Chapter: Medical Surgical Nursing: Management of Patients With Gastric and Duodenal Disorders
Nursing Process: The Patient With Gastritis
NURSING
PROCESS: THE PATIENT WITH GASTRITIS
Assessment
When obtaining the history, the nurse asks about the patient’s presenting signs and symptoms. Does the patient have heartburn, indigestion, nausea, or vomiting? Do the symptoms occur at any
specific time of the day, before or after meals, after ingesting spicy or
irritating foods, or after the ingestion of cer-tain drugs or alcohol? Has
there been recent weight gain or loss? Are the symptoms related to anxiety,
stress, allergies, eat-ing or drinking too much, or eating too quickly? How are
the symptoms relieved? Is there a history of previous gastric disease or surgery?
A diet history plus a 72-hour dietary recall (a list of everything the patient
ate and drank in the last 72 hours) may be helpful.
A
thorough history is important because it helps the nurse to identify whether
known dietary excesses or other indiscretions are associated with the current
symptoms, whether others in the pa-tient’s environment have similar symptoms,
whether the patient is vomiting blood, and whether any known caustic element
has been ingested. The nurse also identifies the duration of the cur-rent
symptoms, any methods used by the patient to treat these symptoms, and whether
the methods are effective. Signs to note during the physical examination
include abdominal tenderness, dehydration, and evidence of any systemic
disorder that might be responsible for the symptoms of gastritis.
Nursing Diagnoses
Based
on the assessment data, the patient’s major nursing diag-noses may include the
following:
•
Anxiety related to treatment
•
Imbalanced nutrition, less than body requirements,
related to inadequate intake of nutrients
•
Risk for imbalanced fluid volume related to
insufficient fluid intake and excessive fluid loss subsequent to vomiting
•
Deficient knowledge about dietary management and
disease process
•
Acute pain related to irritated stomach mucosa
Planning and Goals
The
major goals for the patient may include reduced anxiety, avoidance of
irritating foods, adequate intake of nutrients, mainte-nance of fluid balance,
increased awareness of dietary management, and relief of pain.
Nursing Interventions
REDUCING ANXIETY
If the
patient has ingested acids or alkalis, emergency measures may be needed. The
nurse offers supportive therapy to the patient and family during treatment and
after the ingested acid or alkali has been neutralized or diluted. In some
cases, the nurse may need to prepare the patient for additional diagnostic
studies (endoscopy) or surgery. The patient usually feels anxious about the
pain and the treatment modalities. The nurse uses a calm approach to assess the
patient and to answer all questions as completely as possible. It is important
to explain all procedures and treatments according to the patient’s level of
understanding.
PROMOTING OPTIMAL NUTRITION
For acute gastritis, the nurse provides physical and emotional sup-port and helps the patient manage the symptoms, which may include nausea, vomiting, heartburn, and fatigue. The patient should take no foods or fluids by mouth—possibly for days—until the acute symptoms subside, thus allowing the gastric mucosa to heal. If IV therapy is necessary, the nurse monitors it regularly, along with serum electrolyte values. After the symptoms sub-side, the nurse can offer the patient ice chips followed by clear liquids. Introducing solid food as soon as possible will provide oral nutrition, decrease the need for IV therapy, and minimize irri-tation to the gastric mucosa. As food is introduced, the nurse evaluates and reports any symptoms that suggest a repeat episode of gastritis.
The
nurse discourages the intake of caffeinated beverages, be-cause caffeine is a
central nervous system stimulant that increases gastric activity and pepsin
secretion. It also is important to dis-courage alcohol use. Discouraging cigarette
smoking is important because nicotine reduces the secretion of pancreatic
bicarbonate and thus inhibits the neutralization of gastric acid in the
duodenum (Eastwood, 1997). When appropriate, the nurse refers the patient for
alcohol counseling and smoking cessation programs.
PROMOTING FLUID BALANCE
Daily
fluid intake and output are monitored to detect early signs of dehydration
(minimal urine output of 30 mL/hour, minimal intake of 1.5 L/day). If food and
fluids are withheld, IV fluids (3 L/day) usually are prescribed and a record of
fluid intake plus caloric value (1 L of 5% dextrose in water = 170 calories of carbohydrate) needs to be
maintained. Electrolyte values (sodium, potassium, chloride) are assessed every
24 hours to detect imbalance.
The
nurse must always be alert for any indicators of hemor-rhagic gastritis, which
include hematemesis (vomiting of
blood), tachycardia, and hypotension. If these occur, the physician is
noti-fied and the patient’s vital signs are monitored as the patient’s
con-dition warrants. Guidelines for managing upper GI tract bleeding are
discussed later.
RELIEVING PAIN
Measures
to help relieve pain include instructing the patient to avoid foods and
beverages that may be irritating to the gastric mucosa (described earlier) and
instructing the patient about using medications to relieve chronic gastritis.
To follow up, the nurse assesses the patient’s level of pain and the extent of
comfort at-tained from the use of medications and avoidance of irritating
substances.
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care
The
nurse evaluates the patient’s knowledge about gastritis and de-velops an
individualized teaching plan that includes information about stress management,
diet, and medications (Chart 37-1). Dietary instructions take into account the
patient’s daily caloric needs, food preferences, and pattern of eating. The
nurse and pa-tient review foods and other substances to be avoided (eg, spicy,
irritating, or highly seasoned foods; caffeine; nicotine; alcohol).
Consultation with a dietitian may be recommended.
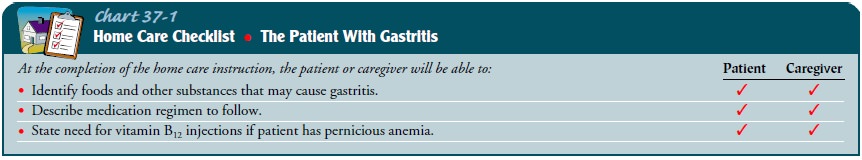
Providing
information about prescribed antibiotics, bismuth salts, medications to
decrease gastric secretion, and medications to protect mucosal cells from
gastric secretions can help the pa-tient recover and prevent recurrence.
Patients with pernicious anemia need information about long-term vitamin B12 injections; the nurse
may instruct a family member about administering these injections or make
arrangements for the patient to receive the in-jections from a health care
provider. Finally, the nurse empha-sizes the importance of keeping follow-up
appointments with health care providers.
Evaluation
EXPECTED PATIENT OUTCOMES
Expected
patient outcomes may include the following:
1) Exhibits less anxiety
2) Avoids eating irritating
foods or drinking caffeinated bev-erages or alcohol
3) Maintains fluid balance
a.
Has intake of at least 1.5 L daily
b. Drinks six to eight glasses of water daily
c. Has a urinary output of about 1 L daily
d. Displays adequate skin turgor
4. Adheres to medical regimen
a. Selects nonirritating foods and beverages
b. Takes medications as prescribed
5. Maintains appropriate weight
6. Reports less pain
Related Topics