Chapter: Medical Surgical Nursing: Gastrointestinal Intubation and Special Nutritional Modalities
Nursing Process: The Patient Receiving a Tube Feeding
NURSING
PROCESS:THE PATIENT RECEIVING A TUBE FEEDING
Assessment
A
preliminary assessment of the patient who requires a tube feed-ing includes
several considerations, as well as the family’s need for information:
•
What is the patient’s nutritional status, as judged
by current physical appearance, dietary history, and recent weight loss?
•
Are there any existing chronic illnesses or factors
that will increase metabolic demands on the body (eg, surgical stress, fever)?
•
What is the patient’s hydration status? What are
the elec-trolyte levels?
•
Is the patient’s digestive tract functioning?
•
Are the kidneys functioning normally?
•
Are fluid requirements (ie, 30 to 40 mL/kg body
weight) being met?
•
What medications and other therapies is the patient
re-ceiving that may affect digestive intake and function of the digestive
system?
•
Does the dietary prescription fulfill the patient’s
needs?
In
addition, a more elaborate assessment is performed for pa-tients who require
extensive nutritional therapy. A team that in-cludes the nurse, physician, and
dietitian conducts this assessment. In addition to the history and physical
examination (which in-cludes anthropometric measurements), nutritional
assessment consists of recording any weight change; determining albumin,
prealbumin, and transferrin levels and total lymphocyte count; testing for the
delayed hypersensitivity reaction; and evaluating muscle function.
Diagnosis
NURSING DIAGNOSES
Based
on the assessment data, the major nursing diagnoses may include the following:
•
Imbalanced nutrition, less than body requirements,
related to inadequate intake of nutrients
•
Risk for diarrhea related to the dumping syndrome
or to tube feeding intolerance
•
Risk for ineffective airway clearance related to
aspiration of tube feeding
•
Risk for deficient fluid volume related to
hypertonic dehy-dration
•
Risk for ineffective coping related to discomfort
imposed by the presence of the NG or nasoenteric tube
•
Risk for ineffective therapeutic regimen management
•
Deficient knowledge about home tube feeding regimen
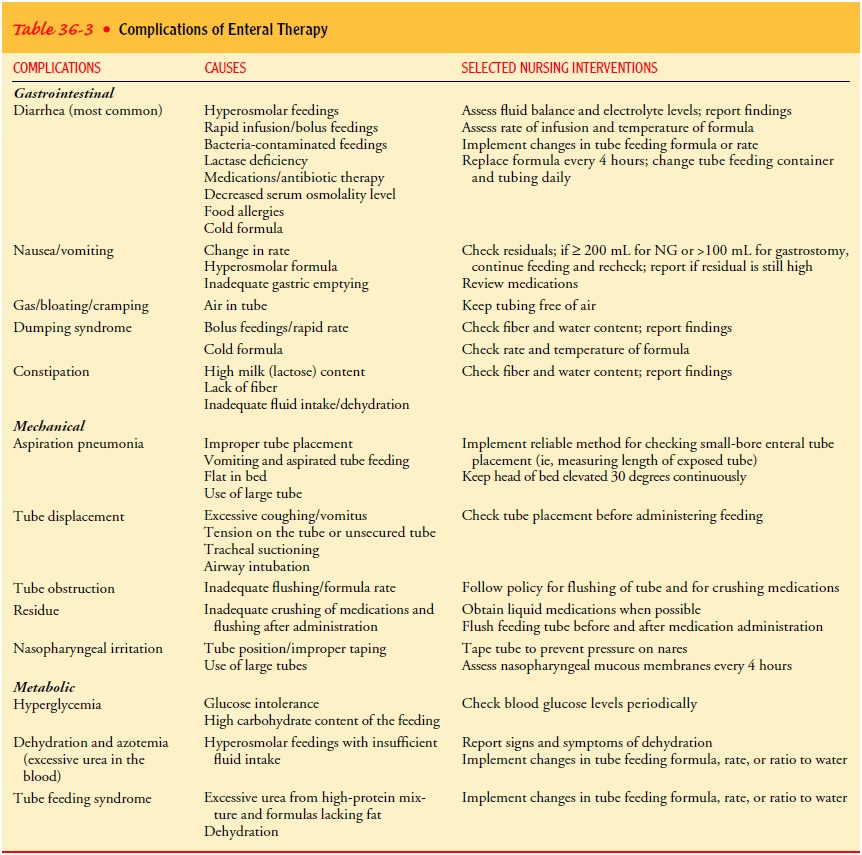
COLLABORATIVE PROBLEMS/POTENTIAL COMPLICATIONS
Complications
of NG and nasoenteric tube feeding therapy are classified into three types—GI,
mechanical, and metabolic. Table 36-3 lists complications, possible causes, and
appropriate interventions.
Planning and Goals
The
major goals for the patient may include nutritional balance, normal bowel
elimination pattern, reduced risk of aspiration, ad-equate hydration,
individual coping, knowledge and skill in self-care, and prevention of
complications.
Nursing Interventions
MAINTAINING FEEDING EQUIPMENT AND NUTRITIONAL BALANCE
The
temperature and volume of the feeding, the flow rate, and the total fluid
intake are important factors to be considered when tube feedings are
administered. The schedule of tube feedings, in-cluding the correct quantity
and frequency, is maintained. The nurse must carefully monitor the drip rate
and avoid administer-ing fluids too rapidly.
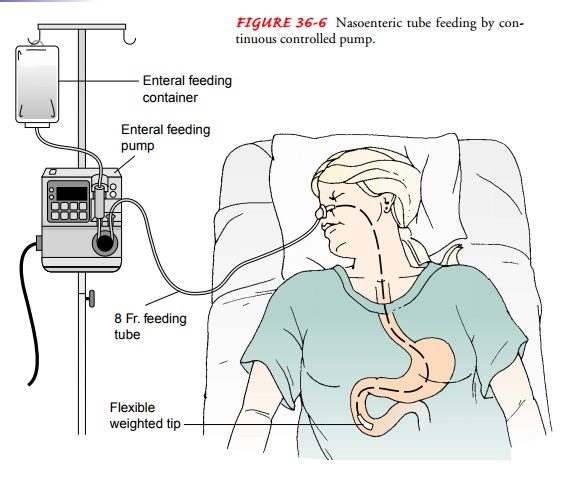
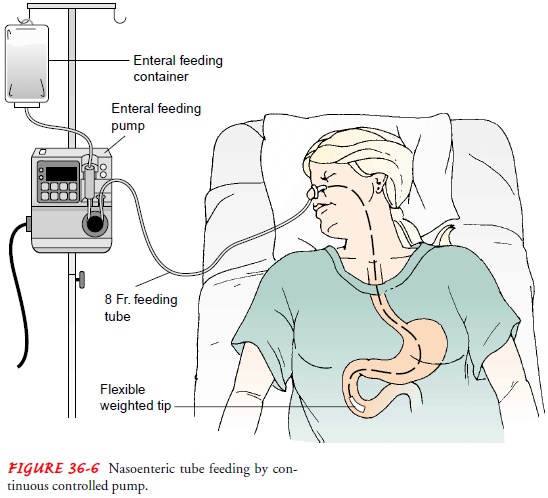
Feedings
are administered by gravity (drip), bolus, or continu-ous controlled pump
(mL/hour or drops/hour). Gravity feedings are placed above the level of the
stomach, with the speed of ad-ministration determined by gravity. Bolus feedings are given in large
volumes (300 to 400 mL every 4 to 6 hours). Continuous feeding is the preferred
method; delivery of the feeding in small amounts over long periods reduces the
incidence of aspiration, distention, nausea, vomiting, and diarrhea. Continuous
admin-istration rates of about 100 to 150 mL/hour (2400 to 3600 calo-ries/day)
are effective in inducing positive nitrogen balance and progressive weight gain
without producing abdominal cramps and diarrhea. If the feeding is
intermittent, 200 to 350 mL is given in 10 to 15 minutes. Enteral pumps are
mechanical devices that control the delivery rate of feeding formula (Fig.
36-6). Pumps allow for a constant flow rate and can infuse a viscous for-mula
through a small-diameter feeding tube. These pumps are relatively heavy and
must be attached to an IV pole. For home use, there are portable lightweight
enteral pumps available that weigh about 4 pounds and are easy to handle. An
enteral pump is available with an automatic water flush system. In addition to
administering the feeding formula, these pumps provide hourly water flushes
that are designed to prevent clogged feeding tubes (Petnicki, 1998).
Residual
gastric content is measured before each intermittent feeding and every 4 to 8
hours during continuous feedings. (This aspirated fluid is readministered to
the patient.) The research findings of McClave et al. (1992) indicated that, if
the amount of aspirated gastric content is greater than or equal to 200 mL for
NG tubes or if residual volumes are greater than or equal to 100 mL for
gastrostomy tubes, tube feeding intolerance should be con-sidered. Tube
feedings may be continued with close monitoring of gastric residual volume,
radiographic studies, and the patient’s physical status. If excessive residual
volumes occur twice, the nurse notifies the physician.
Maintaining
tube function is an ongoing responsibility of the nurse, patient, or primary
caregiver. To ensure patency and to de-crease the chance of bacterial growth,
crusting, or occlusion of the tube, 20 to 30 mL of water is administered in
each of the follow-ing instances:
•
Before and after each dose of medication and each
tube feeding
•
After checking for gastric residuals and gastric pH
•
Every 4 to 6 hours with continuous feedings
•
If the tube feeding is discontinued for any reason
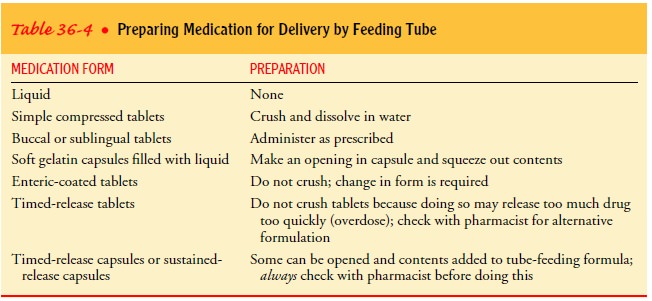
PROVIDING MEDICATIONS BY TUBE
When
different types of medications are administered, each type is given separately,
using a bolus method that is compatible with the medication’s preparation
(Table 36-4). The tube is flushed with 20 to 30 mL of water after each dose. If
a liquid form of a medication is not available and the medication can be
crushed, it must first be reduced to a fine powder or the tube will become
clogged. Devices are available (eg, Handicrush Irrigation Syringe by Nestle)
that crush and dissolve tablets with water (Fig. 36-7). Medications are not
mixed with each other or with the feeding formula. When small-bore feeding
tubes for continuous infusion are irrigated after medication administration, a
30-mL or larger syringe is used, because the pressure generated by smaller
syringes could rupture the tube.
MAINTAINING FEEDING REGIMENS AND DELIVERY SYSTEMS
Tube
feeding formula is delivered to patients by either an open or a closed system.
The open system comes in cans or as a powder and may be mixed with water. The feeding
container (which is hung on a pole) and the tubing used with the open system
are changed—usually every 24 to 72 hours. To avoid bacterial cont-amination,
the amount of feeding formula in the bag should never exceed what is expected
to be infused in 4 hours.
Closed
delivery systems use a prefilled, sterile container that is spiked with enteral
tubing. The bag holding the feeding formula for the closed system can be hung
safely for 24 to 48 hours.
The
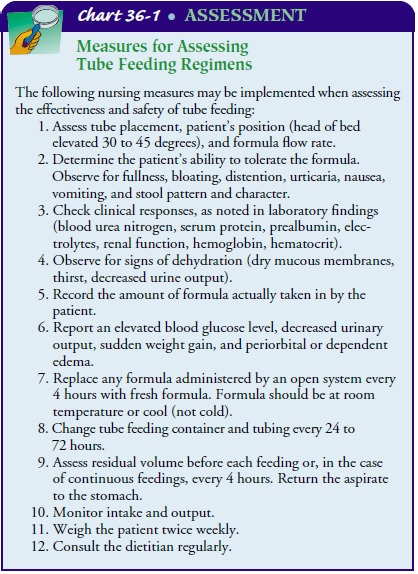
tube-feeding regimen must be assessed frequently to eval-uate its effectiveness
and avoid complications (Chart 36-1).
MAINTAINING NORMAL BOWEL ELIMINATION PATTERN
Patients receiving NG or nasoenteric tube feedings commonly have diarrhea (watery stools occurring three or more times in hours). Pasty, unformed stool is expected with enteral ther-apy, because many formulas have little or no residue. The dump-ing syndrome also leads to diarrhea, but to confirm dumping syndrome as the cause of diarrhea other possible causes must be ruled out, among them the following:
•
Zinc deficiency—Adding 15 mg of zinc to the tube
feeding every 24 hours is recommended to maintain a normal serum level of 50 to
150 fg/dL (7.65 to 22.95 fmol/L)
•
Contaminated formula
•
Malnutrition—A decrease in the intestinal
absorptive area resulting from malnutrition can cause diarrhea
•
Medication therapy—Antibiotics, such as clindamycin
(Cleocin) and lincomycin (Lincocin); antiarrhythmics, such as quinidine and
propranolol (Inderal); and aminophylline, theophylline, and digitalis have been
found to increase the frequency of diarrhea in some patients
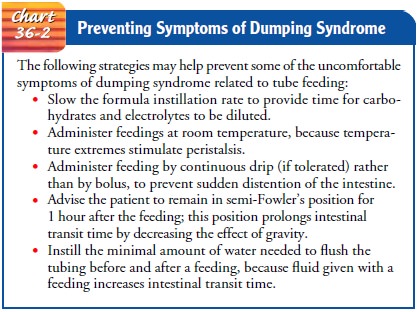
The
dumping syndrome results from rapid distention of the jejunum when hypertonic
solutions are administered quickly (over 10 to 20 minutes). Foods high in
carbohydrates and elec-trolytes draw extracellular fluid from the vascular
system into the jejunum so that dilution and absorption can occur. Measures for
managing the GI symptoms (diarrhea, nausea) associated with the dumping
syndrome are presented in Chart 36-2.
REDUCING THE RISK OF ASPIRATION
Aspiration pneumonia occurs when stomach contents or enteral feedings are regurgitated and aspirated, or when an NG tube is improperly positioned and feedings are instilled into the pharynx or the trachea. Nasoenteric tubes, especially those that provide for gastric and esophageal or duodenal decompression, have helped decrease the frequency of regurgitation and aspiration.
To
prevent aspiration, the nurse must establish the correct tube feeding placement
before every feeding, each time medica-tions are administered, and once every
shift if the tube feeding is continuous. Feedings and medications should always
be given with the patient in the proper position to prevent regurgitation. To reduce
the risk of reflux and pulmonary aspiration, the semi-Fowler’s position is
necessary for an NG feeding, with the pa-tient’s head elevated at least 30 to
45 degrees. This position is maintained at least 1 hour after completion of an
intermittent tube feeding and is maintained at all times for patients receiving
continuous tube feedings. Another prevention strategy is to mon-itor residual
volumes (Edwards & Metheny, 2000).
If
aspiration is suspected, the feeding is stopped immediately, the pharynx and trachea
are suctioned, and the patient is placed on the right side with the head of the
bed down. The physician is notified immediately.
MAINTAINING ADEQUATE HYDRATION
The nurse carefully monitors hydration because, in many cases, the patient cannot communicate the need for water. Water (at least 2 L/day) is given every 4 to 6 hours and after feedings to pre-vent hypertonic dehydration. At the beginning of administration, the feeding is diluted to at least half-strength and not more than 50 to 100 mL is given at a time, or 40 to 60 mL/hour is given in continuous drip administration. This gradual administration helps the patient to develop tolerance, especially for hyperosmo-lar solutions. Key nursing interventions include observing for signs of dehydration (dry mucous membranes, thirst, decreased urine output); administering water routinely and as needed; and monitoring intake, output, and fluid balance (24-hour intake ver-sus output).
PROMOTING COPING ABILITY
The psychosocial goal of nursing care is to support and encour-age the patient to accept physical changes and to convey hope that daily progressive improvement is possible. If the patient is having difficulty adjusting to the treatment, the nurse intervenes by encouraging self-care (eg, recording daily weight and intake and output), within the parameters of the patient’s activity level. In addition, the nurse reinforces an optimistic approach by iden-tifying signs and symptoms that indicate progress (daily weight gain, electrolyte balance, absence of nausea and diarrhea).
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care
Patients
who require long-term tube feedings in the home care setting have conditions
such as obstruction of the upper GI tract, malabsorption syndrome, surgery of
the GI tract or of the head or neck region, or decreased level of
consciousness. For a patient to be considered for tube feeding at home, the following
criteria must be met: The patient must be medically stable and must have
successfully completed a tube feeding trial (tolerated 70% of feeding). In
addition, the patient must be capable of self-care or have a caregiver who is
willing to assume the responsibility, and the patient or caregiver must have
access to supplies and interest in learning how to administer tube feedings at
home.
Preparation
of the patient for home administration of enteral feedings begins while the
patient is still hospitalized. Ideally, the nurse teaches while administering
the feedings so that the patient can observe the mechanics of the procedure,
participate in the procedure, ask questions, and express any concerns. Before
dis-charge, the nurse provides information about the equipment needed, formula
purchase and storage, and administration of the feedings (frequency, quantity,
rate of instillation).
Family
members who will be active in the patient’s home care are encouraged to
participate in all teaching sessions. Available printed information about the
equipment, the formula, and the procedure is reviewed. The nurse encourages the
patient and care-giver to learn to use the equipment with the supervision of
the nurse. Arrangements are made for the caregiver to obtain the equipment and
formula and have it ready for use before the pa-tient’s discharge.
Continuing Care
Referral
to a home care agency is important so that a nurse can arrange to be present to
supervise and provide support during the first feeding at home. Further visits
will depend on the skill and comfort of the patient or caregiver in
administering the feedings.
During
all visits, the nurse monitors the patient’s physical status (weight, vital
signs, activity level) and the ability of the patient and family to administer
the tube feedings correctly. In addition, the nurse assesses for any
complications (dumping syndrome, nausea or vomiting, weight loss, lethargy,
confusion, excessive thirst). The patient or caregiver is encouraged to keep a
diary to record times and amounts of feedings and any symptoms that occur. The
nurse reviews the diary with the patient and caregiver during home visits.
Evaluation
EXPECTED PATIENT OUTCOMES
Expected
patient outcomes may include the following:
1) Attains or maintains
nutritional balance
a.
Has a positive nitrogen balance
b. Maintains laboratory
values within normal limits (ie, blood urea nitrogen, hemoglobin, hematocrit,
prealbu-min, serum protein)
c.
Attains or maintains hydration of body tissue
d.
Attains or maintains desired body weight
2) Is free of episodes of
diarrhea
a.
Has fewer than three watery stools a day
b.
Does not have a bowel movement after a bolus
feeding
c.
States that there is no intestinal cramping
d.
Has normal bowel sounds
3) Avoids aspiration
a.
Lungs are clear to auscultation
b.
Exhibits normal heart rate and respirations
4) Attains or maintains
hydration of body tissue
a.
Has a balanced intake and output every 24 hours
b.
Does not have dry skin or dry mucous membranes
5) Copes effectively with
tube feeding regimen
6) Demonstrates skill in
managing tube feeding regimen
7) Experiences no
complications
a.
Has no GI disturbances
b.
Tube remains intact and patent for duration of
therapy
c.
Maintains metabolic balance within normal limits
Related Topics