Chapter: Medical Surgical Nursing: Management of Patients With Gastric and Duodenal Disorders
Nursing Process: The Patient With Gastric Cancer
NURSING
PROCESS:THE PATIENT WITH GASTRIC CANCER
Assessment
The
nurse elicits a dietary history from the patient, focusing on recent
nutritional intake and status. Has the patient lost weight? If so, how much and
over what period of time? Can the patient tolerate a full diet? If not, what
foods can he or she eat? What other changes in eating habits have occurred?
Does the patient have an appetite? Is the patient in pain? Do foods, antacids,
or medications relieve the pain, make no difference, or worsen the pain? Is
there a history of infection with H.
pylori bacteria? Other health information to obtain includes the patient’s
smoking and alcohol history and the family history (any first- or second-degree
relatives with gastric or other cancer). A psychosocial assessment, including
questions about social support, individual and family coping skills, and
financial resources, will help the nurse plan for care in acute and community
settings.
After
the interview, the nurse performs a complete physical ex-amination, carefully
assesses the patient’s abdomen for tenderness or masses, and also palpates and
percusses to detect ascites.
Nursing Diagnosis
Based
on the assessment data, the patient’s major nursing diag-noses may include the
following:
•
Anxiety related to the disease and anticipated treatment
•
Imbalanced nutrition, less than body requirements,
related to anorexia
•
Pain related to tumor mass
•
Anticipatory grieving related to the diagnosis of
cancer
•
Deficient knowledge regarding self-care activities
Planning and Goals
The
major goals for the patient may include reduced anxiety, op-timal nutrition,
relief of pain, and adjustment to the diagnosis and anticipated lifestyle
changes.
Nursing Interventions
REDUCING ANXIETY
A
relaxed, nonthreatening atmosphere is provided so that patient can express
fears, concerns, and possibly anger about the diagno-sis and prognosis. The
nurse encourages the family in their efforts to support the patient, offering
reassurance and supporting pos-itive coping measures. The nurse advises the
patient about any procedures and treatments so that the patient knows what to
ex-pect. The nurse also may suggest talking with a support person (eg,
spiritual advisor), if the patient desires.
PROMOTING OPTIMAL NUTRITION
The
nurse encourages the patient to eat small, frequent portions of nonirritating
foods to decrease gastric irritation. Food supplements should be high in
calories, as well as vitamins A and C and iron, to enhance tissue repair. If
the patient is unable to eat adequately to meet nutritional requirements,
parenteral nutrition may be neces-sary. Because the patient may develop dumping
syndrome when enteral feeding resumes after gastric resection, the nurse
explains ways to prevent and manage it (six small feedings daily that are low
in carbohydrates and sugar; fluids between meals rather than with meals) and
informs the patient that symptoms often resolve after several months. If a
total gastrectomy is performed, parenteral vitamin B12 will be required
indefinitely, because dietary vitamin B12 is absorbed in the stomach. The nurse
monitors the IV therapy and nutritional status and records intake, output, and
daily weights to ensure that the patient is maintaining or gaining weight. The
nurse assesses for signs of dehydration (thirst, dry mucous mem-branes, poor
skin turgor, tachycardia, decreased urine output) and reviews the results of
daily laboratory studies to note any metabolic abnormalities (sodium,
potassium, glucose, blood urea nitrogen). Antiemetics are administered as
prescribed.
RELIEVING PAIN
The
nurse administers analgesics as prescribed. A continuous in-fusion of an opioid
may be necessary for severe pain. The nurse assesses the frequency, intensity,
and duration of the pain to de-termine the effectiveness of the analgesic being
administered. The nurse works with the patient to manage pain by suggesting
non-pharmacologic methods for pain relief, such as position changes, imagery,
distraction, relaxation exercises (using relaxation audio-tapes), backrubs,
massage, and periods of rest and relaxation.
PROVIDING PSYCHOSOCIAL SUPPORT
The
nurse helps the patient express fears, concerns, and grief about the diagnosis.
It is important to answer the patient’s questions hon-estly and to encourage
the patient to participate in treatment deci-sions. Some patients mourn the
loss of a body part and perceive their surgery as a type of mutilation. Some
express disbelief and need time and support to accept the diagnosis.
The
nurse offers emotional support and involves family mem-bers and significant
others whenever possible. This includes rec-ognizing mood swings and defense
mechanisms (eg, denial, rationalization, displacement, regression) and
reassuring the pa-tient and family members that emotional responses are normal
and expected. The services of clergy, psychiatric clinical nurse specialists,
psychologists, social workers, and psychiatrists are made available, if needed.
The nurse projects an empathetic at-titude and spends time with the patient.
Most patients will begin to participate in self-care activities after they have
acknowledged their loss.
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care
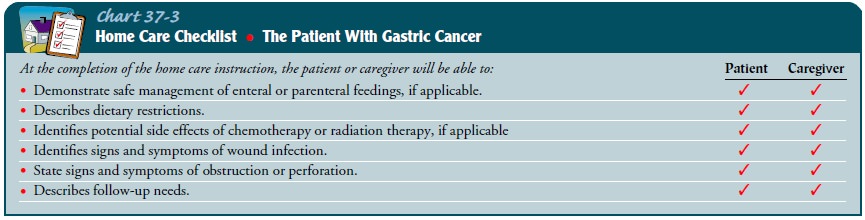
Self-care
activities will depend on the mode of treatment used— surgery, chemotherapy,
radiation, or palliative care. Patient and family teaching will include
information about diet and nutri-tion, treatment regimens, activity and
lifestyle changes, pain management, and possible complications (Chart 37-3).
Consul tation with a dietitian is essential to determine how the patient’s
nutritional needs can best be met at home. The nurse teaches the patient or
care provider about administration of enteral or pa-renteral nutrition. If
chemotherapy or radiation is prescribed, the nurse provides explanations to the
patient and family about what to expect, including the length of treatments,
the expected side effects (eg, nausea, vomiting, anorexia, fatigue,
neutropenia), and the need for transportation to appointments for treatment.
Psy-chological counseling may also be helpful.
Continuing Care
The
need for ongoing care in the home will depend on the patient’s condition and
treatment. The home care nurse reinforces nutri-tional counseling and
supervises the administration of any enteral or parenteral feedings; the
patient or family member must become skillful in administering the feedings and
in detecting and pre-venting untoward effects or complications related to the
feedings. The nurse teaches the patient or a family member to record the
patient’s daily intake, output, and weight and explains strategies to manage
pain, nausea, vomiting, or other symptoms. The nurse also teaches the patient
or caregiver to recognize and report signs and symptoms of complications that
require medical attention, such as bleeding, obstruction, perforation, or any
symp-toms that become progressively worse. It is important to explain the
chemotherapy or radiation therapy regimen. The patient and family need to know
about the care that will be needed during and after treatments. Because the
prognosis for gastric cancer is so poor, the nurse may need to assist the
patient and family with decisions regarding end-of-life care. Referral to
hospice may be warranted.
Evaluation
EXPECTED PATIENT OUTCOMES
Expected
patient outcomes may include the following:
1) Reports less anxiety
a.
Expresses fears and concerns about surgery
b.
Seeks emotional support
2) Attains optimal
nutrition
a.
Eats small, frequent meals high in calories, iron,
and vitamins A and C
b.
Complies with enteral or parenteral nutrition as
needed
3) Has less pain
4) Performs self-care
activities and adjusts to lifestyle changes
a.
Resumes normal activities within 3 months
b.
Alternates periods of rest and activity
c. Manages tube feedings
Related Topics