Chapter: Medical Surgical Nursing: Gastrointestinal Intubation and Special Nutritional Modalities
Tube Feedings With Nasogastric and Nasoenteric Devices
Tube Feedings With Nasogastric and
Nasoenteric Devices
Tube feedings are given to meet nutritional
requirements when oral intake is inadequate or not possible and the GI tract is
func-tioning normally. Tube feedings have several advantages over par-enteral
nutrition: they are low in cost, safe, well tolerated by the patient, and easy
to use both in extended care facilities and in the patient’s home. Tube
feedings have other advantages:
•
They preserve GI integrity by delivery of nutrients
and medications (antacids, simethicone, and metoclopramide) intraluminally
•
They preserve the normal sequence of intestinal and
hepatic metabolism
•
They maintain fat metabolism and lipoprotein
synthesis
•
They maintain normal insulin/glucagon ratios
Tube
feedings are delivered to the stomach (in the case of NG intubation or
gastrostomy) or to the distal duodenum or proximal jejunum (in the case of
nasoduodenal or nasojejunaltube feeding).
Nasoduodenal or nasojejunal feeding is indicatedwhen the esophagus and stomach
need to be bypassed or when the patient is at risk for aspiration (breathing fluids or foods into the trachea and lungs).
For long-term feedings (longer than 4 weeks), nasoduodenal, gastrostomy, or
jejunostomy tubes are preferred for administration of medications or food. The
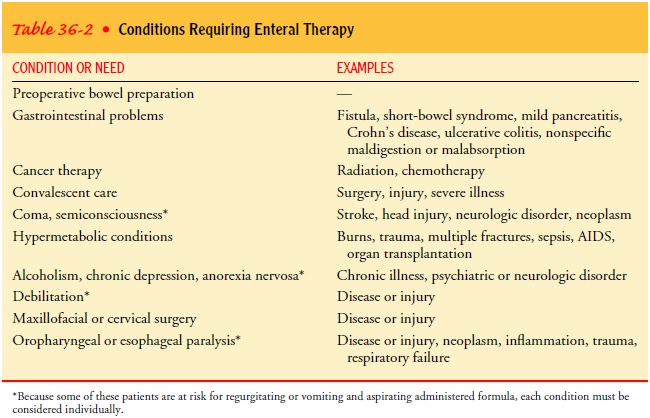
nu-merous conditions requiring enteral nutrition are summarized in Table 36-2.
OSMOSIS AND OSMOLALITY
Osmolality
is an important consideration for patients receiving tube feedings through the
duodenum or jejunum, because feed-ing formulas with a high osmolality may lead
to undesirable ef-fects, such as dumping syndrome (described below).
Fluid
balance is maintained by osmosis,
the process by which water moves through membranes from a dilute solution of
lower osmolality (ionic
concentration) to a more concentrated solutionof higher osmolality until both
solutions are of nearly equal os-molality. The osmolality of normal body fluids
is approximately 300 mOsm/kg. The body attempts to keep the osmolality of the
contents of the stomach and intestines at approximately this level.
Highly
concentrated solutions and certain foods can upset the normal fluid balance in
the body. Individual amino acids and carbohydrates are small particles that
have great osmotic effect. Proteins are extremely large particles and therefore
have less os-motic effect. Fats are not water-soluble and do not enter into a
solution in water; thus, they have no osmotic effect. Electrolytes, such as
sodium and potassium, are comparatively small particles; they have a great
effect on osmolality and consequently on the pa-tient’s ability to tolerate a
given solution.
When a
concentrated solution of high osmolality is taken in large amounts, water will
move to the stomach and intestines from fluid surrounding the organs and the
vascular compartment. The patient has a feeling of fullness, nausea, and
diarrhea; this causes dehydration, hypotension, and tachycardia, collectively
termed the dumping syndrome.
Starting with a more dilute solution and increasing the concentration over
several days can generally alleviate this problem. Patients vary in the degree
to which they tolerate the effects of high osmolality; usually debilitated
patients are more sensitive. The nurse needs to be knowledgeable about the
osmolality of the patient’s formula and needs to observe for and take steps to
prevent undesired effects.
TUBE FEEDING FORMULAS
The choice of formula to be delivered by tube feeding is influ-enced by the status of the GI tract and the nutritional needs of the patient. The formula characteristics evaluated include chem-ical composition of the nutrient source (protein, carbohydrates, fat), caloric density, osmolality, residue, bacteriologic safety, vita-mins, minerals, and cost.
Various
major formula types for tube feedings are available commercially. Blenderized
formulas can be made by the patient’s family or obtained in a ready-to-use form
that is carefully prepared according to directions. Commercially prepared
polymeric for-mulas (formulas with high molecular weight) are composed of
protein, carbohydrates, and fats in a high-molecular-weight form (Boost Plus,
TwoCal HN, Isosource). Chemically defined for-mulas contain predigested and
easy-to-absorb nutrients (Osmo-lite HN). Modular products contain only one
major nutrient, such as protein (Promote). Disease-specific formulas are available
for various conditions, such as renal failure (Nepro), severe chronic
obstructive pulmonary disease (Pulmocare). Nepro is high in calories and low in
electrolytes. It is ideal for patients who re-quire electrolyte and fluid
restriction. Pulmocare is high in fat and low in carbohydrates. Its high
density (1.5 calories/mL) is ideal for patients who require fluid restriction,
and it is also de-signed to reduce carbon dioxide production. Fiber has also
been added to formulas (Jevity) in an attempt to decrease the occur-rence of
diarrhea. Some feedings are given as supplements, and others are designed to
meet the patient’s total nutritional needs. Dietitians collaborate with
physicians and nurses in determining the best formula for the individual patient.
TUBE FEEDING ADMINISTRATION METHODS
Many
patients do not tolerate NG and nasoenteric tube feedings well. Often a medium-
or fine-bore Silastic nasoenteric tube is tolerated better than a plastic or
rubber tube. The finer-bore tube requires a finely dispersed formula to ensure
that the patency of the tube is maintained. For long-term tube feeding therapy,
a gas-trostomy or jejunostomy tube is used (see later discussion).
The
tube feeding method chosen depends on the location of the tube, patient
tolerance, convenience, and cost. Intermittent bolus feedings are administered
into the stomach (usually by gas-trostomy tube) in large amounts at designated
intervals and may be given 4 to 8 times per day. The intermittent gravity drip
is another method for administering tube feedings into the stomach and is
commonly used when the patient is at home. In this in-stance, the tube feeding
is administered over 30 minutes at desig-nated intervals. Both of these
tube-feeding methods are practical and inexpensive. However, the feedings
delivered at variable rates may be poorly tolerated and time-consuming.
The
continuous infusion method is used when feedings are administered into the
small intestine. This method is preferred for patients who are at risk for
aspiration or who tolerate the tube feedings poorly. The feedings are given
continuously at a con-stant rate by means of a pump. The continuous tube
feeding method, which requires a pump device, decreases abdominal distention,
gastric residuals, and the risk of aspiration. However, pumps are expensive,
and they permit the patient less flexibility than intermittent feedings do.
An
alternative to the continuous infusion method is cyclicfeeding. The infusion is given at a faster rate over a
shorter time(usually 8 to 12 hours). Feeding may be infused at night to avoid
interrupting the patient’s lifestyle. Cyclic continuous infusions may be
appropriate for patients who are being weaned from tube feedings to an oral
diet, as a supplement for a patient who cannot eat enough, and for patients at
home who need daytime hours free from the pump.
Tube
feeding solutions vary in terms of required preparation, consistency, and the
number of calories and supplemental vita-mins they contain. The choice of
solution depends on the size and location of the tube, the patient’s nutrient
needs, the type of nu-tritional supplement, the method of delivery, and the
convenience for the patient at home. A wide variety of containers, feeding
tubes and catheters, delivery systems, and pumps are available for use with
tube feedings.
Related Topics