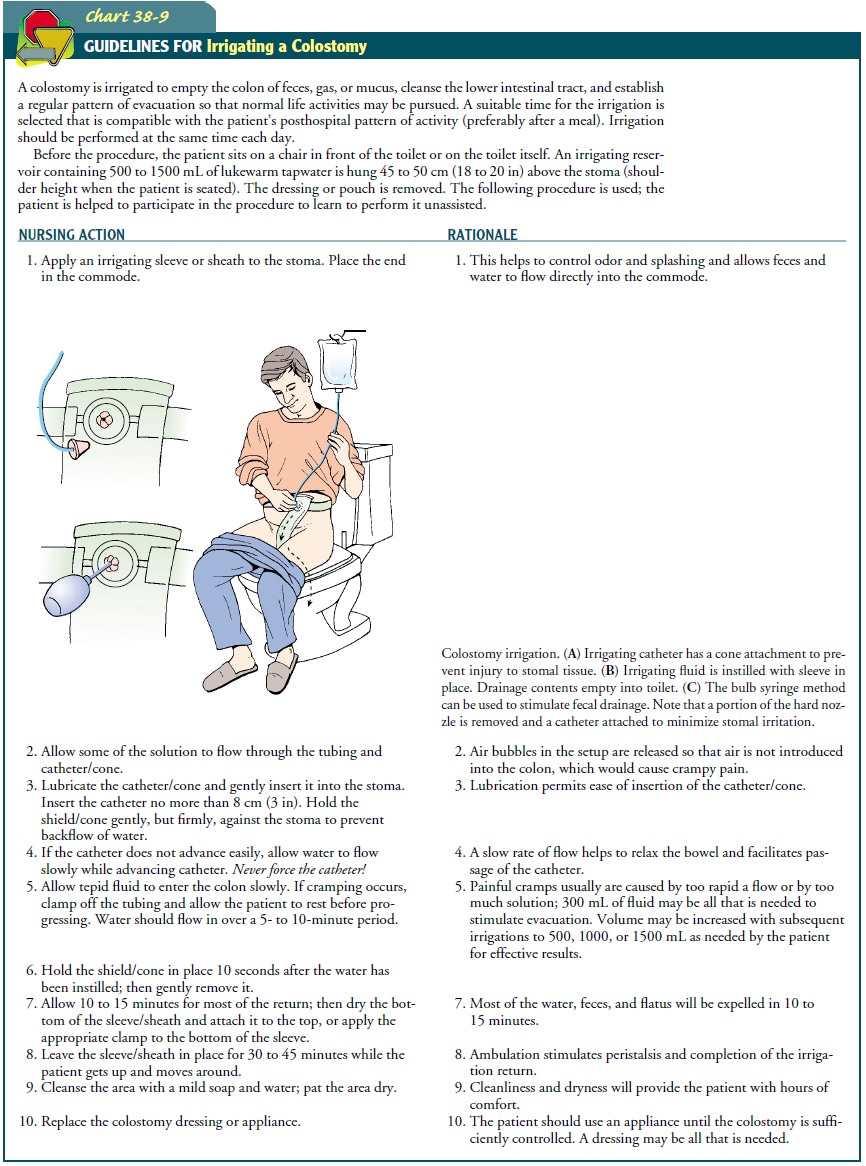
IRRIGATING THE COLOSTOM
The
purpose of irrigating a colostomy is to empty the colon of gas, mucus, and
feces so that the patient can go about social and busi-ness activities without
fear of fecal drainage. A stoma does not have voluntary muscular control and
may empty at irregular intervals. Regulating the passage of fecal material is
achieved by irrigating the colostomy or allowing the bowel to evacuate
naturally with-out irrigations. The choice often depends on the individual and
the type of the colostomy. By irrigating the stoma at a regular time, there is
less gas and retention of the irrigant. The time for ir-rigating the colostomy
should be consistent with the schedule the person will follow after leaving the
hospital. Chart 38-9 delineates the irrigating procedure.
SUPPORTING A POSITIVE BODY IMAGE
The patient is encouraged to verbalize feelings and concerns about altered body image and to discuss the surgery and the stoma (if one was created). A supportive environment and a supportive attitude on the nurseŌĆÖs part are crucial in promoting the patientŌĆÖs adaptation to the changes brought about by the surgery. If applicable, the patient must learn colostomy care and begin to plan for incorporating stoma care into daily life. The nurse helps the patient overcome aversion to the stoma or fear of self-injury by providing care and teaching in an open, ac-cepting manner and by encouraging the patient to talk about his or her feelings about the stoma.
DISCUSSING SEXUALITY ISSUES
The
nurse encourages the patient to discuss feelings about sexu-ality and sexual
function. Some patients may initiate questions about sexual activity directly
or give indirect clues about their fears. Some may view the surgery as
mutilating and a threat to their sexuality; some fear impotence. Others may
express worry about odor or leakage from the pouch during sexual activity.
Al-though the appliance presents no deterrent to sexual activity, some patients
wear silk or cotton covers and smaller pouches during sex. Alternative sexual
positions are recommended, as well as alternative methods of stimulation to
satisfy sexual drives. The nurse assesses the patientŌĆÖs needs and attempts to
identify specific concerns. If the nurse is uncomfortable with this or if the
patientŌĆÖs concerns seem complex, it is appropriate for the nurse to seek assistance
from an enterostomal therapy nurse, sex coun-selor or therapist, or advanced
practice nurse.
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care
Patient
education and discharge planning require the combined efforts of the physician,
nurse, enterostomal therapist, social worker, and dietitian. Patients are given
specific information, in-dividualized to their needs, about ostomy care and
signs and symptoms of potential complications. Dietary instructions are
es-sential to help patients identify and eliminate irritating foods that can
cause diarrhea or constipation. It is important to teach pa-tients about their
prescribed medications (ie, action, purpose, and possible side effects).
The
nurse reviews treatments (eg, irrigations, wound cleans-ing) and dressing
changes and encourages the family to partici-pate. Because the hospital stay is
short, the patient may not be able to become proficient in stoma care
techniques before dis-charge. Many patients need referral to a home care agency
and the telephone number of the local c hapter of the American Can-cer Society.
The home care nurse goes to the home to provide fur-ther care and teaching and
to assess how well the patient and family are adjusting to the colostomy. The
home environment is assessed for adequacy of resources that allow the patient
to ac-complish self-care. A family member may assume responsibility for
purchasing the equipment and supplies needed at home.
Patients
need very specific directions about when to call the physician. They need to
know which complications require prompt attention (ie, bleeding, abdominal
distention and rigidity, diarrhea, fever, wound drainage, and disruption of
suture line). If radiation therapy is planned, the possible side effects (ie,
anorexia, vomiting, diarrhea, and exhaustion) are reviewed.
Continuing Care
Ongoing
care of the patient with cancer and a colostomy often ex-tends well beyond the
initial hospital stay. Home care nurses man-age ostomy follow-up care, manage
the assessment and care of the debilitated patient, and coordinate adjuvant
therapy. The home care visits also provide the nurse with opportunities to
assess the patientŌĆÖs physical and emotional status and the patientŌĆÖs and
fam-ilyŌĆÖs ability to carry out recommended management strategies. Visits from
an enterostomal therapy nurse are available to the pa-tient and family as they
learn to care for the ostomy and work through their feelings about it, the
diagnosis of cancer, and the future. Some patients are interested in and can
benefit from involvement in an ostomy support group.
Evaluation
EXPECTED PATIENT OUTCOMES
Expected
patient outcomes may include the following:
ŌĆó
Consumes a healthy diet
a)
Avoids foods and fluids that cause diarrhea
b)
Substitutes nonirritating foods and fluids for those
that are restricted
ŌĆó
Maintains fluid balance
a)
Experiences no vomiting or diarrhea
b)
Experiences no signs or symptoms of dehydration
ŌĆó
Feels less anxious
a)
Expresses concerns and fears freely
b)
Uses coping measures to manage stress
ŌĆó
Acquires information about diagnosis, surgical
procedure, preoperative preparation, and self-care after discharge
a) Discusses the diagnosis,
surgical procedure, and post-operative self-care
b)
Demonstrates techniques of ostomy care
ŌĆó
Maintains clean incision, stoma, and perineal wound
ŌĆó
Expresses feelings and concerns about self
a)
Gradually increases participation in stoma and
peri-stomal skin care
b)
Discusses feelings related to changed appearance
ŌĆó
Discusses sexuality in relation to ostomy and to
changes in body image
ŌĆó
Recovers without complications
a)
Is afebrile
b)
Regains normal bowel activity
c) Exhibits no signs and
symptoms of perforation or bleeding
Related Topics