Chapter: Medical Surgical Nursing: Management of Patients With Intestinal and Rectal Disorders
Nursing Process: Management of the Patient With Inflammatory Bowel Disease
NURSING
PROCESS:MANAGEMENT OF THE PATIENT WITH INFLAMMATORY BOWEL DISEASE
Assessment
The
nurse takes a health history to identify the onset, duration, and
characteristics of abdominal pain; the presence of diarrhea or fecal urgency,
straining at stool (tenesmus), nausea, anorexia, or weight loss; and family
history of IBD. It is important to discuss dietary patterns, including the
amounts of alcohol, caffeine, and nicotine containing products used daily and
weekly. The nurse asks about patterns of bowel elimination, including
character, fre-quency, and presence of blood, pus, fat, or mucus. It is
important to note allergies and food intolerance, especially milk (lactose)
in-tolerance. The patient may identify sleep disturbances if diarrhea or pain
occurs at night.
Assessment
includes auscultating the abdomen for bowel sounds and their characteristics;
palpating the abdomen for distention, tenderness, or pain; and inspecting the
skin for evidence of fistula tracts or symptoms of dehydration. The stool is
inspected for blood and mucus.
With
regional enteritis, pain is usually localized in the right lower quadrant,
where hyperactive bowel sounds can be heard be-cause of borborygmus and
increased peristalsis. Abdominal ten-derness is noticed on palpation. The most
prominent symptom is intermittent pain that occurs with diarrhea but does not
de-crease after defecation. Pain in the periumbilical region usually indicates
involvement of the terminal ileum. With ulcerative colitis, the abdomen may be
distended, and rebound tenderness may be present. Rectal bleeding is a
significant sign.
Diagnosis
NURSING DIAGNOSES
Based
on the assessment data, the nursing diagnoses may include the following:
•
Diarrhea related to the inflammatory process
•
Acute pain related to increased peristalsis and GI
inflam-mation
•
Deficient fluid volume deficit related to anorexia,
nausea, and diarrhea
•
Imbalanced nutrition, less than body requirements,
related to dietary restrictions, nausea, and malabsorption
•
Activity intolerance related to fatigue
•
Anxiety related to impending surgery
•
Ineffective coping related to repeated episodes of
diarrhea
•
Risk for impaired skin integrity related to
malnutrition and diarrhea
•
Risk for ineffective therapeutic regimen management
related to insufficient knowledge concerning the process and man-agement of the
disease
COLLABORATIVE PROBLEMS/ POTENTIAL COMPLICATIONS
Potential
complications that may develop include the following:
•
Electrolyte imbalance
•
Cardiac dysrhythmia related to electrolyte
depletion
•
GI bleeding with fluid volume loss
•
Perforation of the bowel
Planning and Goals
The
major goals for the patient include attainment of normal bowel elimination
patterns, relief of abdominal pain and cramp-ing, prevention of fluid volume
deficit, maintenance of optimal nutrition and weight, avoidance of fatigue,
reducing anxiety, pro-moting effective coping, absence of skin breakdown,
learning about the disease process and therapeutic regimen, and avoidance of
complications.
Nursing Interventions
MAINTAINING NORMAL ELIMINATION PATTERNS
The
nurse determines if there is a relationship between diarrhea and certain foods,
activity, or emotional stress. Identifying pre-cipitating factors, the
frequency of bowel movements, and the character, consistency, and amount of
stool passed is important. The nurse provides ready access to a bathroom,
commode, or bedpan and keeps the environment clean and odor free. It is
im-portant to administer antidiarrheal medications as prescribed, to record the
frequency and consistency of stools after therapy is ini-tiated, and to
encourage bed rest to decrease peristalsis.
RELIEVING PAIN
The
character of the pain is described as dull, burning, or crampy. Asking about
its onset is relevant. Does it occur before or after meals, during the night,
or before elimination? Is the pattern con-stant or intermittent? Is it relieved
with medications? The nurse administers anticholinergic medications as
prescribed 30 minutes before a meal to decrease intestinal motility and
administers anal-gesics as prescribed for pain. Position changes, local
application of heat (as prescribed), diversional activities, and the prevention
of fatigue also are helpful for reducing pain.
MAINTAINING FLUID INTAKE
To
detect fluid volume deficit, the nurse keeps an accurate record of oral and
intravenous fluids and maintains a record of output (ie, urine, liquid stool,
vomitus, and wound or fistula drainage). The nurse monitors daily weights for
fluid gains or losses and as-sesses the patient for signs of fluid volume
deficit (ie, dry skin and mucous membranes, decreased skin turgor, oliguria,
exhaustion, decreased temperature, increased hematocrit, elevated urine
spe-cific gravity, and hypotension). It is important to encourage oral intake
of fluids and to monitor the intravenous flow rate. The nurse initiates
measures to decrease diarrhea (eg, dietary restrictions, stress reduction,
antidiarrheal agents).
MAINTAINING OPTIMAL NUTRITION
Parenteral
nutrition (PN) is used when the symptoms of IBD are severe. With PN, the nurse
maintains an accurate record of fluid intake and output as well as the
patient’s daily weight. The pa-tient should gain 0.5 kg daily during PN
therapy. Because PN is very high in glucose and can cause hyperglycemia, blood
glucose levels are monitored every 6 hours. Elemental feedings high in protein
and low in fat and residue are instituted after PN ther-apy because they are
digested primarily in the jejunum, do not stimulate intestinal secretions, and
allow the bowel to rest. The nurse notes intolerance if the patient exhibits
nausea, vomiting, diarrhea, or abdominal distention.
If
oral foods are tolerated, small, frequent, low-residue feed-ings are given to
avoid overdistending the stomach and stimu-lating peristalsis. It is important
for the patient to restrict activity to conserve energy, reduce peristalsis,
and reduce calorie requirements.
PROMOTING REST
The
nurse recommends intermittent rest periods during the day and schedules or
restricts activities to conserve energy and reduce the metabolic rate. It is
important to encourage activity within the limits of the patient’s capacity. The
nurse suggests bed rest for a patient who is febrile, has frequent diarrheal
stools, or is bleeding. The patient on bed rest should perform active exercises
to maintain muscle tone and prevent thromboembolic compli-cations. If the
patient is unable to perform these active exercises, the nurse performs passive
exercises and joint range of motion. Activity restrictions are modified as
needed on a day-to-day basis.
REDUCING ANXIETY
Rapport
can be established by being attentive and displaying a calm, confident manner.
The nurse allows time for the patient to ask questions and express feelings.
Careful listening and sensitiv-ity to nonverbal indicators of anxiety (eg,
restlessness, tense facial expressions) are helpful. The patient may be
emotionally labile because of the consequences of the disease; the nurse
tailors in-formation about possible impending surgery to the patient’s level of
understanding and desire for detail. If surgery is planned, pic-tures and
illustrations help to explain the surgical procedure and help the patient to
visualize what a stoma looks like.
ENHANCING COPING MEASURES
Because
the patient may feel isolated, helpless, and out of control, understanding and
emotional support are essential. The patient may respond to stress in a variety
of ways that may alienate others, including anger, denial, and social
self-isolation.
The
nurse needs to recognize that the patient’s behavior may be affected by a
number of factors unrelated to inherent emo-tional characteristics. Any patient
suffering the discomforts of frequent bowel movements and rectal soreness is
anxious, dis-couraged, and depressed. It is important to develop a relationship
with the patient that supports all attempts to cope with these stresses. It is
also important to communicate that the patient’s feelings are understood by
encouraging the patient to talk and ex-press his or her feelings and to discuss
any concerns. Stress re-duction measures that may be used include relaxation
techniques, visualization, breathing exercises, and biofeedback. Professional
counseling may be needed to help the patient and family manage issues
associated with chronic illness.
PREVENTING SKIN BREAKDOWN
The
nurse examines the patient’s skin frequently, especially the perianal skin.
Perianal care, including the use of a skin barrier, is important after each
bowel movement. The nurse gives immediate attention to reddened or irritated
areas over a bony prominence and uses pressure-relieving devices to prevent
skin breakdown. Consultation with a wound care specialist or enterostomal
ther-apist is often helpful.
MONITORING AND MANAGING POTENTIAL COMPLICATIONS
Serum
electrolyte levels are monitored daily, and electrolyte re-placements are
administered as prescribed. It is important to re-port evidence of dysrhythmias
or change in level of consciousness immediately.
The
nurse closely monitors rectal bleeding and administers blood component therapy
and volume expanders as prescribed to prevent hypovolemia. It is important to
monitor the blood pres-sure for hypotension and to obtain coagulation and
hematocrit and hemoglobin profiles frequently. Vitamin K may be prescribed to
increase clotting factors.
The
nurse closely monitors the patient for indications of per-foration (ie, acute
increase in abdominal pain, rigid abdomen, vomiting, or hypotension) and
obstruction and toxic megacolon (ie, abdominal distention, decreased or absent
bowel sounds, change in mental status, fever, tachycardia, hypotension,
dehy-dration, and electrolyte imbalances).
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care
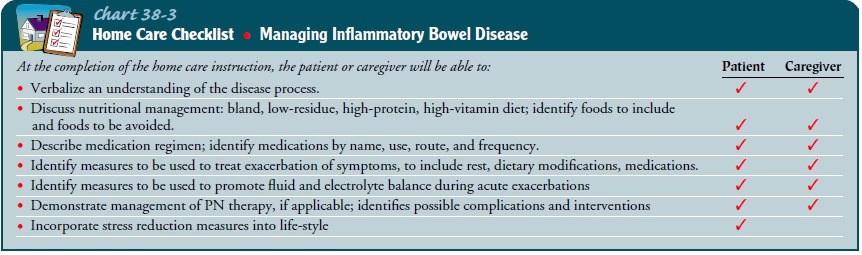
The
nurse assesses the patient’s understanding of the disease process and his or
her need for additional information about medical management (eg, medications,
diet) and surgical inter-ventions. The nurse provides information about
nutritional man-agement; a bland, low-residue, high-protein, high-calorie, and
high-vitamin diet relieves symptoms and decreases diarrhea. It is important to
provide the rationale for the use of corticosteroids and anti-inflammatory,
antibacterial, antidiarrheal, and antispas-modic medications. The nurse
emphasizes the importance of tak-ing medications as prescribed and not abruptly
discontinuing them (especially corticosteroids) to avoid development of serious
medical problems (Chart 38-3). The nurse reviews ileostomy care as necessary
(see Nursing Management of the Patient with an Ileostomy). Patient education
information can be obtained from the National Foundation for Ileitis and
Colitis.
Continuing Care
Patients
with chronic inflammatory disease are managed at home with follow-up care by
their physician or through an outpatient clinic. Those whose nutritional status
is compromised and who are receiving PN need home care nursing to ensure that
their nutri-tional requirements are being met and that they or their caregivers
can follow through with the instructions for PN. Patients who are medically
managed need to understand that their disease can be controlled and that they
can lead a healthy life between exacerba-tions. Control implies management
based on an understanding of the disease and its treatment. Patients in the
home setting need in-formation about their medications (ie, name, dose, side
effects, and frequency of administration) and need to take medications on
schedule. Medication reminders such as containers that separate pills according
to day and time or daily checklists are helpful.
During
a flare-up, the nurse encourages patients to rest as needed and to modify
activities according to their energy levels. Patients should limit tasks that
impose strain on the lower ab-dominal muscles. They should sleep in a room
close to the bath-room because of the frequent diarrhea (10 to 20 times per
day); quick access to a toilet helps alleviate the worry of embarrassment if an
accident occurs. Room deodorizers help control odors.
Dietary modifications can control but not cure the disease; the nurse recommends a low-residue, high-protein, high-calorie diet, especially during an acute phase. It is important to encourage pa-tients to keep a record of the foods that irritate the bowel and to eliminate them from the diet and to remind patients to drink at least eight glasses of water each day.
The
prolonged nature of the disease has an impact on the patient and often strains
his or her family life and financial resources as well. Family support is
vital; however, some family members may be re-sentful, guilty, and tired and
feel unable to continue coping with the emotional demands of the illness and
the physical demands of car-ing for another. Some patients with IBD do not
socialize for fear of being embarrassed. Many prefer to eat alone. Because they
have lost control over elimination, they may fear losing control over other
as-pects of their lives. They need time to express their fears and
frus-trations. Individual and family counseling may be helpful.
Evaluation
EXPECTED PATIENT OUTCOMES
Expected
patient outcomes may include the following:
1) Reports a decrease in
the frequency of diarrhea stools
a. Complies with dietary
restrictions; maintains bed rest
b. Takes medications as
prescribed
2) Has reduced pain
3) Maintains fluid volume
balance
a. Drinks 1 to 2 L of oral
fluids daily
b. Has a normal body
temperature
c. Displays adequate skin
turgor and moist mucous membranes
4) Attains optimal
nutrition; tolerates small, frequent feed-ings without diarrhea
5) Avoids fatigue
a. Rests periodically
during the day
b. Adheres to activity
restrictions
6) Is less anxious
7) Copes successfully with
diagnosis
a. Expresses feelings
freely
b. Uses appropriate stress
reduction behaviors
8) Maintains skin integrity
a. Cleans perianal skin
after defecation
b. Uses lotion or ointment
as skin barrier
9) Acquires an
understanding of the disease process
a. Modifies diet
appropriately to decrease diarrhea
b. Adheres to medication
regimen
10)
Recovers without complications
a. Maintains electrolytes
within normal ranges
b. Maintains normal sinus
or baseline cardiac rhythm
c. Maintains fluid balance
d. Experiences no
perforation or rectal bleeding
Related Topics