Chapter: Medical Surgical Nursing: Management of Patients With Gastric and Duodenal Disorders
Morbid Obesity
Morbid Obesity
One in
three Americans is 20% or more over his or her ideal body weight (U.S.
Department of Health and Human Services, 2001). Morbid obesity is the term applied to people who are more than two
times their ideal body weight or whose body mass index (BMI) exceeds 30 kg/m2.
Another
definition of morbid obesity is body weight that is more than 100 pounds
greater than the ideal body weight (Monteforte & Turkelson, 2000). Patients
with morbid obesity are at higher risk for health complications, such as
cardiovascular disease, arthritis, asthma, bronchitis, and diabetes. They
fre-quently suffer from low self-esteem, impaired body image, and depression.
Medical Management
Conservative
management consists of placing the person on a weight loss diet in conjunction
with behavioral modification and exercise; however, diet therapy is usually
unsuccessful. There is a belief that depression may be a contributing factor to
weight gain, and treatment of the depression with bupropion hydrochloride
(Wellbutrin) may be helpful (Wangsness, 2000). Some physicians recommend
acupuncture and hypnosis before recommending surgery.
PHARMACOLOGIC MANAGEMENT
Several
medications have recently been approved for obesity. They include sibutramine
HCl (Meridia) and orlistat (Xenical). By inhibiting the reuptake of serotonin
and norepinephrine, sibutramine decreases appetite. Orlistat reduces caloric
intake by binding to gastric and pancreatic lipase to prevent digestion of
fats. Both medications require a physician’s prescription. Sibutramine may
increase blood pressure and should not be taken by people with a history of
coronary artery disease, angina pectoris, dysrhythmias, or kidney disease; by
those taking antidepressants or monoamine oxidase inhibitors; or by pregnant or
nursing women. Side effects may include dry mouth, insomnia, headache,
increased sweating, and increased heart rate. Side effects of orlistat may
include in-creased bowel movements, gas with oily discharge, decreased food
absorption, decreased bile flow, and decreased absorption of some vitamins. A
multivitamin is usually recommended for patients taking orlistat. Women who are
pregnant or nursing should not take orlistat (Hussar, 2000).
SURGICAL MANAGEMENT
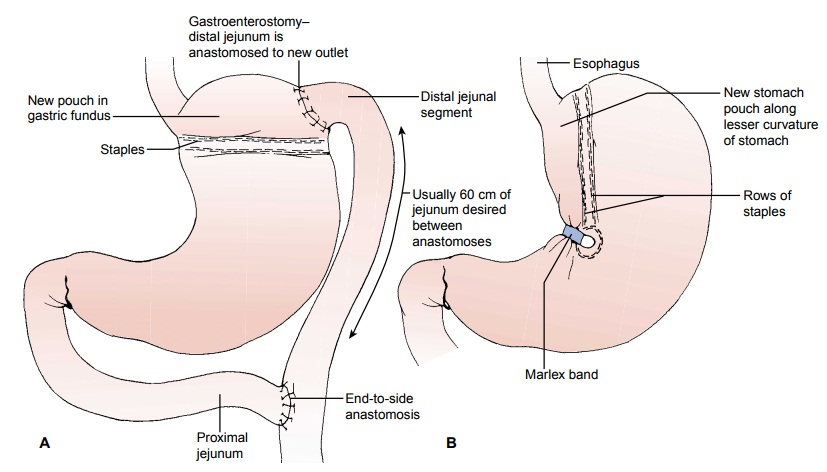
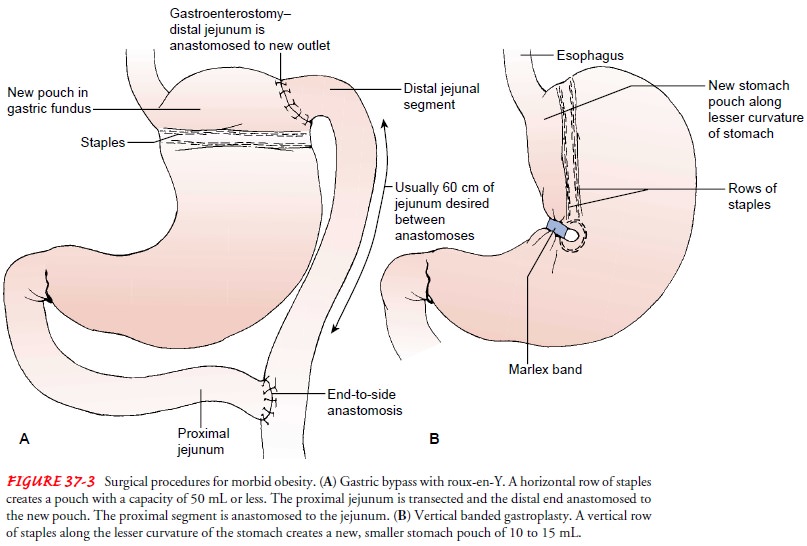
Bariatric
surgery, or surgery for morbid obesity, is performed only after other nonsurgical
attempts at weight control have failed. The first surgical procedure to treat
morbid obesity was the je-junoileal bypass. This procedure, which resulted in
significant complications, has been largely replaced by gastric restriction
pro-cedures. Gastric bypass and vertical banded gastroplasty are the current
operations of choice. These procedures may be performed laparoscopically or by
an open surgical technique.
In
gastric bypass surgery, the proximal segment of the stomach is transected to
form a small pouch with a small gastroenterostomy stoma. The Roux-en-Y gastric
bypass is the recommended proce-dure for long-term weight loss. In this
procedure, a horizontal row of staples creates a stomach pouch with a 1-cm
stoma that is anas-tomosed with a portion of distal jejunum, creating a
gastro-enterostomy. The transected proximal portion of the jejunum is
anastomosed to the distal jejunum (Fig. 37-3A).
In
vertical banded gastroplasty, a double row of staples is ap-plied vertically
along the lesser curvature of the stomach, begin-ning at the angle of His. A
small stoma is created at the end of the staples by adding a circle of staples
or a band of polypropylene mesh or silicone tubing (see Fig. 37-3B).
After
weight loss, the patient may need surgical intervention for body contouring.
This may include lipoplasty to remove fat deposits or a panniculectomy to
remove excess abdominal skinfolds.
Nursing Management
Nursing
management focuses on care of the patient after surgery. General postoperative
nursing care is similar to that for a patient recovering from a gastric
resection, but with attention given to the risks of complications associated
with morbid obesity. Complica-tions that may occur in the immediate
postoperative period in-clude peritonitis, stomal obstruction, stomal ulcers,
atelectasis and pneumonia, thromboembolism, and metabolic imbalances result-ing
from prolonged vomiting and diarrhea. After bowel sounds have returned and oral
intake is resumed, the nurse provides six Small feedings consisting of a total
of 600 to 800 calories per day and encourages fluid intake to prevent
dehydration.
Patients
are usually discharged in 4 to 5 days with detailed di-etary instructions. The
nurse instructs patients to report excessive thirst or concentrated urine, both
of which are indications of de-hydration. Psychosocial interventions are also
essential for these pa-tients. Efforts are directed toward helping them modify
their eating behaviors and cope with changes in body image. The nurse explains
that noncompliance by eating too much or too fast or eating high-calorie liquid
and soft foods results in vomiting and painful esophageal distention. The nurse
discusses dietary instructions be-fore discharge and schedules monthly
outpatient visits. Long-term side effects may include increased risk of
gallstones, nutritional de-ficiencies, and potential to regain weight.
Related Topics