Chapter: Medical Surgical Nursing: Management of Patients With Intestinal and Rectal Disorders
Irritable Bowel Syndrome - Abnormalities of Fecal Elimination
IRRITABLE
BOWEL SYNDROME
IBS is
one of the most common GI problems. Approximately one in six otherwise healthy
persons report classic symptoms of IBS (Wolfe, 2000). It occurs more commonly
in women than in men, and the cause is still unknown. Although no anatomic or
bio-chemical abnormalities have been found that explain the com-mon symptoms,
various factors are associated with the syndrome: heredity, psychological
stress or conditions such as depression and anxiety, a diet high in fat and
stimulating or irritating foods, alcohol consumption, and smoking. The small
intestine has be-come a focus of investigation as an additional site of
dysmotility in IBS, and cluster contractions in the jejunum and ileum are being
studied (Wolfe, 2000). The diagnosis is made only after tests have been
completed that prove the absence of structural or other disorders.
Pathophysiology
IBS
results from a functional disorder of intestinal motility. The change in
motility may be related to the neurologic regulatory system, infection or
irritation, or a vascular or metabolic distur-bance. The peristaltic waves are
affected at specific segments of the intestine and in the intensity with which
they propel the fecal matter forward. There is no evidence of inflammation or
tissue changes in the intestinal mucosa.
Clinical Manifestations
There
is a wide variability in symptom presentation. Symptoms range in intensity and
duration from mild and infrequent to se-vere and continuous. The primary
symptom is an alteration in bowel patterns—constipation, diarrhea, or a
combination of both. Pain, bloating, and abdominal distention often accompany
this change in bowel pattern. The abdominal pain is sometimes precipitated by
eating and is frequently relieved by defecation.
Assessment and Diagnostic Findings
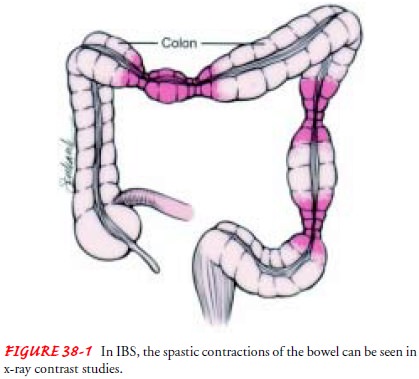
A
definite diagnosis of IBS requires tests that prove the absence of structural
or other disorders. Stool studies, contrast x-ray stud-ies, and proctoscopy may
be performed to rule out other colon diseases. Barium enema and colonoscopy may
reveal spasm, dis-tention, or mucus accumulation in the intestine (Fig. 38-1).
Manometry and electromyography are used to study intralumi-nal pressure changes
generated by spasticity.
Medical Management
The goals of treatment are aimed at relieving abdominal pain, con-trolling the diarrhea or constipation, and reducing stress. Re-striction and then gradual reintroduction of foods that are possibly irritating may help determine what types of food are acting as ir-ritants (eg, beans, caffeinated products, fried foods, alcohol, spicy foods). A healthy, high-fiber diet is prescribed to help control the diarrhea and constipation. Exercise can assist in reducing anxiety and increasing intestinal motility. Patients often find it helpful to participate in a stress reduction or behavior-modification program.
Hydrophilic
colloids (ie, bulk) and antidiarrheal agents (eg, lop-eramide) may be given to
control the diarrhea and fecal urgency. Antidepressants can assist in treating
underlying anxiety and de-pression. Anticholinergics and calcium channel
blockers decrease smooth muscle spasm, decreasing cramping and constipation.
Nursing Management
The
nurse’s role is to provide patient and family education. The nurse emphasizes
teaching and reinforces good dietary habits. The patient is encouraged to eat
at regular times and to chew food slowly and thoroughly. The patient should
understand that, al-though adequate fluid intake is necessary, fluid should not
be taken with meals because this results in abdominal distention. Alcohol use
and cigarette smoking are discouraged.
Related Topics