Chapter: Medical Surgical Nursing: Gastrointestinal Intubation and Special Nutritional Modalities
Nursing Process: The Patient With a Gastrostomy
NURSING
PROCESS: THE PATIENT WITH A GASTROSTOMY
Assessment
The
focus of the preoperative assessment is to determine the pa-tient’s ability
both to understand and to cope with the impend-ing surgical experience. The
nurse evaluates the patient’s ability to adjust to a change in body image and
to participate in self-care, along with the patient’s and the family’s
psychological status.
The
purpose of the operative procedure is explained so that the patient will have a
better understanding of the expected post-operative course. The patient needs
to know that the result of this surgery is to bypass the mouth and esophagus so
that liquid feedings can be administered directly into the stomach by means of
a rubber or plastic tube or a prosthesis. If the prosthesis is to be permanent,
the patient should be made aware of this. Psy-chologically, this is often
difficult for the patient to accept. If the procedure is being performed to
relieve discomfort, prolonged vomiting, debilitation, or an inability to eat,
the patient may find it more acceptable.
The
nurse evaluates the patient’s skin condition and deter-mines whether a delay in
healing may be anticipated because of a systemic disorder (eg, diabetes
mellitus, cancer).
In the
postoperative period, the patient’s fluid and nutritional needs are assessed to
ensure proper intake of food and fluids. The nurse inspects the tube for proper
maintenance and the incision for signs of infection. At the same time, the
nurse evaluates the patient’s response to the change in body image and the
patient’s understanding of the feeding methods. Interventions are identi-fied
to help the patient cope with the tube and learn self-care measures.
Diagnosis
NURSING DIAGNOSES
Based
on the assessment data, the major nursing diagnoses in the postoperative period
may include the following:
•
Imbalanced nutrition, less than body requirements,
related to enteral feeding problems
•
Risk for infection related to presence of wound and
tube
•
Risk for impaired skin integrity at tube site
•
Ineffective coping related to inability to eat
normally
•
Disturbed body image related to presence of tube
•
Risk for ineffective therapeutic regimen management
re-lated to knowledge deficit about home care and the feeding procedure
COLLABORATIVE PROBLEMS/POTENTIAL COMPLICATIONS
Potential
complications that may develop include the following:
•
Wound infection, cellulitis, and abdominal wall
abscess
•
GI bleeding
•
Premature removal of the tube
Planning and Goals
The
major goals for the patient may include attaining an optimal level of
nutrition, preventing infection, maintaining skin in-tegrity, enhancing coping,
adjusting to changes in body image, acquiring knowledge of and skill in
self-care, and preventing complications.
Nursing Interventions
MEETING NUTRITIONAL NEEDS
The
first fluid nourishment is administered soon after surgery and usually consists
of tap water and 10% glucose. At first, only 30 to 60 mL (1 to 2 oz) is given
at one time, but the amount is in-creased gradually. By the second day, 180 to
240 mL (6 to 8 oz) may be given at one time, provided it is tolerated and no
leakage of fluid occurs around the tube. Water and milk can be instilled after
24 hours for a permanent gastrostomy. High-calorie liquids are added gradually.
In some settings, during the early postoper-ative period the nurse aspirates
gastric secretions and reinstills them after adding enough feeding solution to
bring the volume to the desired total. By this method, gastric dilation is
avoided.
Blenderized
foods are added gradually to clear liquids until a full diet is achieved.
Powdered feedings that are easily liquefied are commercially available. The
patient who receives blenderized tube feedings typically is not forced to give
up usual dietary pat-terns, which may prove to be psychologically more
acceptable. In addition, near-normal bowel function is promoted because the
fiber and residue are similar to that of a normal diet. Intake of milk is
avoided in patients with lactase deficiency.
PROVIDING TUBE CARE AND PREVENTING INFECTION
A
small dressing can be applied over the tube outlet, and the gas-trostomy tube
can be held in place by a thin strip of adhesive tape that is first placed
around the tube and then firmly attached to the abdomen. The dressing protects
the skin around the incision from seepage of gastric acid and spillage of
feedings.
The
nurse verifies the tube’s placement, assesses residuals, and rotates the tube
or stabilizing disk once daily to prevent skin break-down. Some gastrostomy
tubes have balloons that are inflated with water to anchor the tube in the
stomach. The adequacy of balloon inflation is checked weekly by deflating the
balloon using a Luer-tip syringe.
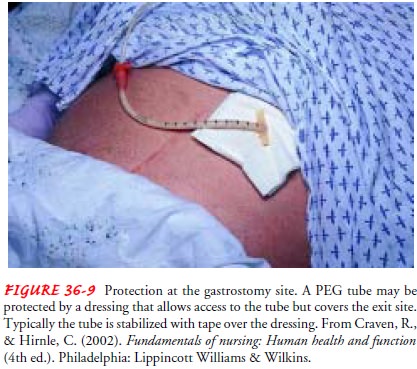
PROVIDING SKIN CARE
The
skin surrounding a gastrostomy requires special care because it may become
irritated from the enzymatic action of gastric juices that leak around the
tube. Left untreated, the skin becomes mac-erated, red, raw, and painful. The
nurse washes the area around the tube with soap and water daily, removes any
encrustation with saline solution, rinses the area well with water, and pats it
dry. Once the stoma heals and drainage ceases, a dressing is not required. A
long-term gastrostomy may require a special dressing or stabi-lization device
to protect the skin around the tube from gastric se-cretions and to help secure
the tube in place (Fig. 36-9).
Skin
at the exit site is evaluated daily for signs of breakdown, irritation,
excoriation, and the presence of drainage or gastric leakage. The nurse
encourages the patient and family members to participate in this inspection and
in hygiene activities. If skin problems do occur, an enterostomal therapist or
wound care spe-cialist can be of assistance.
ENHANCING BODY IMAGE
The
patient with a gastrostomy has experienced a major assault to body image.
Eating, a physiologic and social function, can no longer be taken for granted.
The patient is also aware that gas-trostomy as a therapeutic intervention is
performed only in the presence of a major, chronic, or perhaps terminal
illness.
Calm
discussion of the purposes and routines of gastrostomy feeding can help keep
the patient from feeling overwhelmed. Talk-ing with a person who has had a
gastrostomy can also help the pa-tient to accept the expected changes.
Adjusting to a change in body image takes time and requires family support and
acceptance. Eval-uating the existing family support system is necessary. One
family member may emerge as the primary support person.
MONITORING AND MANAGING POTENTIAL COMPLICATIONS
During
the postoperative course, the nurse monitors the patient for potential
complications. The most common complications are wound infection and other
wound problems, including cel-lulitis at the wound site and abscesses in the
abdominal wall. Be-cause many patients who receive tube feedings are
debilitated and have compromised nutritional status, any signs of infections
are promptly reported to the physician so that appropriate antibiotic therapy
can be instituted.
Bleeding
from the insertion site in the stomach may also occur. The nurse closely
monitors the patient’s vital signs and observes all drainage from the operative
site, vomitus, and stool for evi-dence of bleeding. Any signs of bleeding are
reported promptly.
Premature
removal of the tube, whether it is done inadver-tently by the patient or by the
caregiver, is another complication. If the tube is removed prematurely, the
skin is cleansed and a ster-ile dressing is applied; the nurse immediately
notifies the physi-cian. The tract will close within 4 to 6 hours if the tube
is not replaced promptly.
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care
The
patient who is to receive gastrostomy tube feedings in the home setting must be
capable of, and responsible for, adminis-tering the tube feedings or have a
caregiver who is able to do so. There must also be the physical, financial, and
social resources to maintain care.
The
nurse assesses the patient’s level of knowledge, interest in learning about the
tube feeding, and ability to understand and apply the information before
providing detailed instructions about how to prepare the formula and manage the
tube feeding. Written materials for patients and caregivers are designed to
out-line the care instructions. To facilitate self-care, the nurse en-courages
the patient to participate in the tube feedings during hospitalization and to
establish as normal a routine as possible.
Demonstration
of the tube feeding begins by showing the pa-tient how to check for residual
gastric contents before the feed-ing. The patient then learns how to check and
maintain the patency of the tube by administering room-temperature water
be-fore and after the feeding. This will establish patency before the feeding
and then clear the tube of food particles, which could de-compose if allowed to
remain in the tube. All feedings are given at room temperature or near body
temperature.
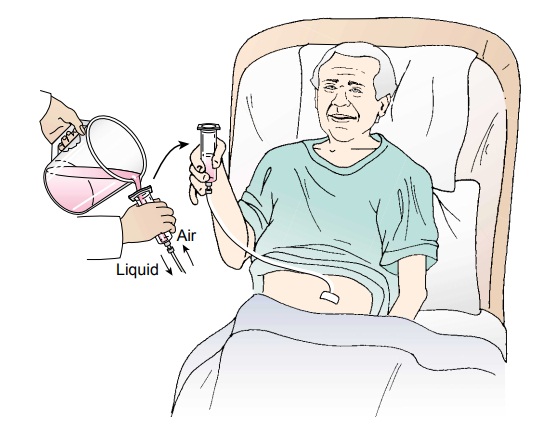
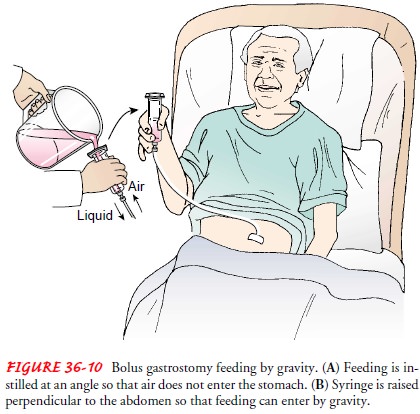
For a
bolus feeding, the nurse shows the patient how to intro-duce the liquid into
the catheter by using a funnel or the barrel of a syringe. The receptacle is
tilted to allow air to escape while the liquid is being instilled initially. As
the funnel or syringe fills with liquid, the feeding is allowed to flow into
the stomach by gravity by holding the barrel or syringe perpendicular to the
ab-domen (Fig. 36-10). Raising or lowering the receptacle to no higher than 45
cm (18 in) above the abdominal wall regulates the rate of flow.
A
bolus feeding of 300 to 500 mL usually is given for each meal and requires 10
to 15 minutes to complete. The amount is often determined by the patient’s
reaction. If the patient feels full, it may be desirable to give smaller
amounts more frequently.
The patient and caregiver must understand that keeping the head of the bed elevated for at least 1 hour after feeding facili-tates digestion and decreases the risk for aspiration. Any ob-struction requires that the feeding be stopped and the physician notified.
The
patient or caregiver is instructed to flush the tube with 30 mL of water after
each bolus or medication administration, and otherwise to flush the tube daily
to keep it patent. Adaptors are available that can be secured to the end of the
tube to create a “Y” site for ease of flushing or medication delivery. The
flushing equipment is cleaned with warm, soapy water and rinsed after each use.
The
patient and caregiver are made aware that the tube is marked at skin level to
provide the patient a baseline for later comparison. They are advised to
monitor the tube’s length and to notify the physician or home care nurse if the
segment of the tube outside the body becomes shorter or longer.
If the
patient is to use an intermittent or continuous-pressure feeding pump at home,
instruction in the use of the particular type of pump is essential. Most
feeding pumps have built-in alarms that signal when the bag is empty, when the
battery is low, or when an occlusion is present. The patient and caregiver need
to be aware of these alarms and how to troubleshoot the pump.
Continuing Care
Referral
to a home care agency is important to ensure initial su-pervision and support
for the patient and caregiver. The home care nurse assesses the patient’s
status and progress and evaluates the techniques that are used in administering
the tube feeding. Further instruction and supervision in the home setting may
be required to help the patient and caregiver adapt to a physical environment
and equipment that are different from the hospital setting. The nurse also
reviews with the patient and caregiver information about com-plications to
report (eg, dumping syndrome, nausea and vomiting, infection of the skin at the
insertion site of the tube).
The
home care nurse assists the patient and family in estab-lishing as normal a
routine as possible. Some patients will want to experience a sensation of
normal eating and are advised that they can try smelling, tasting, and chewing
small amounts of food before taking their tube feedings. This stimulates the
flow of sali-vary and gastric secretions and may give some sensation of a
nor-mal meal. The chewed food can then be deposited by the patient into a
funnel or syringe attached to the gastrostomy tube for administration into the
stomach. The patient or caregiver is en-couraged to keep a diary to record the
times and amounts of feed-ings and any symptoms that occur. The nurse reviews
the diary during home visits. When the tube is to be replaced, the patient or
caregiver must be taught how to do this.
Evaluation
EXPECTED PATIENT OUTCOMES
Expected
patient outcomes may include the following:
1) Achieves an adequate
intake of nutrients
a.
Tolerates quantity and frequency of tube feedings
b. Has 50 mL or less of
residual gastric content before each feeding
c.
Has no diarrhea
d.
Maintains or gains weight
e.
Has normal electrolyte values
2) Is free from infection
and skin breakdown
a.
Is afebrile
b.
Has no drainage from the incision
c.
Demonstrates intact skin surrounding the exit site
d.
Inspects exit site twice a day
3) Adjusts to change in
body image
a.
Is able to discuss expected changes
b.
Verbalizes concerns
c.
Asks to speak with someone who has experienced this
procedure
4) Demonstrates skill in
managing feeding regimen
a.
Helps prepare prescribed formula or blenderized
food
b.
Handles equipment competently
c.
Helps administer the feeding or does so
independently
d.
Demonstrates how to maintain tube patency
e.
Cleans tubing as needed
f.
Keeps an accurate record of intake
g.
Can remove and reinsert the tube as appropriate and
needed for feedings
5) Avoids complications
a.
Exhibits adequate wound healing
b.
Has no abnormal bleeding from puncture site
c.
Tube remains intact for the duration of therapy
Related Topics