Chapter: Medical Surgical Nursing: Management of Patients With Intestinal and Rectal Disorders
Diseases of the Anorectum
Diseases of the Anorectum
Anorectal
disorders are common, and more than one half of the population will experience
one at some time during their lives (Yamada et al., 1999). Patients with
anorectal disorders seek medical care primarily because of pain, rectal
bleeding, or change in bowel habits. Other common complaints are protrusion of
hemorrhoids, anal discharge, perianal itching, swelling, anal ten-derness,
stenosis, and ulceration. Constipation results from delay-ing defecation
because of anorectal pain.
There
has been a steady increase in the frequency of sexually transmitted diseases in
recent decades, leading to the identifica-tion of new anorectal syndromes. The
prevalence of these condi-tions is increasing. These syndromes include venereal
infections such as syphilis, gonorrhea, herpes, chlamydia, and candidiasis, and
they are most commonly seen in male homosexuals who practice anorectal
intercourse (Wolfe, 2000).
ANORECTAL ABSCESS
An
anorectal abscess is caused by obstruction of an anal gland, resulting in
retrograde infection. People with regional enteritis or immunosuppressive
conditions such as AIDS are particularly susceptible to these infections. Many
of these abscesses result in fistulas.
An
abscess may occur in a variety of spaces in and around the rectum. It often
contains a quantity of foul-smelling pus and is painful. If the abscess is
superficial, swelling, redness, and ten-derness are observed. A deeper abscess
may result in toxic symp-toms, lower abdominal pain, and fever.
Palliative
therapy consists of sitz baths and analgesics. How-ever, prompt surgical
treatment to incise and drain the abscess is the treatment of choice. When a
deeper infection exists with the possibility of a fistula, the fistulous tract
must be excised. If pos-sible, the fistula is excised when the abscess is
incised and drained, or a second procedure to do so may be necessary. The wound
may be packed with gauze and allowed to heal by granulation.
ANAL FISTULA
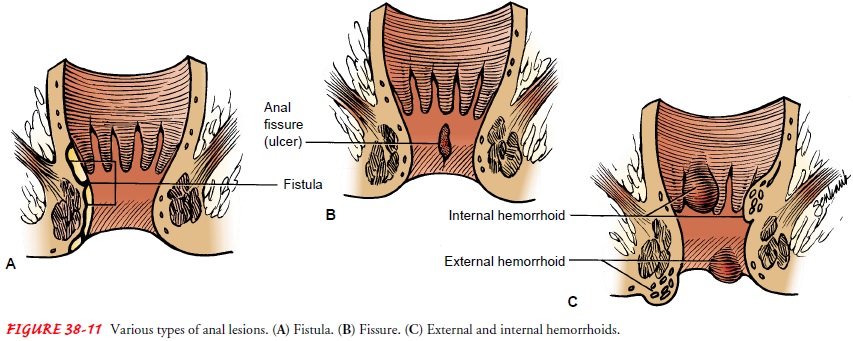
An
anal fistula is a tiny, tubular, fibrous tract that extends into the anal canal
from an opening located beside the anus (Fig. 38-11A). Fistulas usually result
from an infection. They may also develop from trauma, fissures, or regional
enteritis. Pus or stool may leak constantly from the cutaneous opening. Other
symptoms may be the passage of flatus or feces from the vagina or bladder,
depend-ing on the fistula tract. Untreated fistulas may cause systemic
in-fection with related symptoms.
Surgery
is always recommended, because few fistulas heal spon-taneously. A fistulectomy
(ie, excision of the fistulous tract) is the recommended surgical procedure.
The lower bowel is evacuated thoroughly with several prescribed enemas. During
surgery, the sinus tract is identified by inserting a probe into it or by
injecting the tract with methylene blue solution. The fistula is dissected out
or laid open by an incision from its rectal opening to its outlet. The wound is
packed with gauze.
ANAL FISSURE
An anal fissure is a longitudinal tear or
ulceration in the lining of the anal canal (see Fig. 38-11B). Fissures are
usually caused by the trauma of passing a large, firm stool or from persistent
tightening of the anal canal because of stress and anxiety (leading to
constipation). Other causes include childbirth, trauma, and overuse of
laxatives.
Extremely painful defecation, burning, and
bleeding character-ize fissures. Most of these fissures heal if treated by
conservative mea-sures, which include stool softeners and bulk agents, an
increase in water intake, sitz baths, and emollient suppositories. A
suppository combining an anesthetic with a corticosteroid helps relieve the
dis-comfort. Anal dilation under anesthesia may be required.
If
fissures do not respond to conservative treatment, surgery is indicated. The
procedure considered by most surgeons to be the procedure of choice is the
lateral internal sphincterotomy with excision of the fissure; the success rate
is 90% to 95% (Rieghley, 1999).
HEMORRHOIDS
Hemorrhoids are dilated portions of veins in the anal canal. They are very common. By the age of 50, about 50% of people have hemorrhoids to some extent (Corman, 1998).
Shearing of the mucosa
during defecation results in the sliding of the structures in the wall of the
anal canal, including the hemorrhoidal and vascular tissues. Increased pressure
in the hemorrhoidal tissue due to pregnancy may initiate hemorrhoids or
aggravate existing ones. Hemorrhoids are classified as one of two types. Those
above the internal sphincter are called internal hemorrhoids, and those
appearing outside the external sphincter are called external hem-orrhoids (see
Fig. 38-11C).
Hemorrhoids
cause itching and pain and are the most common cause of bright red bleeding
with defecation. External hemor-rhoids are associated with severe pain from the
inflammation and edema caused by thrombosis (ie, clotting of blood within the
hem-orrhoid). This may lead to ischemia of the area and eventual necrosis.
Internal hemorrhoids are not usually painful until they bleed or prolapse when
they become enlarged.
Hemorrhoid
symptoms and discomfort can be relieved by good personal hygiene and by avoiding
excessive straining during defecation. A high-residue diet that contains fruit
and bran along with an increased fluid intake may be all the treatment that is
necessary to promote the passage of soft, bulky stools to prevent straining. If
this treatment is not successful, the addition of hy-drophilic bulk-forming
agents such as psyllium and mucilloid may help. Warm compresses, sitz baths,
analgesic ointments and suppositories, astringents (eg, witch hazel), and bed
rest allow the engorgement to subside.
There
are several types of nonsurgical treatments for hemor-rhoids. Infrared
photocoagulation, bipolar diathermy, and laser therapy are newer techniques
that are used to affix the mucosa to the underlying muscle. Injecting
sclerosing solutions is also ef-fective for small, bleeding hemorrhoids. These
procedures help prevent prolapse.
A
conservative surgical treatment of internal hemorrhoids is the rubber-band
ligation procedure. The hemorrhoid is visual-ized through the anoscope, and its
proximal portion above the mucocutaneous lines is grasped with an instrument. A
small rub-ber band is then slipped over the hemorrhoid. Tissue distal to the
rubber band becomes necrotic after several days and sloughs off. Fibrosis
occurs; the result is that the lower anal mucosa is drawn up and adheres to the
underlying muscle. Although this treat-ment has been satisfactory for some
patients, it has proven painful for others and may cause secondary hemorrhage.
It has been known to cause perianal infection.
Cryosurgical
hemorrhoidectomy, another method for re-moving hemorrhoids, involves freezing
the hemorrhoid for a sufficient time to cause necrosis. Although it is
relatively pain-less, this procedure is not widely used because the discharge
is very foul smelling and wound healing is prolonged. The Nd:YAG laser is
useful in excising hemorrhoids, particularly external hemorrhoidal tags. The
treatment is quick and rela-tively painless. Hemorrhage and abscess are rare
postoperative complications.
The
previously described methods of treating hemorrhoids are not effective for
advanced thrombosed veins, which must be treated by more extensive surgery.
Hemorrhoidectomy, or surgi-cal excision, can be performed to remove all the
redundant tissue involved in the process. During surgery, the rectal sphincter
is usually dilated digitally and the hemorrhoids are removed with a clamp and
cautery or are ligated and then excised. After the op-erative procedures are
completed, a small tube may be inserted through the sphincter to permit the escape
of flatus and blood; pieces of Gelfoam or Oxycel gauze may be placed over the
anal wounds.
SEXUALLY TRANSMITTED ANORECTAL DISEASES
Three infectious syndromes that are related
to sexually transmitted diseases have been identified. Proctitis involves the
rectum. It is commonly associated with recent anal-receptive intercourse with
an infected partner. Symptoms include a mucopurulent discharge or bleeding,
pain in the area, and diarrhea. The pathogens most fre-quently involved are Neisseria gonorrheae (53%), Chlamydia (20%), herpes simplex virus
(18%), and Treponema pallidium (9%)
(Yamada et al., 1999). Proctocolitis involves the rectum and lowest portion of
the descending colon. Symptoms are similar to proctitis but may also include
watery or bloody diarrhea, cramps, pain, and bloating. Enteritis involves more
of the descending colon, and symp-toms include watery, bloody diarrhea;
abdominal pain; and weight loss. The most common pathogens causing enteritis
are E. histolyt-ica, Giardia lamblia,
Shigella, and Campylobacter (Wolfe,
2000).
Sigmoidoscopy
is performed to identify portions of the anorec-tum involved. Samples are taken
with rectal swabs, and cultures are obtained to identify the pathogens
involved. The treatment of choice for bacterial infections is antibiotics (ie,
cefixime, doxycy-cline, and penicillin). Acyclovir is given to those with viral
infec-tions. Infections from E.
histolytica and G. lamblia are
treated with antiamebic therapy (ie, metronidazole). Ciprofloxacin is an
effec-tive treatment for Shigella.
Antibiotics of choice for Campylobacter
infection are erythromycin and ciprofloxacin.
PILONIDAL SINUS OR CYST
A pilonidal sinus or cyst is found in the intergluteal cleft on the posterior surface of the lower sacrum (Fig. 38-12). Current the-ories suggest that it results from local trauma that causes the penetration of hairs into the epithelium and subcutaneous tissue (Yamada et al., 1999).
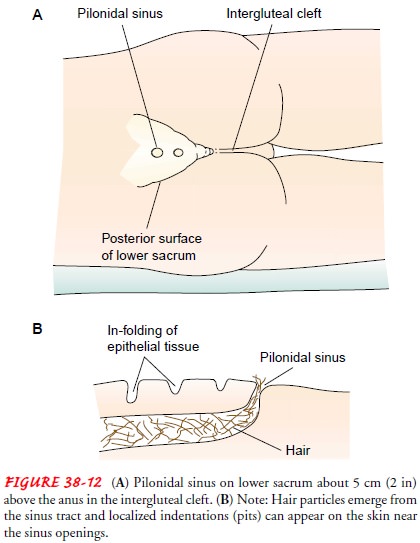
It
may also be formed congenitally by an infolding of epithelial tissue beneath
the skin, which may com-municate with the skin surface through one or several
small sinus openings. Hair frequently is seen protruding from these open-ings,
and this gives the cyst its name, pilonidal
(ie, a nest of hair). The cysts rarely cause symptoms until adolescence or
early adult life, when infection produces an irritating drainage or an abscess.
Perspiration and friction easily irritate this area.
In the
early stages of the inflammation, the infection may be controlled by antibiotic
therapy, but after an abscess has formed, surgery is indicated. The abscess is
incised and drained under local anesthesia. After the acute process resolves,
further surgery is performed to excise the cyst and the secondary sinus tracts.
The wound is allowed to heal by granulation. Gauze dressings are placed in the
wound to keep its edges separated while heal-ing occurs.
Related Topics