Chapter: Medical Surgical Nursing: Management of Patients With Gastric and Duodenal Disorders
Nursing Process: The Patient Undergoing Gastric Surgery
NURSING
PROCESS: THE PATIENT UNDERGOING GASTRIC SURGERY
Assessment
Before
surgery, the nurse assesses the patient’s and family’s knowledge of
preoperative and postoperative surgical routines and the rationale for surgery.
The nurse also assesses the patient’s nutritional status: Has the patient lost
weight? How much? Over how much time? Does the patient have nausea and
vomiting? Has the patient had hematemesis? The nurse assesses for the presence
of bowel sounds and palpates the abdomen to detect masses or tenderness.
After
surgery, the nurse assesses the patient for complications secondary to the
surgical intervention, such as hemorrhage, in-fection, abdominal distention, or
decreased nutritional status.
Diagnosis
NURSING DIAGNOSES
Based
on the assessment data, the patient’s major nursing diag-noses may include the
following:
•
Anxiety related to surgical intervention
•
Acute pain related to surgical incision
•
Deficient knowledge about surgical procedures and
post-operative course
•
Imbalanced nutrition, less than body requirements,
related to poor nutrition before surgery and altered GI system after surgery
COLLABORATIVE PROBLEMS/POTENTIAL COMPLICATIONS
In
addition to the complications to which all postoperative pa-tients are subject,
the patient undergoing gastric surgery is at in-creased risk for:
•
Hemorrhage
•
Dietary deficiencies
•
Bile reflux
•
Dumping syndrome
Planning and Goals
The
major goals for the patient undergoing gastric surgery may include reduced
anxiety, increased knowledge and understanding about the surgical procedure and
postoperative course, optimal nutrition and management of the complications
that can inter-fere with nutrition, relief of pain, avoidance of hemorrhage and
steatorrhea, and enhanced self-care skills at home.
Nursing Interventions
REDUCING ANXIETY
An
important part of the preoperative nursing care involves allaying the patient’s
fears and anxieties about the impending surgery and its implications. The nurse
encourages the patient to express feelings and answers the patient’s and
family’s questions. If the patient has an acute obstruction, a perforated
bowel, or an active GI hemor-rhage, adequate psychological preparation may not
be possible. In this event, the nurse caring for the patient after surgery
should an-ticipate the concerns, fears, and questions that are likely to
surface and should be available for support and further explanations.
RELIEVING PAIN
After
surgery, analgesics may be administered as prescribed to re-lieve pain and
discomfort. It is important to avoid sedating the pa-tient so as not to impair
his or her ability to perform pulmonary care activities (deep breathing and
coughing) and to ambulate. The nurse assesses the effectiveness of analgesic
intervention. Position-ing the patient in a Fowler’s position promotes comfort
and allows emptying of the stomach after a partial gastrectomy.
The
nurse maintains functioning of the NG tube to prevent dis-tention and resultant
pain and damage to the suture line. Normally, the amount of NG drainage after a
total gastrectomy is small.
INCREASING KNOWLEDGE
The
nurse explains routine preoperative and postoperative activ-ities to the
patient, which include preoperative medications, NG intubation, IV fluids,
abdominal dressings, and pulmonary care. These explanations need to be
reinforced after surgery, especially if the patient had emergency surgery.
RESUMING ENTERAL INTAKE
The
patient’s nutritional status is evaluated before surgery, be-cause many
patients with gastric cancer are malnourished and may require preoperative enteral
or, more often, parenteral nu-trition. After surgery, parenteral nutrition may
be continued to meet caloric needs, to replace fluids lost through drainage and
vomitus, and to support the patient metabolically until oral intake is
adequate.
After
the return of bowel sounds and removal of the NG tube, the nurse may give
fluids, followed by food in small portions. The nurse adds foods gradually
until the patient is able to eat six small meals a day and drink 120 mL of
fluid between meals. The key to increasing the dietary content is to offer food
and fluids gradually as tolerated and to recognize that each patient’s
tolerance is different.
RECOGNIZING OBSTACLES TO ADEQUATE NUTRITION
Dysphagia and Gastric Retention
Dysphagia
may occur in patients who have had truncal vagot-omy, a surgical procedure that
can result in trauma to the lower esophagus. Gastric retention may be evidenced
by abdominal dis-tention, nausea, and vomiting. Regurgitation may also occur if
the patient has eaten too much or too quickly. It also may indi-cate that edema
along the suture line is preventing fluids and food from moving into the
intestinal tract. If gastric retention occurs, it may be necessary to reinstate
NG suction; pressure must be low to avoid disrupting the suture line.
Bile Reflux
Bile
reflux gastritis and esophagitis may occur with the removal of the pylorus,
which acts as a barrier to the reflux of duodenal con-tents. Burning epigastric
pain and vomiting of bilious material manifest this condition. Eating or vomiting
does not relieve the situation. Agents that bind with bile acid, such as
cholestyramine (Questran), may be helpful. Aluminum hydroxide gel (an antacid)
and metoclopramide hydrochloride (Reglan) have been used with some success.
Dumping Syndrome
The
term dumping syndrome refers to an
unpleasant set of vasomotor and GI symptoms that sometimes occur in patients
who have had gastric surgery or a form of vagotomy. It may be the mechanical
result of surgery in which a small gastric remnant is connected to the jejunum
through a large opening. Foods high in carbohydrates and electrolytes must be
diluted in the jejunum before absorption can take place, but the passage of
food from the stomach remnant into the jejunum is too rapid to allow this to
happen. The symptoms that occur are probably a result of rapid distention of
the jejunal loop anastomosed to the stomach. The hypertonic intestinal contents
draw extracellular fluid from the circulating blood volume into the jejunum to
dilute the high con-centration of electrolytes and sugars. The ingestion of
fluid at meal-time is another factor that causes the stomach contents to empty
rapidly into the jejunum.
Early
symptoms include a sensation of fullness, weakness, faint-ness, dizziness,
palpitations, diaphoresis, cramping pains, and diar-rhea. Later, there is a
rapid elevation of blood glucose, followed by increased insulin secretion. This
results in a reactive hypoglycemia, which also is unpleasant for the patient.
Vasomotor symptoms that occur 10 to 90 minutes after eating are pallor,
perspiration, palpita-tions, headache, and feelings of warmth, dizziness, and
even drowsi-ness. Anorexia may also be a result of the dumping syndrome.
Steatorrhea
also may occur in the patient with gastric surgery. It is partially the result
of rapid gastric emptying, which prevents adequate mixing with pancreatic and
biliary secretions. In mild cases, reducing the intake of fat and administering
an antimotility medication can control steatorrhea.
Vitamin and Mineral Deficiencies
Other
dietary deficiencies the nurse should be aware of include malabsorption of
organic iron, which may require supplementa-tion with oral or parenteral iron,
and a low serum level of vitamin B12, which may require supplementation by the
intramuscular route. Total gastrectomy results in lack of intrinsic factor, a
gas-tric secretion required for the absorption of vitamin B12 from the GI tract.
Unless this vitamin is supplied by parenteral injection after gastrectomy, the
patient inevitably will suffer vitamin B12 de-ficiency, which eventually leads to a
condition identical to perni-cious anemia. All manifestations of pernicious
anemia, including macrocytic anemia and combined system disease, may be
expected to develop within a period of 5 years or less; they progress in
sever-ity thereafter and, in the absence of therapy, are fatal. This
com-plication is avoided by the regular monthly intramuscular injection of 100
to 1000 μ g (usual dose is 300 μ g) of vitamin B12.This regimen should be started without delay
after gastrectomy. Weight loss is a common long-term problem because the
patient experiences early fullness, which suppresses the appetite.
TEACHING DIETARY SELF-MANAGEMENT
Because
the patient may experience any of the described conditions affecting nutrition,
nursing intervention includes proper dietary in-struction. The following
teaching points are emphasized:
•
To delay stomach emptying, the patient should
assume a low Fowler’s position during mealtime, and after the meal the patient
should lie down for 20 to 30 minutes.
•
Antispasmodics, as prescribed, also may aid in
delaying the emptying of the stomach.
•
Fluid intake with meals is discouraged; instead,
fluids may be consumed up to 1 hour before or 1 hour after mealtime.
•
Meals should contain more dry items than liquid
items.
•
The patient can eat fat as tolerated but should
keep carbo-hydrate intake low and avoid concentrated sources of car-bohydrates.
•
The patient should eat smaller but more frequent
meals.
•
Dietary supplements of vitamins and medium-chain
triglycerides and injections of vitamin B12 and iron may be prescribed.
The
nurse also gives instructions regarding enteral or pa-renteral supplementation
if it is needed.
MONITORING AND MANAGING
POTENTIAL COMPLICATIONS
Occasionally
hemorrhage complicates gastric surgery. The pa-tient has the usual signs of
rapid blood loss and shock and may vomit considerable amounts of bright red
blood. The nurse assesses NG drainage for type and amount; some bloody drainage
for the first 12 hours is expected, but excessive bleeding should be reported.
The nurse also assesses the abdom-inal dressing for bleeding. Because this
situation is upsetting to the patient and family, the nurse should remain calm.
The nurse performs emergency measures, such as NG lavage and adminis-tration of
blood and blood products.
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care
Nurse-patient
teaching stems from the assessment of the patient’s physical and psychological
readiness to participate in self-care. The nurse provides information about
nutrition, enteral or parenteral nutrition if required, nutritional
supplements, pain management, and the symptoms of dumping syndrome and measures
to use to prevent or minimize these symptoms (Chart 37-4). It is important to
emphasize the continued need for vitamin B12 injections.
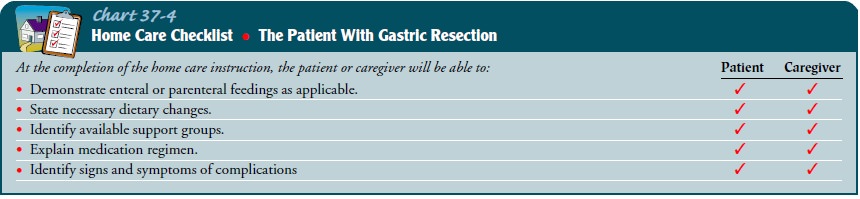
Continuing Care
Both
the patient and the family can benefit from a team approach to discharge
planning. The team members include the home care nurse, physician, dietitian,
social worker, patient and family; written instructions about meals,
activities, medications, and follow-up care are helpful. The home care nurse
supervises the administration of any enteral or parenteral feedings,
emphasizing information about detection and prevention of untoward effects or
complications related to the feedings. Information about commu-nity support
groups is provided to the patient and family.
Evaluation
EXPECTED PATIENT OUTCOMES
Expected
patient outcomes may include:
1) Reports decreased
anxiety; expresses fears and concerns about surgery
2) Demonstrates knowledge
regarding postoperative course by discussing the surgical procedure and
postoperative course
3) Attains optimal
nutrition
a.
Maintains a reasonable weight
b.
Does not have excessive diarrhea
c.
Tolerates 6 small meals a day
d.
Does not experience dysphagia, gastric retention,
bile reflux, dumping syndrome, or vitamin and mineral deficiencies
4) Attains optimal level of
comfort
5) Has no evidence of
hemorrhage
Related Topics