Chapter: Medical Surgical Nursing: Gastrointestinal Intubation and Special Nutritional Modalities
Gastrointestinal Intubation
Gastrointestinal Intubation
GI
intubation is the insertion of a rubber or plastic tube into the stomach, the duodenum (first section of the small
intestine), or the intestine. The tube may be inserted through the mouth, the
nose, or the abdominal wall. The tubes can be short, medium, or long, depending
on their intended use; nasogastric (NG)
tubes are short, nasoduodenal tubes
are of medium length, and naso-enteric tubes are long. GI intubation may be
performed for the following reasons:
•
To decompress the stomach and remove gas and fluid
•
To lavage the stomach and remove ingested toxins
•
To diagnose disorders of GI motility and other
disorders
•
To administer medications and feedings
•
To treat an obstruction
•
To compress a bleeding site
•
To aspirate gastric contents for analysis
A
variety of tubes are used for decompression, aspiration, and lavage. The
Sengstaken-Blakemore tube is a type of NG tube used to treat bleeding
esophageal varices. Orogastric tubes are large-bore tubes with wide proximal
outlets for removal of particles of ingested substances (eg, pills); they are
primarily used in emergency departments. Various other tubes are used to
ad-minister feedings and medications. The tubes are made of various materials
(rubber, polyurethane, silicone), and they vary in length (90 cm to 3 m [3 to
10 ft]), in size (6 to 18 French [Fr]), in pur-pose, and in placement in the GI
tract (stomach, duodenum, je-junum) (Table 36-1). Any solution administered
through a tube is either poured through a syringe or delivered by a drip
mechanism regulated by gravity or by an electric pump. Aspiration (suctioning) to remove gas and fluids is accomplished
with the use of a syringe, an electric suction machine, or a wall suction
outlet.
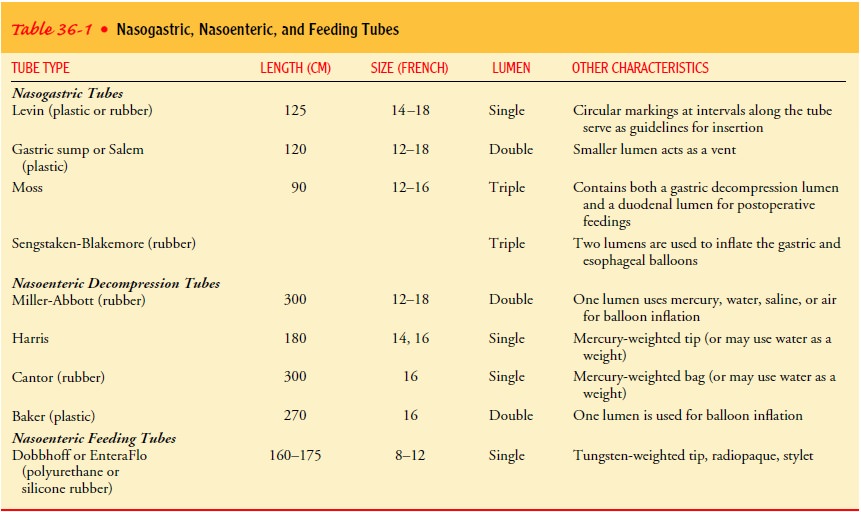
SHORT TUBES
An NG
tube or short tube is introduced through the nose into the stomach, often
before or during esophageal or stomach surgery. Commonly used short tubes
include the Levin tube and the gas-tric sump tube. Short tubes are used in
adults primarily to remove fluid and gas from the upper GI tract or to obtain a
specimen of gastric contents for laboratory studies. They are occasionally used
for the short-term (3 to 4 weeks) administration of medications or feedings.
Levin Tube
The Levin tube has a single lumen (the hollow part of the tube), ranges from 14 to 18 Fr in size, and is made of plastic or rubber with openings near its tip. It is 125 cm (50 in) long. Circular markings at specific points on the tube serve as guides for inser-tion. A marking is made on the tube to indicate the midpoint. The tube is advanced cautiously until this marking reaches the patient’s nostril, suggesting that the tube is in the stomach. Place-ment is checked by observing the characteristics of the aspirate and by testing the pH (which varies according to the source of the aspirate). Seeing the tube on an x-ray study is the only sure way to verify its location. The Levin tube is connected to low in-termittent suction (30 to 40 mm Hg). Intermittent suction is used to avoid erosion or tearing of the stomach lining, which can result from constant adherence of the tube’s lumen to the mu-cosal lining of the stomach.
Gastric Sump
The
gastric sump (Salem) tube is a radiopaque, clear plastic, double-lumen NG tube
used to decompress the stomach and keep it empty. It is 120 cm (48 in) long and
is passed into the stomach in the same way as the Levin tube. The inner,
smaller tube vents the larger suction-drainage tube to the atmosphere by means
of an opening at the distal end of the tube. The sump tube can pro-tect gastric
suture lines because, when used properly, it maintains the force of suction at
the drainage openings, or outlets, at less than 25 mm Hg, the level of
capillary fragility. The small vent tube (known as the blue pigtail) controls
this action. These tubes are connected to low continuous suction. The suction
lumen is irrigated as prescribed to maintain patency.
To
prevent reflux of gastric contents through the vent lumen (blue pigtail), the
vent lumen is kept above the patient’s waist; otherwise it will act as a
siphon. A one-way antireflux valve
seated in the blue pigtail prevents the reflux of gastric contents out the vent
lumen (Fig. 36-1). The valve is removed after irri-gation of the suction lumen,
and 20 mL of air is injected to reestablish a buffer of air between the gastric
contents and the valve.
MEDIUM TUBES
Medium-length
nasoenteric tubes are used for feeding. Feeding tubes placed in the duodenum
are 160 cm (60 in) long; feeding tubes placed in the jejunum (portion of the small intestine adja-cent to the duodenum)
are 175 cm (66 in) long. They can be in-serted at the time of surgery or before
surgery, by interventional radiologists assisted by fluoroscopy or at the
bedside. If the tube is inserted at the bedside, placement is verified by
radiography.
After
insertion, the tip of the tube will initially be in the stomach; it usually
takes 24 hours for the tube to pass through the stom-ach and into the
intestines.
Polyurethane
or silicone rubber feeding tubes have narrow di-ameters (6 to 12 Fr) and
tungsten tips (rather than mercury-filled bags); some have a water-activated
lubricant that makes it easier to insert the tube. The tubing may kink when a
stylet is not used, particularly if the patient is uncooperative or unable to
swallow. Feeding tubes with a stylet are inserted with caution in patients who
are predisposed to esophageal puncture, such as elderly and frail patients with
thin tissues. These tubes are ad-vanced in the same way as an NG tube; that is,
with the patient in Fowler’s position. If this is not feasible, the patient is
placed on the right side.
LONG TUBES
A long nasoenteric tube is introduced through the nose and passed through the esophagus and stomach into the intestinal tract. It is used to aspirate intestinal contents so that gas and fluid do not distend the intestine; this is called decompression. Three major nasoenteric tubes used for aspiration and decompression are the Miller-Abbott tube, the Harris tube, and the Cantor tube. These tubes are used to relieve obstruction of the small in-testine. They are also used prophylactically; they may be inserted the night before GI surgery to prevent postoperative obstruction.
Because
peristalsis is either stopped or
slowed for 24 to 48 hours after surgery as a result of anesthesia and visceral
ma-nipulation, NG or nasoenteric suction is used to evacuate fluids and flatus
so that vomiting is prevented, tension is reduced along the incision line, and
obstruction is prevented. Usually, the tube remains in place until peristalsis
returns, as evidenced by the re-sumption of bowel sounds and the passage of
flatus.
Miller-Abbott Tube
The
Miller-Abbott tube is a double-lumen rubber tube that is 300 cm (10 ft) long
and 12, 14, 16, or 18 Fr in size. One lumen is used to introduce mercury, water,
or saline into the balloon at the end of the tube for weighting of the tube;
the other lumen is used for aspiration. Before the tube is inserted, the
balloon should be tested and its capacity measured; then it should be deflated
completely. The tube should be lubricated sparingly and chilled well (chilling
causes the tube to become stiff and facilitates its passage) before the tip is
inserted through the patient’s nose. Markings on the tube indicate the distance
it has been passed. Before removal, the bal-loon at the end of the lumen must
be completely deflated.
Harris Tube
The
Harris tube is a single-lumen (14 Fr), mercury-weighted tube of about 180 cm (6
ft). This tube has a metal tip that is lubricated and introduced through the
nose. The mercury-weighted bag follows. The weight of the mercury promotes the
passage of the bag by gravity. This tube is used solely for suction and irrigation. Usually, a Y-tube is
attached to the end of the Harris tube. The suction is applied to one side of
the Y and the other side is clamped, except when irrigation of the tube is
being performed.
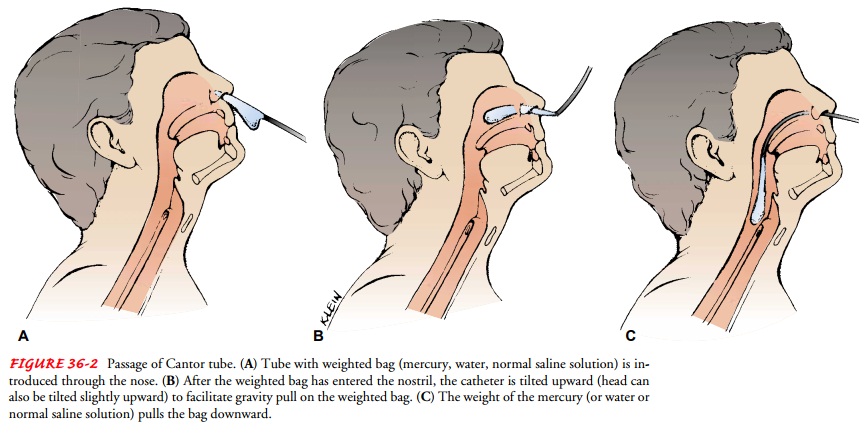
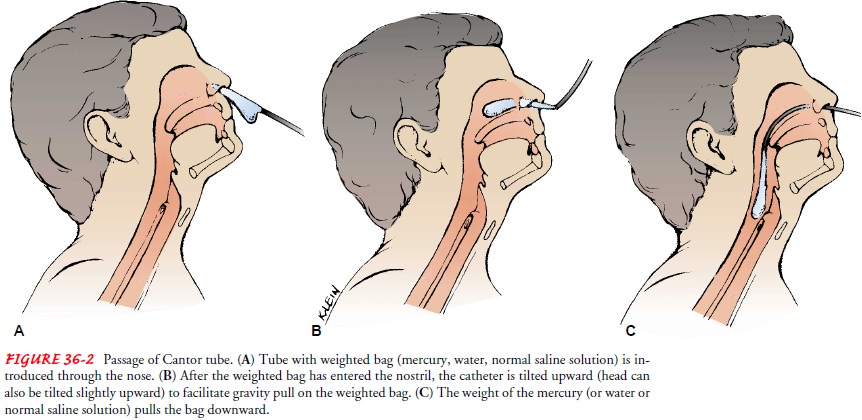
Cantor Tube
The
Cantor tube is 300 cm (10 ft) long and has a 16-Fr lumen. Its distinguishing
feature is that it is larger than the other long tubes. It has a 4- or 5-mL bag
at the extreme end of the rubber tubing; mercury, water or saline is introduced
into this bag to weight the tube. Before the tube is inserted, the bag is
wrapped around the tube. After the tube is lubricated, it is advanced through
the nose and into the esophagus (Fig. 36-2). The patient assumes a sitting
position and may be offered sips of water to facilitate pas-sage of the tube.
Fluoroscopy helps to verify that the tube has passed into the duodenum.
Related Topics