Chapter: Medical Surgical Nursing: Management of Patients With Intestinal and Rectal Disorders
Colorectal Cancer
COLORECTAL
CANCER
Tumors
of the colon and rectum are relatively common; the col-orectal area (the colon
and rectum combined) is now the third most common site of new cancer cases and
deaths in the United States. Colorectal cancer is a disease of Western
cultures; there were an estimated 148,300 new cases and 56,000 deaths from the
disease in 2002 (American Cancer Society, 2002).
The
incidence increases with age (the incidence is highest for people older than 85
years of age) and is higher for people with a family history of colon cancer
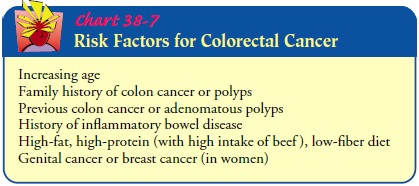
and those with IBD or polyps. The exact cause of colon and rectal cancer is
still unknown, but risk factors have been identified (Chart 38-7).
The
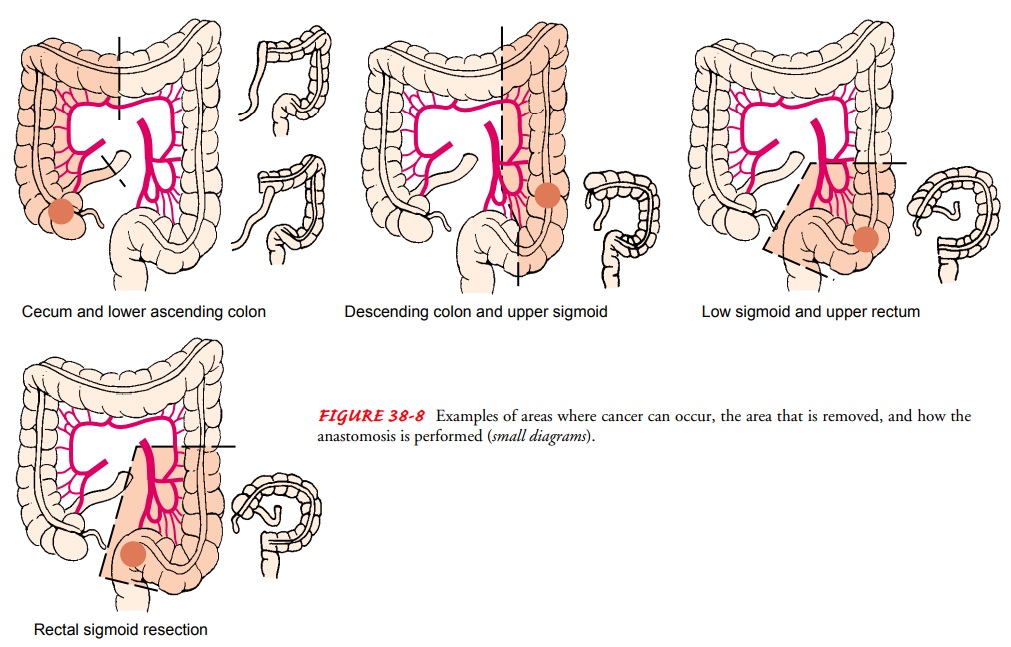
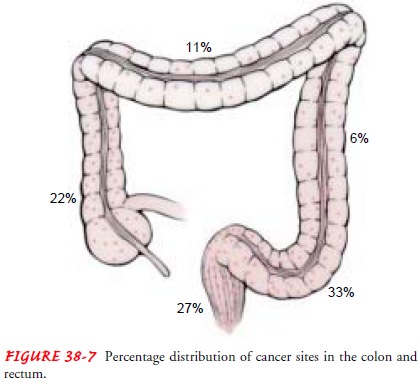
distribution of cancer sites throughout the colon is shown in Figure 38-7
(Goldman, & Bennett, 2000). Changes in this dis-tribution have occurred in
recent years. The incidence of cancer in the sigmoid and rectal areas has
decreased, whereas the inci-dence of cancer in the cecum, ascending, and
descending colon has increased.
Improved
screening strategies have helped to reduce the num-ber of deaths in recent
years. Of the more than 148,000 people diagnosed each year, fewer than half
that number die annually (Beyers et al., 2001). Early diagnosis and prompt treatment
could save almost three of every four people with colorectal cancer. If the
disease is detected and treated at an early stage, the 5-year sur-vival rate is
90%, but only 34% of colorectal cancers are found at an early stage. Survival
rates after late diagnosis are very low. Most people are asymptomatic for long
periods and seek health care only when they notice a change in bowel habits or
rectal bleed-ing. Prevention and early screening are key to detection and
re-duction of mortality rates.
Pathophysiology
Cancer
of the colon and rectum is predominantly (95%) ade-nocarcinoma (ie, arising
from the epithelial lining of the intes-tine). It may start as a benign polyp
but may become malignant, invade and destroy normal tissues, and extend into
surrounding structures. Cancer cells may break away from the primarytumor and
spread to other parts of the body (most often to the liver).
Clinical Manifestations
The
symptoms are greatly determined by the location of the cancer, the stage of the
disease, and the function of the intesti-nal segment in which it is located.
The most common present-ing symptom is a change in bowel habits. The passage of
blood in the stools is the second most common symptom. Symptoms may also
include unexplained anemia, anorexia, weight loss, and fatigue.
The
symptoms most commonly associated with right-sided le-sions are dull abdominal
pain and melena (ie, black, tarry stools). The symptoms most commonly
associated with left-sided lesions are those associated with obstruction (ie, abdominal
pain and cramping, narrowing stools, constipation, and distention), as well as
bright red blood in the stool. Symptoms associated with rectal lesions are
tenesmus (ie, ineffective, painful straining at stool), rec-tal pain, the
feeling of incomplete evacuation after a bowel move-ment, alternating
constipation and diarrhea, and bloody stool.
Assessment and Diagnostic Findings
Along
with an abdominal and rectal examination, the most im-portant diagnostic
procedures for cancer of the colon are fecal oc-cult blood testing, barium
enema, proctosigmoidoscopy, and colonoscopy. As many as 60% of colorectal
cancer cases can be identified by sigmoidoscopy with biopsy or cytology smears
(Yamada et al., 1999).
Carcinoembryonic
antigen (CEA) studies may also be per-formed. Although CEA may not be a highly
reliable indicator in diagnosing colon cancer because not all lesions secrete
CEA, stud-ies show that CEA levels are reliable in predicting prognosis. With
complete excision of the tumor, the elevated levels of CEA should return to
normal within 48 hours. Elevations of CEA at a later date suggest recurrence
(Yamada et al., 1999).
Complications
Tumor
growth may cause partial or complete bowel obstruction. Extension of the tumor
and ulceration into the surrounding blood vessels results in hemorrhage.
Perforation, abscess formation, peri-tonitis, sepsis, and shock may occur.
Gerontologic Considerations
The
incidence of carcinoma of the colon and rectum increases with age. These
cancers are considered common malignancies in advanced age. Only prostate
cancer and lung cancer in men exceed colorectal cancer. Among women, only
breast cancer exceeds the incidence of colorectal cancer (Lueckenotte, 2000).
Symptoms are often insidious. Cancer patients usually report fatigue, which is
caused primarily by iron-deficiency anemia. In early stages, minor changes in
bowel patterns and occasional bleeding may occur. The later symptoms most
commonly reported by the elderly are abdominal pain, obstruction, tenesmus, and
rectal bleeding.
Colon
cancer in the elderly has been closely associated with di-etary carcinogens.
Lack of fiber is a major causative factor because the passage of feces through
the intestinal tract is prolonged, which extends exposure to possible
carcinogens. Excess fat is be-lieved to alter bacterial flora and convert
steroids into compounds that have carcinogenic properties.
Medical Management
The
patient with symptoms of intestinal obstruction is treated with intravenous
fluids and nasogastric suction. If there has been significant bleeding, blood
component therapy may be required.
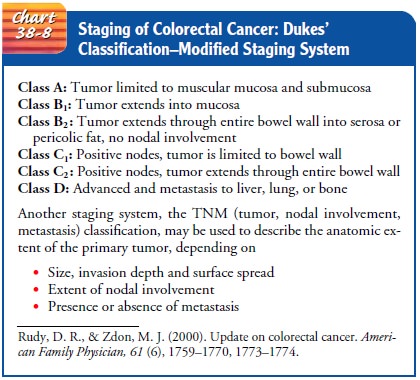
Treatment
for colorectal cancer depends on the stage of the disease (Chart 38-8) and
consists of surgery to remove the tumor, supportive therapy, and adjuvant
therapy. Data demonstrate de-lays in tumor recurrence and increases in survival
time for patients who receive some form of adjuvant therapy—chemotherapy,
radiation therapy, immunotherapy, or multimodality therapy.
ADJUVANT THERAPY
The
standard adjuvant therapy administered to patients with Dukes’ class C colon
cancer is the 5-fluorouracil plus levamisole regimen (Wolfe, 2000). Patients
with Dukes’ class B or C rectal cancer are given 5-fluorouracil and high doses
of pelvic irradia-tion. Mitomycin is also used. Radiation therapy is used
before, during, and after surgery to shrink the tumor, to achieve better
results from surgery, and to reduce the risk of recurrence. For in-operative or
unresectable tumors, irradiation is used to provide significant relief from
symptoms. Intracavity and implantable devices are used to deliver radiation to
the site. The response to adjuvant therapy varies.
SURGICAL MANAGEMENT
Surgery is the primary treatment for most colon and rectal can-cers. It may be curative or palliative. Advances in surgical tech-niques can enable the patient with cancer to have sphincter-saving devices that restore continuity of the GI tract (Tierney et al., 2000). The type of surgery recommended depends on the location and size of the tumor. Cancers limited to one site can be removed through the colonoscope. Laparoscopic colotomy with polypec-tomy minimizes the extent of surgery needed in some cases. A lap-aroscope is used as a guide in making an incision into the colon; the tumor mass is then excised. Use of the neodymium/yttrium-aluminum-garnet (Nd:YAG) laser has proved effective with some lesions as well. Bowel resection is indicated for most class A lesions and all class B and C lesions. Surgery is sometimes recommended for class D colon cancer, but the goal of surgery in this instance is palliative; if the tumor has spread and involves surrounding vital structures, it is considered nonresectable.
Surgical
procedures include the following:
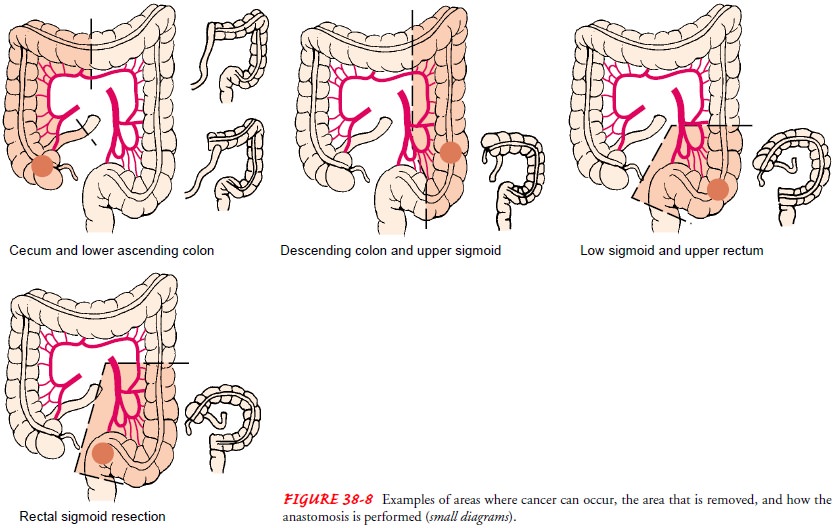
•
Segmental resection with anastomosis (ie, removal
of the tumor and portions of the bowel on either side of the growth, as well as
the blood vessels and lymphatic nodes) (Fig. 38-8).
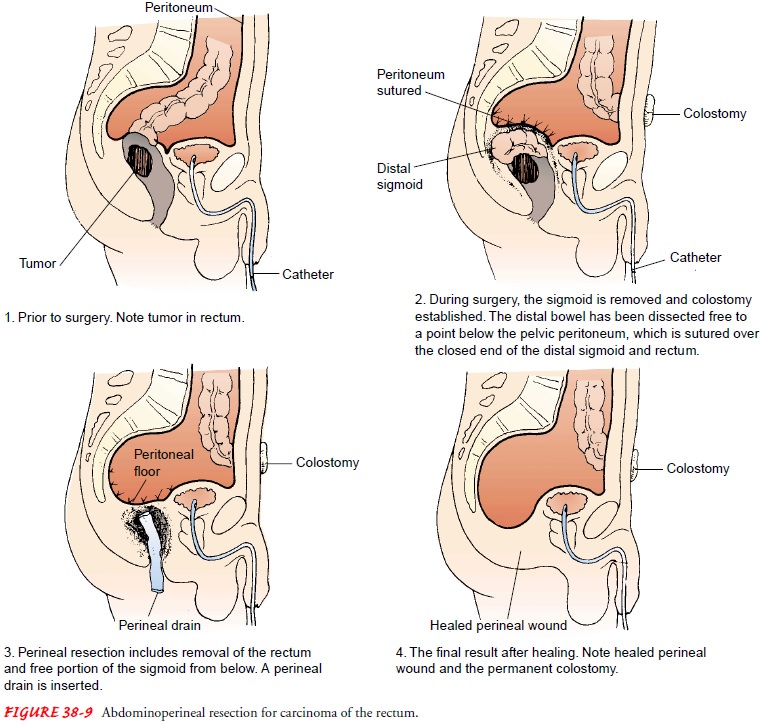
•
Abdominoperineal resection with permanent sigmoid
colos-tomy (ie, removal of the tumor and a portion of the sigmoid and all of
the rectum and anal sphincter) (Fig. 38-9).
•
Temporary colostomy followed by segmental resection
and anastomosis and subsequent reanastomosis of the colostomy, allowing initial
bowel decompression and bowel preparation before resection
•
Permanent colostomy or ileostomy for palliation of
unre-sectable obstructing lesions
•
Construction of a coloanal reservoir called a
colonic J pouch is performed in two steps. A temporary loop ileostomy is
constructed to divert intestinal flow, and the newly con-structed J pouch (made
from 6 to 10 cm of colon) is re-attached to the anal stump. About 3 months
after the initial stage, the ileostomy is reversed, and intestinal continuity
is restored. The anal sphincter and therefore continence are preserved.
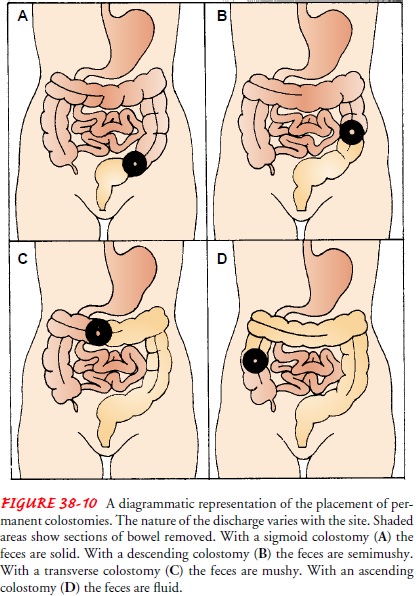
A colostomy is the surgical creation of
an opening (ie, stoma) into the colon. It can be created as a temporary or
permanent fecal diversion. It allows the drainage or evacuation of colon
con-tents to the outside of the body. The consistency of the drainage is
related to the placement of the colostomy, which is dictated by the location of
the tumor and the extent of invasion into sur-rounding tissues (Fig. 38-10).
With improved surgical tech-niques, colostomies are performed on fewer than one
third of patients with colorectal cancer.
Gerontologic Considerations
The
elderly are at increased risk for complications after surgery and may have
difficulty managing colostomy care. They may have decreased vision, impaired
hearing, and difficulty with fine motor coordination. It may be helpful for the
patient to handle ostomy equipment and simulate cleaning the peristomal skin
and irri-gating the stoma before surgery. Skin care is a major concern in the
elderly ostomate because of the skin changes that occur with aging—the epithelial
and subcutaneous fatty layers become thin, and the skin is irritated easily. To
prevent skin breakdown, special attention is paid to skin cleansing and the
proper fit of an appliance. Arteriosclerosis causes decreased blood flow to the
wound and stoma site. As a result, transport of nutrients is de-layed, and
healing time may be prolonged. Some patients have delayed elimination after
irrigation because of decreased peristalsis and mucus production. Most patients
require 6 months before they feel comfortable with their ostomy care.
Related Topics