Chapter: Medical Surgical Nursing: Management of Patients With Gastric and Duodenal Disorders
Nursing Process: The Patient With Ulcer Disease
NURSING
PROCESS:THE PATIENT WITH ULCER DISEASE
Assessment
The
nurse asks the patient to describe the pain and the methods used to relieve it
(e.g., food, antacids). The patient usually describes peptic ulcer pain as
burning or gnawing; it occurs about 2 hours after a meal and frequently awakens
the patient between midnight and 3 AM. Taking antacids,
eating, or vomiting often relieves the pain. If the patient reports a recent
history of vomiting, the nurse determines how often emesis has occurred and
notes important characteristics of the vomitus: Is it bright red, does it
resemble coffee grounds, or is there undigested food from previous meals? Has
the patient noted any bloody or tarry stools?
The
nurse also asks the patient to list his or her usual food in-take for a 72-hour
period and to describe food habits (e.g., speed of eating, regularity of meals,
preference for spicy foods, use of sea-sonings, use of caffeinated beverages
and decaffeinated coffee). Lifestyle and habits are a concern as well. Does the
patient use irri-tating substances? For example, does he or she smoke
cigarettes? If yes, how many? Does the patient ingest alcohol? If yes, how much
and how often? Are NSAIDs used? The nurse inquires about the patient’s level of
anxiety and his or her perception of current stres-sors. How does the patient
express anger or cope with stressful sit-uations? Is the patient experiencing
occupational stress or problems within the family? Is there a family history of
ulcer disease?
The
nurse assesses vital signs and reports tachycardia and hypotension, which may
indicate anemia from GI bleeding. The stool is tested for occult blood, and a
physical examination, in-cluding palpation of the abdomen for localized
tenderness, is per-formed as well.
Diagnosis
NURSING DIAGNOSES
Based
on the assessment data, the patient’s nursing diagnoses may include the
following:
•
Acute pain related to the effect of gastric acid
secretion on damaged tissue
•
Anxiety related to coping with an acute disease
•
Imbalanced nutrition related to changes in diet
•
Deficient knowledge about prevention of symptoms
and management of the condition
COLLABORATIVE PROBLEMS/POTENTIAL COMPLICATIONS
Potential
complications may include the following:
•
Hemorrhage
•
Perforation
•
Penetration
•
Pyloric obstruction (gastric outlet obstruction)
Planning and Goals
The
goals for the patient may include relief of pain, reduced anx-iety, maintenance
of nutritional requirements, knowledge about the management and prevention of
ulcer recurrence, and absence of complications.
Nursing Interventions
RELIEVING PAIN
Pain
relief can be achieved with prescribed medications. The patient should avoid
aspirin, foods and beverages that contain caffeine, and decaffeinated coffee,
and meals should be eaten at regularly paced intervals in a relaxed setting.
Some patients benefit from learning relaxation techniques to help manage stress
and pain and to en-hance smoking cessation efforts.
REDUCING ANXIETY
The
nurse assesses the patient’s level of anxiety. Patients with pep-tic ulcers are
usually anxious, but their anxiety is not always obvi-ous. Appropriate
information is provided at the patient’s level of understanding, all questions
are answered, and the patient is en-couraged to express fears openly.
Explaining diagnostic tests and administering medications on schedule also help
to reduce anxi-ety. The nurse interacts with the patient in a relaxed manner,
helps identify stressors, and explains various coping techniques and relaxation
methods, such as biofeedback, hypnosis, or be-havior modification. The
patient’s family is also encouraged to participate in care and to provide
emotional support.
MAINTAINING OPTIMAL NUTRITIONAL STATUS
The
nurse assesses the patient for malnutrition and weight loss. After recovery
from an acute phase of peptic ulcer disease, the pa-tient is advised about the
importance of complying with the med-ication regimen and dietary restrictions.
MONITORING AND MANAGING POTENTIAL COMPLICATIONS
Hemorrhage
Gastritis
and hemorrhage from peptic ulcer are the two most common causes of upper GI
tract bleeding. Hemorrhage, the most common complication, occurs in about 15%
of patients with peptic ulcers (Yamada, 1999). The site of bleeding is usually
the distal portion of the duodenum. Bleeding may be manifested by hematemesis
or melena (tarry stools). The vomited
blood can be bright red, or it can have a “coffee grounds” appearance (which is
dark) from the oxidation of hemoglobin to methemoglobin. When the hemorrhage is
large (2000 to 3000 mL), most of the blood is vomited. Because large quantities
of blood may be lost quickly, immediate correction of blood loss may be
required to prevent hemorrhagic shock. When the hemorrhage is small, much or
all of the blood is passed in the stools, which will appear tarry black because
of the digested hemoglobin. Management depends on the amount of blood lost and
the rate of bleeding.
The
nurse assesses the patient for faintness or dizziness and nausea, which may
precede or accompany bleeding. It is impor-tant to monitor vital signs
frequently and to evaluate the patient for tachycardia, hypotension, and
tachypnea. Other nursing in-terventions include monitoring the hemoglobin and
hematocrit, testing the stool for gross or occult blood, and recording hourly
urinary output to detect anuria or oliguria (absence or decreased urine
production).
Many
times the bleeding from a peptic ulcer stops sponta-neously; however, the
incidence of recurrent bleeding is high. Because bleeding can be fatal, the
cause and severity of the hem-orrhage must be identified quickly and the blood
loss treated to prevent hemorrhagic shock. Management of upper GI tract
bleeding consists of quickly determining the amount of blood lost and the rate
of bleeding, rapidly replacing the blood that has been lost, stopping the
bleeding, stabilizing the patient, and di-agnosing and treating the cause.
Related nursing and collabora-tive interventions include the following:
•
Inserting a peripheral IV line for the infusion of
saline or lactated Ringer’s solution and blood products. The nurse may need to
assist with the placement of a pulmonary artery catheter for hemodynamic
monitoring. Blood component therapy is initiated if there are signs of shock
(eg, tachycar-dia, sweating, coldness of the extremities).
•
Monitoring the hemoglobin and hematocrit to assist
in evaluating blood loss
•
Inserting an NG tube to distinguish fresh blood
from “coffee grounds” material, to aid in the removal of clots and acid, to
prevent nausea and vomiting, and to provide a means of monitoring further
bleeding
•
Administering a room-temperature lavage of saline
solution or water. This is controversial; some authorities recommend using ice
lavage (Yamada, 1999).
•
Inserting an indwelling urinary catheter and
monitoring urinary output
•
Monitoring vital signs and oxygen saturation and
adminis-tering oxygen therapy
•
Placing the patient in the recumbent position with
the legs elevated to prevent hypotension; or, to prevent aspiration from
vomiting, placing the patient on the left side
•
Treating hemorrhagic shock
If
bleeding cannot be managed by the measures described, other treatment
modalities may be used. Transendoscopic coagulation by laser, heat probe,
medication, a sclerosing agent, or a combina-tion of these therapies can halt
bleeding and make surgical inter-vention unnecessary. There is much debate
regarding how soon endoscopy should be performed. Some believe that endoscopy
should be performed in the first 24 hours after hemorrhage has been stabilized.
Others believe that endoscopy may be performed during acute bleeding, as long
as the esophageal or gastric area can be visualized (blood may decrease
visibility) (Yamada, 1999).
For
those who are unable to undergo surgery, selective em-bolization may be used.
This procedure involves forcing emboli of autologous blood clots with or
without Gelfoam (absorbable gelatin sponge) through a catheter in the artery to
a point above the bleeding lesion. A radiologist performs this procedure.
Rebleeding may occur and often warrants
surgical intervention. The nurse monitors the patient carefully so that bleeding
can be detected quickly. Signs of bleeding include tachycardia, tachypnea,
hypotension, mental confusion, thirst, and oliguria. If bleeding re-curs within
48 hours after medical therapy has begun, or if more than 6 to 10 units of
blood are required within 24 hours to main-tain blood volume, the patient is
likely to require surgery. Some physicians recommend surgical intervention if a
patient hemor-rhages three times. Other criteria for surgery are the patient’s
age (massive hemorrhaging is three times more likely to be fatal in those older
than 60 years of age); a history of chronic duodenal ulcer; and a coincidental
gastric ulcer (Yamada, 1999). The area of the ulcer is removed or the bleeding
vessels are ligated. Many patients also undergo procedures (eg, vagotomy and
pyloroplasty, gastrectomy) aimed at controlling the underlying cause of the
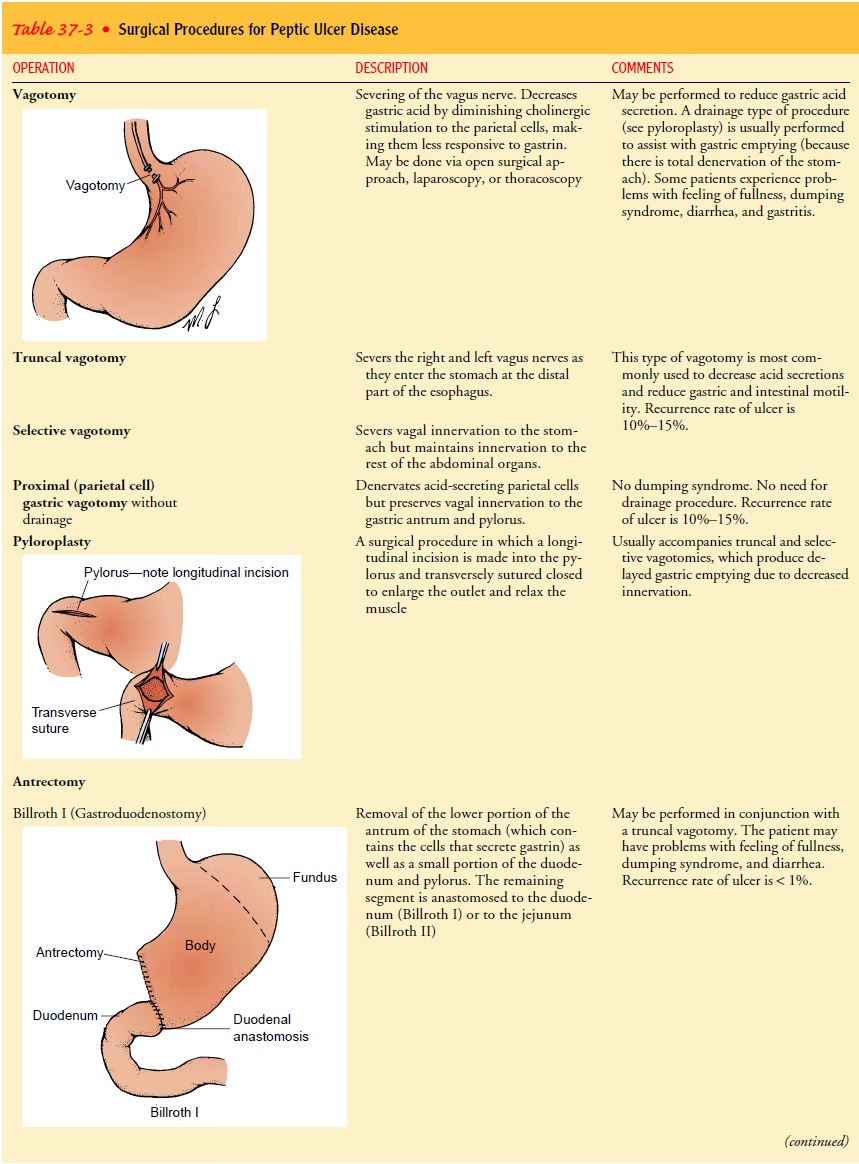
ulcers (see Table 37-3).

Perforation and Penetration
Perforation
is the erosion of the ulcer through the gastric serosa into the peritoneal
cavity without warning. It is an abdominal cat-astrophe and requires immediate
surgery. Penetration is erosion of the ulcer through the gastric serosa into
adjacent structures such as the pancreas, biliary tract, or gastrohepatic
omentum. Symp-toms of penetration include back and epigastric pain not relieved
by medications that were effective in the past. Like perforation, penetration
usually requires surgical intervention.
Signs
and symptoms of perforation include the following:
•
Sudden, severe upper abdominal pain (persisting and
in-creasing in intensity); pain may be referred to the shoulders, especially
the right shoulder, because of irritation of the phrenic nerve in the
diaphragm.
•
Vomiting and collapse (fainting)
•
Extremely tender and rigid (boardlike) abdomen
•
Hypotension and tachycardia, indicating shock
Because
chemical peritonitis develops within a few hours after perforation and is
followed by bacterial peritonitis, the perfora-tion must be closed as quickly
as possible. In a few patients, it may be deemed safe and advisable to perform
surgery for the ulcer dis-ease in addition to suturing the perforation.
Postoperatively,
the stomach contents are drained by means of an NG tube. The nurse monitors
fluid and electrolyte balance and assesses the patient for peritonitis or
localized infection (in-creased temperature, abdominal pain, paralytic ileus,
increased or absent bowel sounds, abdominal distention). Antibiotic therapy is
administered parenterally as prescribed.
Pyloric Obstruction
Pyloric
obstruction, also called gastric outlet obstruction (GOO), occurs when the area
distal to the pyloric sphincter becomes scarred and stenosed from spasm or
edema or from scar tissue that forms when an ulcer alternately heals and breaks
down. The pa-tient has nausea and vomiting, constipation, epigastric fullness,
anorexia, and, later, weight loss.
In
treating the patient with pyloric obstruction, the first con-sideration is to
insert an NG tube to decompress the stomach. Con-firmation that obstruction is
the cause of the discomfort is accomplished by assessing the amount of fluid
aspirated from the NG tube. A residual of more than 400 mL strongly suggests
ob-struction. Usually an upper GI study or endoscopy is performed to confirm
gastric outlet obstruction. Decompression of the stomach and management of
extracellular fluid volume and electrolyte bal-ances may improve the patient’s
condition and avert the need for surgical intervention. A balloon dilatation of
the pylorus via endoscopy may be beneficial. If the obstruction is unrelieved
by medical management, surgery (in the form of a vagotomy and antrectomy or gastrojejunostomy and
vagotomy) may be required.
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care
To manage ulcer disease successfully, the patient is instructed about the factors that will help or aggravate the condition (Chart 37-2). The nurse reviews information about medications to be taken at home, including name, dosage, frequency, and possible side ef-fects, stressing the importance of continuing to take medications even after signs and symptoms have decreased or subsided.
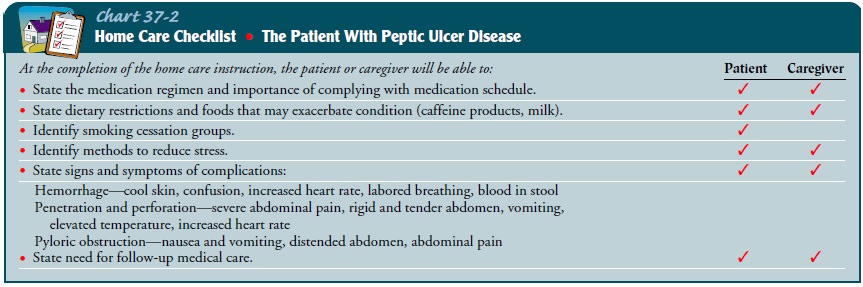
Then the patient is instructed to avoid certain
medications and foods that exacerbate symptoms as well as substances that have
acid-producing potential (eg, alcohol; caffeinated beverages such as coffee,
tea, and colas). It is important to counsel the patient to eat meals at regular
times and in a relaxed setting, and to avoid overeating. If relevant, the nurse
also informs the patient about the irritant effects of smoking on the ulcer and
provides infor-mation about smoking cessation programs.
The
nurse reinforces the importance of follow-up care for ap-proximately 1 year,
the need to report recurrence of symptoms, and the need for treating possible
problems that occur after surgery, such as intolerance to dairy products and
sweet foods.
Evaluation
EXPECTED PATIENT OUTCOMES
Expected
patient outcomes may include the following:
1) Reports freedom from
pain between meals
2) Feels less anxiety by
avoiding stress
3) Complies with
therapeutic regimen
a.
Avoids irritating foods and beverages
b.
Eats regularly scheduled meals
c.
Takes prescribed medications as scheduled
d.
Uses coping mechanisms to deal with stress
4) Maintains weight
5) Is free of complications
Related Topics