Chapter: Medical Surgical Nursing: Management of Patients With Gastric and Duodenal Disorders
Gastritis
Gastritis
Gastritis (inflammation of the gastric or
stomach mucosa) is a com-mon GI problem. Gastritis may be acute, lasting
several hours to a few days, or chronic, resulting from repeated exposure to
irritating agents or recurring episodes of acute gastritis. Acute gastritis is
often caused by dietary indiscretion—the person eats food that is contaminated
with disease-causing microorganisms or that is irritating or too highly
seasoned. Other causes of acute gastritis include overuse of aspirin and other
nonsteroidal anti-inflammatory drugs (NSAIDs), excessive alcohol intake, bile
reflux, and radiation therapy. A more severe form of acute gastritis is caused
by the ingestion of strong acid or alkali, which may cause the mucosa to become
gangrenous or to perforate. Scarring can occur, resulting in pyloric obstruction.
Gastritis also may be the first sign of an acute systemic infection.
Chronic gastritis and prolonged inflammation
of the stomach may be caused by either benign or malignant ulcers of the
stomach or by the bacteria Helicobacter pylori. Chronic gastritis is sometimes
associated with autoimmune diseases such as pernicious anemia; dietary factors
such as caffeine; the use of medications, especially NSAIDs; alcohol; smoking;
or reflux of intestinal contents into the stomach.
Pathophysiology
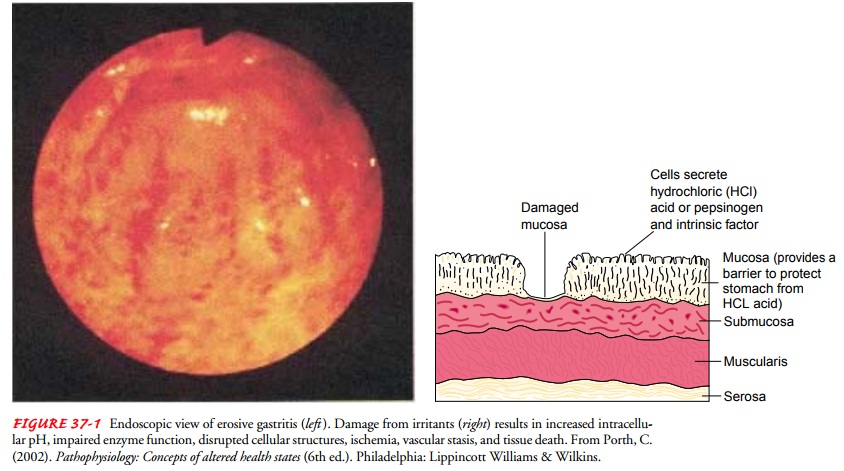
In gastritis, the gastric mucous membrane
becomes edematous and hyperemic (congested with fluid and blood) and undergoes
superficial erosion (Fig. 37-1). It secretes a scanty amount of gastric juice,
containing very little acid but much mucus. Superficial ulceration may occur
and can lead to hemorrhage.
Clinical Manifestations
The patient with acute gastritis may have
abdominal discomfort, headache, lassitude, nausea, anorexia, vomiting, and
hiccupping. Some patients, however, have no symptoms. The patient with chronic
gastritis may complain of anorexia, heartburn after eating, belching, a sour
taste in the mouth, or nausea and vomiting. Patients with chronic gastritis
from vitamin deficiency usually have evidence of malabsorption of vitamin B12
caused by antibodies against intrinsic factor
Assessment and Diagnostic Findings
Gastritis is sometimes associated with
achlorhydria or hypochlorhydria (absence or low levels of hydrochloric acid
[HCl]) or with hyperchlorhydria (high levels of HCl). Diagnosis can be
determined by endoscopy, upper GI radiographic studies, and histologic
examination of a tissue specimen obtained by biopsy. In addition to biopsy,
other diagnostic measures for detecting H. pylori include serologic testing for
antibodies against the H. pylori antigen, a 1-minute ultrarapid urease test,
and a breath test.
Medical Management
The gastric mucosa is capable of repairing
itself after a bout of gastritis. As a rule, the patient recovers in about 1
day, although the appetite may be diminished for an additional 2 or 3 days.
Acute gastritis is also managed by instructing the patient to refrain from
alcohol and food until symptoms subside. After the patient can take nourishment
by mouth, a nonirritating diet is recommended. If the symptoms persist, fluids
may need to be administered parenterally. If bleeding is present, management is
similar to the procedures used for upper GI tract hemorrhage.
If gastritis is caused by ingestion of strong
acids or alkalis, treatment consists of diluting and neutralizing the offending
agent. To neutralize acids, common antacids (eg, aluminum hydroxide) are used;
to neutralize an alkali, diluted lemon juice or diluted vinegar is used. If
corrosion is extensive or severe, emetics and lavage are avoided because of the
danger of perforation and damage to the esophagus.Therapy is supportive and may
include nasogastric (NG) intubation, analgesic agents and sedatives, antacids,
and intravenous (IV) fluids. Fiberoptic endoscopy may be necessary. In extreme
cases, emergency surgery may be required to remove gangrenous or perforated
tissue. Gastrojejunostomy or gastric resection may be necessary to treat
pyloric obstruction, a narrowing of the pyloric orifice.
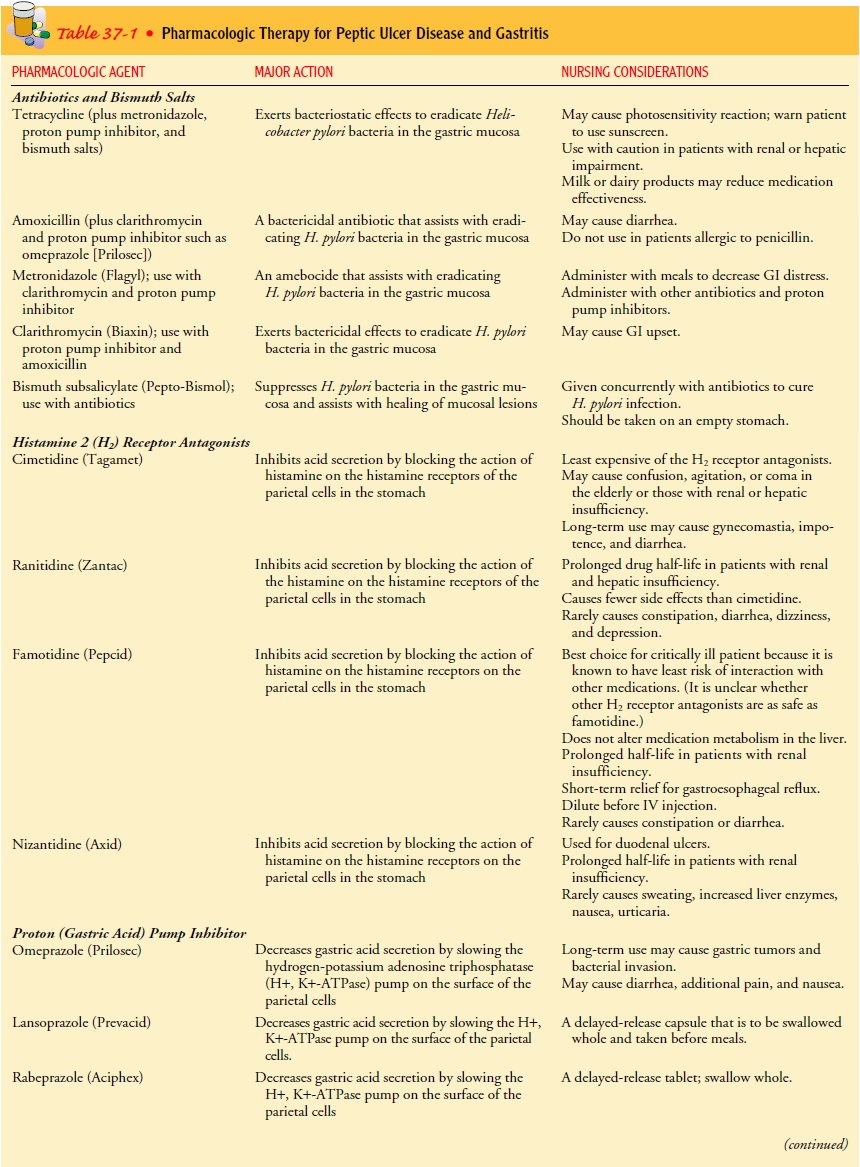
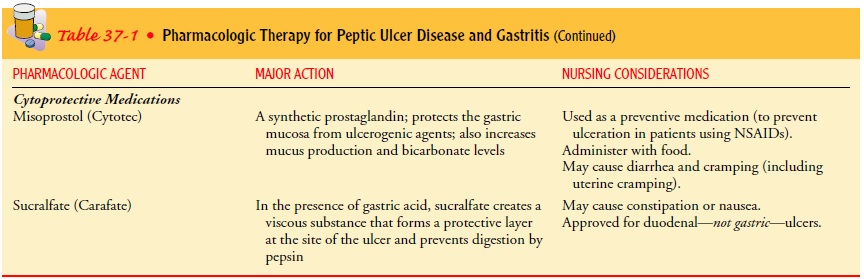
Chronic gastritis is managed by modifying the
patient’s diet, promoting rest, reducing stress, and initiating
pharmacotherapy.H. pylori may be treated with antibiotics (eg, tetracycline or
amoxicillin, combined with clarithromycin) and a proton pump inhibitor (eg,
lansoprazole [Prevacid]), and possibly bismuth salts (Pepto-Bismol) (Table
37-1). Research is being conducted to develop a vaccine against H. pylori
(Alsahli et al., 2001)
Related Topics