Chapter: Medical Surgical Nursing: Gastrointestinal Intubation and Special Nutritional Modalities
Nursing Process: The Patient Receiving Parenteral Nutrition
NURSING
PROCESS: THE PATIENT RECEIVING PARENTERAL NUTRITION
Assessment
The
nurse assists in identifying patients who may be candidates for PN. Indicators
include any significant weight loss (10% or more of usual weight), a decrease
in oral food intake for more than 1 week, any significant sign of protein loss
(serum albumin levels less than 3.2 g/dL [32 g/L], muscle wasting, decreased
tis-sue healing, or abnormal urea nitrogen excretion), and persistent vomiting
and diarrhea. The nurse carefully monitors the patient’s hydration, electrolyte
levels, and calorie intake.
Diagnosis
NURSING DIAGNOSES
Based
on the assessment data, the major nursing diagnoses may include the following:
•
Imbalanced nutrition, less than body requirements,
related to inadequate oral intake of nutrients
•
Risk for infection related to contamination of the
central catheter site or infusion line
•
Risk for excess or deficient fluid volume related
to altered infusion rate
•
Risk for immobility related to fear that the
catheter will be-come dislodged or occluded
•
Risk for ineffective therapeutic regimen management
re-lated to knowledge deficit about home PN therapy
COLLABORATIVE PROBLEMS/ POTENTIAL COMPLICATIONS
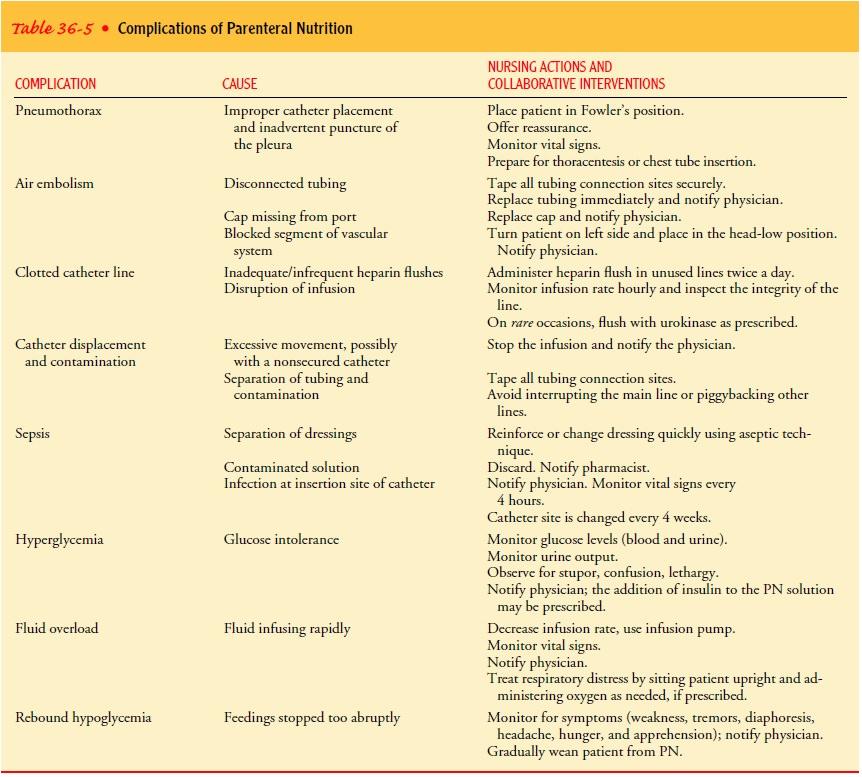
The most common complications are pneumothorax, air em-bolism, a clotted or displaced catheter, sepsis, hyperglycemia, rebound hypoglycemia, and fluid overload. These problems and the associated collaborative interventions are described in Table 36-5.
Planning and Goals
The
major goals for the patient may include optimal level of nu-trition, absence of
infection, adequate fluid volume, optimal level of activity (within individual
limitations), knowledge of and skill in self-care, and prevention of
complications.
Nursing Interventions
MAINTAINING OPTIMAL NUTRITION
A continuous,
uniform infusion of PN solution over a 24-hour period is desired. In some
cases, however (eg, home care patients), cyclic PN may be appropriate. With
cyclic PN, there is a set time during a 24-hour period when PN is infused and a
set time when it is not. The time periods for infusion are sufficient to meet
the patient’s nutritional and pharmacologic needs. Ideally, cyclic PN is
infused over an 8- to 10-hour period during the night.
The
patient is weighed daily (this may be decreased to two or three times per
week), at the same time of the day under the same conditions for accurate
comparison. Under the PN regimen (without additional energy expenditure), a
satisfactory weight gain is usually achieved. It is important to keep accurate
intake and output records and calculations of fluid balance. A calorie count is
kept of any oral nutrients. Trace elements (copper, zinc, chromium, manganese,
and selenium) are included in PN solu-tions and are individualized for each
patient. The PN solutions are prescribed daily by the physician on a standard
PN order form based on laboratory values and patient tolerance.
PREVENTING INFECTION
The
high glucose content of PN solutions makes these solutions ideal culture media
for bacterial and fungal growth, and CVADs provide a port of entry. Candida albicans is the most common
in-fectious organism. Other infectious organisms include Staphylo-coccus aureus, Staphylococcus epidermidis, and Klebsiella pneumoniae. Meticulous
technique is essential to prevent infection.
The
primary sources of microorganisms for catheter-related infections are the skin
and the catheter hub. The catheter site is covered with an occlusive gauze
dressing that is usually changed every other day. Alternatively, a transparent
dressing may be used and changed weekly. The Centers for Disease Control and
Prevention recommends changing dressings for CVADs only if they are damp,
bloody, loose, or soiled. The dressings are changed using sterile technique.
The nurse and patient wear masks dur-ing dressing changes to reduce the
possibility of airborne contam-ination. The area is checked for leakage, bloody
drainage, a kinked catheter, and skin reactions such as inflammation, redness,
swelling, tenderness, or purulent drainage. The nurse puts on sterile gloves
and cleanses the area with tincture of 2% iodine or a chlorhexidine solution on
a sterile gauze. The site is cleaned thoroughly using circular motion from the
site outward approx-imately 3 inches. This is repeated two times. This is
followed with the same cleaning procedure using 2 × 2-inch gauze pads
moist-ened with sterile water or saline solution (alcohol is used to re-move
iodine). Next the catheter lumens are cleaned from the exit site to the distal
end with an alcohol wipe. The insertion site is covered with an occlusive gauze
pad or transparent dressing cen-tered over the area.
The
advantages of using a transparent dressing over the gauze pad are that it
allows frequent examination of the catheter site without changing the dressing,
it adheres well, and it is more comfortable for the patient. When an extension
set is used with a central catheter, it is considered an extension of the
catheter it-self. It is not routinely changed with dressing or tubing changes.
The connection (hub) between the catheter and extension tubing is secured with
adhesive tape to prevent separation and exposure to air. Main-line IV tubing
and filters are changed every 72 to 96 hours, and all connections are taped
securely to avoid breaks in the integrity of the system. The dressing and
tubing are labeled with the date, time of insertion, time of dressing change,
and ini-tials of the person who carried out the procedure; this informa-tion is
also documented in the medical record.
The
catheter is another major source of colonization and in-fection.
Antiseptic-impregnated central venous catheters are new devices that reduce
catheter colonization by coating of the catheter surfaces with antimicrobial
agents. Two types are avail-able, one coated with chlorhexidine/silver sulfadiazine
and the other with minocycline/rifampin (Hanna et al., 2001).
MAINTAINING FLUID BALANCE
An infusion pump is necessary for PN to maintain an accurate rate of administration. A designated rate is set in milliliters per hour, and the rate checked every 30 to 60 minutes. An alarm signals a problem. The infusion rate should not be increased or decreased to compensate for fluids that have infused too quickly or too slowly. If the solution runs out, 10% dextrose and water is infused until the next PN solution is available from the pharmacy.
If the
rate is too rapid, hyperosmolar diuresis occurs (excess sugar will be
excreted), which, if severe enough, can cause in-tractable seizures, coma, and
death. Symptoms of rapid hyper-tonic fluid intake include headache, nausea,
fever, chills, and increasing lethargy.
If the
flow rate is too slow, the patient does not get the maxi-mal benefit of
calories and nitrogen. Intake and output are recorded every 8 hours so that
fluid imbalance can be readily de-tected. The patient is weighed two or three
times a week; in ideal situations, the patient will show neither weight loss
nor signifi-cant weight gain. The nurse assesses for signs of dehydration (eg,
thirst, decreased skin turgor, decreased central venous pressure) and reports
these findings to the physician immediately. It is essential to monitor blood
glucose levels, because hyperglycemia can cause diuresis and excessive fluid
loss.
ENCOURAGING ACTIVITY
Activities
and ambulation are encouraged when the patient is physically capable. With a
catheter in the subclavian vein, the pa-tient is free to move the extremities
and should be encouraged to maintain good muscle tone. If applicable, the
teaching and exer-cise program initiated in the occupational and physical
therapy departments should be reinforced.
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care
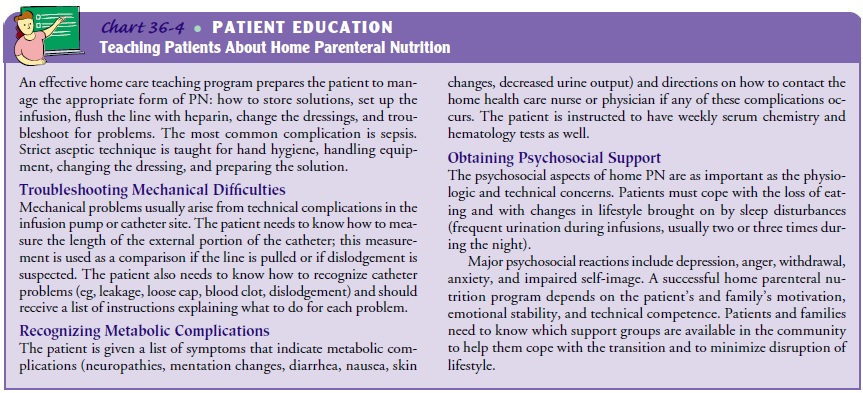
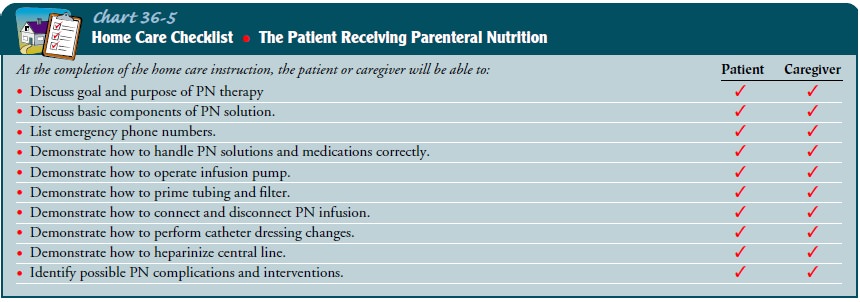
Successful home PN requires teaching the patient and family spe-cialized skills using an intensive training program and follow-up supervision
in the home. This is accomplished through a team ef-fort. The financial costs
of such programs, although high, are less than those incurred in a hospital.
Initiation of a home program may be the only way the patient can be discharged
from the hospital.
Ideal
candidates for home PN are those patients who have a reasonable life expectancy
after return home, have only a limited number of medical illnesses other than
the one that has resulted in the need for PN, and are highly motivated and
fairly self-sufficient. In addition, ability to learn, availability of family
in-terest and support, adequate finances, and the physical plan of the home are
factors that must be assessed when the decision for home PN is made.
Home
health care agencies sponsoring home PN programs have developed teaching
brochures for every aspect of the treat-ment, including catheter and dressing
care, use of an infusion pump, administration of fat emulsions, and
instillation of hepa-rin flushes. Teaching begins in the hospital and continues
in the home or in an ambulatory infusion center.
Continuing Care
The
home care nurse should be aware that the average patient needs about 2 weeks of
instruction and reinforcement. For more information about home patient
education, see Charts 36-4 and 36-5.
Evaluation
EXPECTED PATIENT OUTCOMES
Expected
patient outcomes may include the following:
1) Attains or maintains
nutritional balance
2) Is free of infection at
the catheter site
a.
Is afebrile
b.
Has no purulent drainage from the catheter
insertion site
c.
Has intact IV line
3) Is hydrated, as
evidenced by good skin turgor
4) Achieves an optimal
level of activity, within limitations
5) Demonstrates skill in managing PN regimen
6) Prevents complications
a.
Maintains proper catheter and equipment function
b.
Has no symptoms of sepsis
c.
Maintains metabolic balance within normal limits
d.
Shows improved and stabilized nutritional status
Related Topics