Chapter: Medical Surgical Nursing: Management of Patients With Gastric and Duodenal Disorders
Gastric and Duodenal Ulcers
Gastric and Duodenal Ulcers
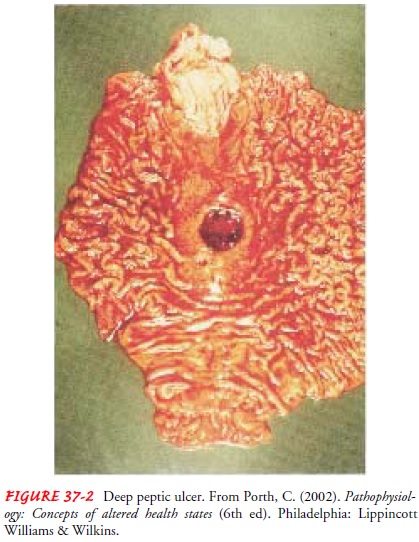
A peptic ulcer is an excavation (hollowed-out area) that forms in the
mucosal wall of the stomach, in the pylorus (opening between stomach and
duodenum), in the duodenum (first part of small intestine), or in the
esophagus. A peptic ulcer is frequently referred to as a gastric, duodenal, or
esophageal ulcer, depending on its location, or as peptic ulcer disease.
Erosion of a circumscribed area of mucous membrane is the cause (Fig. 37-2).
This erosion may extend as deeply as the muscle layers or through the muscle to
the peritoneum. Peptic ulcers are more likely to be in the duodenum than in the
stomach. As a rule they occur alone, but they may occur in multiples. Chronic
gastric ulcers tend to occur in the lesser curvature of the stomach, near the
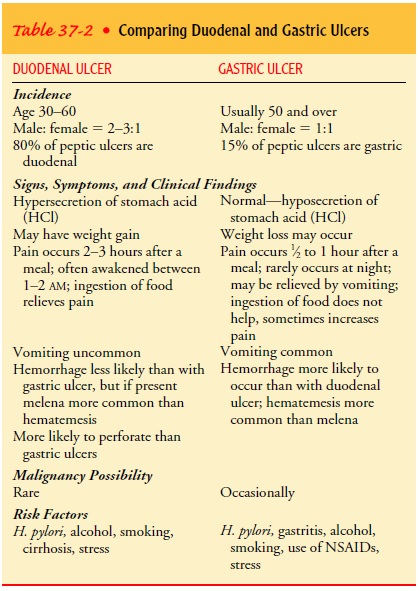
pylorus. Table 37-2 compares the features of gastric and duodenal ulcers.
Peptic ulcer disease occurs with the greatest frequency in people between the ages of 40 and 60 years. It is relatively uncommon in women of childbearing age, but it has been observed in children and even in infants. After menopause, the incidence of peptic ulcers in women is almost equal to that in men. Peptic ulcers in the body of the stomach can occur without excessive acid secretion.
In the past, stress and anxiety were thought to be causes of ulcers.
Research has identified that peptic ulcers result from infection with the
gram-negative bacteria H. pylori (Tytgat, 2000). However, ulcers do seem to
develop more commonly in people who are tense; whether this is a contributing
factor to the condition is uncertain. In addition, excessive secretion of HCl
in the stomach may contribute to the formation of gastric ulcers, and stress
may be associated with its increased secretion.
The ingestion of milk and caffeinated beverages, smoking, and alcohol
also may increase HCl secretion.Familial tendency may be a significant
predisposing factor. A further genetic link is noted in the finding that people
with blood type O are more susceptible to peptic ulcers than are those with
blood type A, B, or AB. There also is an association between duodenal ulcers
and chronic pulmonary disease or chronic renal disease. Other predisposing
factors associated with peptic ulcer include chronic use of NSAIDs, alcohol
ingestion, and excessive smoking.
Rarely, ulcers are caused by excessive amounts of the hormone gastrin,
produced by tumors. This Zollinger-Ellison syndrome (ZES) consists of severe
peptic ulcers, extreme gastric hyperacidity, and gastrin-secreting benign or
malignant tumors of the pancreas. Stress ulcers, which are clinically different
from peptic ulcers, are ulcerations in the mucosa that can occur in the
gastroduodenal area. Stress ulcers may occur in patients who are exposed to
stressful conditions. Esophageal ulcers occur as a result of the backward flow
of HCl from the stomach into the esophagus (gastroesophageal reflux disease
[GERD]).
Pathophysiology
Peptic
ulcers occur mainly in the gastroduodenal mucosa because this tissue cannot
withstand the digestive action of gastric acid (HCl) and pepsin. The erosion is
caused by the increased concen-tration or activity of acid-pepsin, or by
decreased resistance of the mucosa. A damaged mucosa cannot secrete enough
mucus to act as a barrier against HCl. The use of NSAIDs inhibits the secretion
of mucus that protects the mucosa. Patients with duodenal ulcer disease secrete
more acid than normal, whereas patients with gas-tric ulcer tend to secrete
normal or decreased levels of acid.
ZES is
suspected when a patient has several peptic ulcers or an ulcer that is
resistant to standard medical therapy. It is identified by the following
findings: hypersecretion of gastric juice, duode-nal ulcers, and gastrinomas
(islet cell tumors) in the pancreas. Ninety percent of tumors are found in the
“gastric triangle,” which encompasses the cystic and common bile ducts, the
second and third portions of the duodenum, and the neck and body of the
pancreas. Approximately one third of gastrinomas are malig-nant. Diarrhea and
steatorrhea (unabsorbed fat in the stool) may be evident. The patient may have
coexisting parathyroid adeno-mas or hyperplasia and may therefore exhibit signs
of hyper-calcemia. The most common complaint is epigastric pain. H. pylori is not a risk factor for ZES.
Stress ulcer is the term given to the acute mucosal
ulceration ofthe duodenal or gastric area that occurs after physiologically
stress-ful events, such as burns, shock, severe sepsis, and multiple organ
traumas. These ulcers are most common in ventilator-dependent patients after
trauma or surgery. Fiberoptic endoscopy within 24 hours after injury reveals
shallow erosions of the stomach wall; by 72 hours, multiple gastric erosions
are observed. As the stress-ful condition continues, the ulcers spread. When
the patient re-covers, the lesions are reversed. This pattern is typical of
stress ulceration.
Differences
of opinion exist as to the actual cause of mucosal ulceration in stress ulcers.
Usually, it is preceded by shock; this leads to decreased gastric mucosal blood
flow and to reflux of duodenal contents into the stomach. In addition, large
quantities of pepsin are released. The combination of ischemia, acid, and
pepsin creates an ideal climate for ulceration.
Stress
ulcers should be distinguished from Cushing’s ulcers and Curling’s ulcers, two
other types of gastric ulcers. Cushing’s ulcers are common in patients with
trauma to the brain. They may occur in the esophagus, stomach, or duodenum and
are usu-ally deeper and more penetrating than stress ulcers. Curling’s ulcer is
frequently observed about 72 hours after extensive burns and involves the
antrum of the stomach or the duodenum.
Clinical Manifestations
Symptoms
of an ulcer may last for a few days, weeks, or months and may disappear only to
reappear, often without an identifiable cause. Many people have symptomless
ulcers, and in 20% to 30% perforation or hemorrhage may occur without any
preceding manifestations.
As a
rule, the patient with an ulcer complains of dull, gnaw-ing pain or a burning
sensation in the midepigastrium or in the back. It is believed that the pain
occurs when the increased acid content of the stomach and duodenum erodes the
lesion and stimulates the exposed nerve endings. Another theory suggests that
contact of the lesion with acid stimulates a local reflex mech-anism that
initiates contraction of the adjacent smooth muscle. Pain is usually relieved
by eating, because food neutralizes the acid, or by taking alkali; however,
once the stomach has emptied or the alkali’s effect has decreased, the pain
returns. Sharply local-ized tenderness can be elicited by applying gentle
pressure to the epigastrium at or slightly to the right of the midline.
Other
symptoms include pyrosis
(heartburn), vomiting, con-stipation or diarrhea, and bleeding. Pyrosis is a
burning sensation in the esophagus and stomach that moves up to the mouth.
Heartburn is often accompanied by sour eructation, or burping, which is common
when the patient’s stomach is empty.
Although
vomiting is rare in uncomplicated duodenal ulcer, it may be a symptom of a
peptic ulcer complication. It results from obstruction of the pyloric orifice,
caused by either muscu-lar spasm of the pylorus or mechanical obstruction from
scarring or acute swelling of the inflamed mucous membrane adjacent to the
ulcer. Vomiting may or may not be preceded by nausea; usu-ally it follows a
bout of severe pain and bloating, which is relieved by ejection of the gastric
contents. Emesis often contains un-digested food eaten many hours earlier.
Constipation or diarrhea can occur, probably as a result of diet and
medications.
Fifteen
percent of patients with gastric ulcers experience bleed-ing. Patients may
present with GI bleeding as evidenced by the passage of tarry stools. A small
portion of patients who bleed from an acute ulcer have had no previous
digestive complaints, but they develop symptoms thereafter (Yamada, 1999).
Assessment and Diagnostic Findings
A
physical examination may reveal pain, epigastric tenderness, or abdominal
distention. A barium study of the upper GI tract may show an ulcer; however,
endoscopy is the preferred diagnostic procedure because it allows direct
visualization of inflammatory changes, ulcers, and lesions. Through endoscopy,
a biopsy of the gastric mucosa and of any suspicious lesions can be obtained.
En-doscopy may reveal lesions that are not evident on x-ray studies because of
their size or location.
Stools
may be tested periodically until they are negative for oc-cult blood. Gastric
secretory studies are of value in diagnosing achlorhydria and ZES. H. pylori infection may be determined by
biopsy and histology with culture. There is also a breath test that detects H. pylori, as well as a serologic test
for antibodies to the H. pylori antigen.
Pain that is relieved by ingesting food orantacids and absence of pain on
arising are also highly suggestive of an ulcer.
Medical Management
Once
the diagnosis is established, the patient is informed that the problem can be
controlled. Recurrence may develop; however, peptic ulcers treated with
antibiotics to eradicate H. pylori
have a lower recurrence rate than those not treated with antibiotics. The goals
are to eradicate H. pylori and to
manage gastric acidity. Methods used include medications, lifestyle changes,
and surgical intervention.
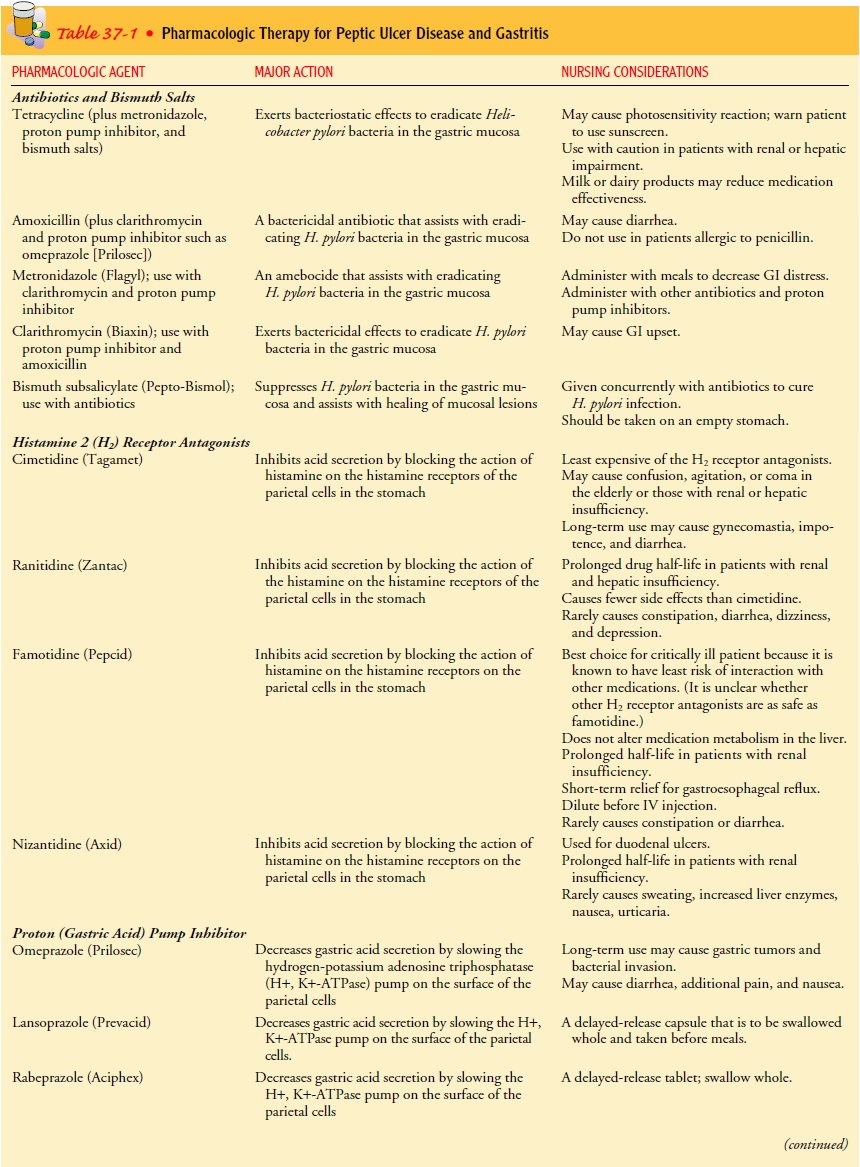
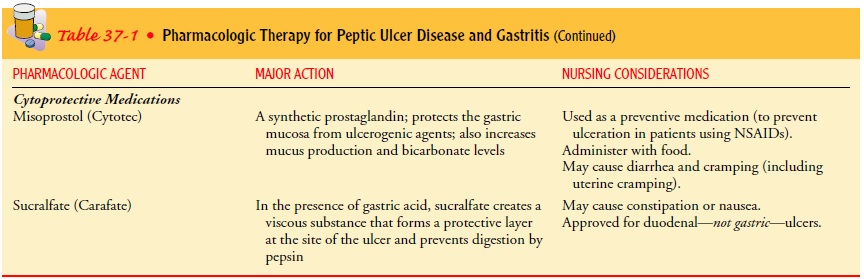
PHARMACOLOGIC THERAPY
Currently,
the most commonly used therapy in the treatment of ulcers is a combination of
antibiotics, proton pump inhibitors, and bismuth salts that suppresses or
eradicates H. pylori; hista-mine 2 (H2) receptor antagonists
and proton pump inhibitors are used to treat NSAID-induced and other ulcers not
associated with H. pylori ulcers.
Table 37-1 provides details about pharma-cologic treatment.
The
patient is advised to adhere to the medication regimen to ensure complete
healing of the ulcer. Because most patients be-come symptom-free within a week,
it becomes a nursing responsi-bility to stress the importance of following the
prescribed regimen so that the healing process can continue uninterrupted and
the re-turn of chronic ulcer symptoms can be prevented. Rest, sedatives, and
tranquilizers may add to the patient’s comfort and are pre-scribed as needed.
Maintenance dosages of H2 receptor antagonists are usually recommended for 1
year.
For
patients with ZES, hypersecretion of acid may be con-trolled with high doses of
H2 receptor antagonists.
These patients may require twice the normal dose, and dosages usually need to
be increased with prolonged use. Octreotide (Sandostatin), a med-ication that
suppresses gastrin levels, also may be prescribed.
Patients
at risk for stress ulcers may be treated prophylacti-cally with IV H2 receptor antagonists
and cytoprotective agents (e.g., misoprostol, sucralfate) because of the risk
for upper GI tract hemorrhage. Frequent gastric aspiration is performed to
allow monitoring of gastric secretion pH.
STRESS REDUCTION AND REST
Reducing
environmental stress requires physical and psychologi-cal modifications on the
patient’s part as well as the aid and coop-eration of family members and
significant others. The patient may need help in identifying situations that
are stressful or exhausting. A rushed lifestyle and an irregular schedule may
aggravate symp-toms and interfere with regular meals taken in relaxed settings
and with the regular administration of medications. The patient may benefit
from regular rest periods during the day, at least during the acute phase of
the disease. Biofeedback, hypnosis, or behavior modification may be helpful.
SMOKING CESSATION
Studies
have shown that smoking decreases the secretion of bicar-bonate from the
pancreas into the duodenum, resulting in increased acidity of the duodenum.
Research indicates that continuing to smoke cigarettes may significantly
inhibit ulcer repair. Therefore, the patient is strongly encouraged to stop
smoking. Smoking cessa-tion support groups and other smoking cessation
approaches are helpful for many patients (Eastwood, 1997).
DIETARY MODIFICATION
The
intent of dietary modification for patients with peptic ulcers is to avoid
oversecretion of acid and hypermotility in the GI tract. These can be minimized
by avoiding extremes of temperature and overstimulation from consumption of
meat extracts, alcohol, coffee (including decaffeinated coffee, which also
stimulates acid secretion) and other caffeinated beverages, and diets rich in
milk and cream (which stimulate acid secretion). In addition, an effort is made
to neutralize acid by eating three regular meals a day. Small, frequent
feedings are not necessary as long as an antacid or a histamine blocker is
taken. Diet compatibility becomes an in-dividual matter: the patient eats foods
that can be tolerated and avoids those that produce pain.
SURGICAL MANAGEMENT
The
introduction of antibiotics to eradicate H.
pylori and of H2 receptor antagonists as treatment for ulcers has
greatly reduced the need for surgical interventions. However, surgery is usually
recom-mended for patients with intractable ulcers (those that fail to heal
after 12 to 16 weeks of medical treatment), life-threatening hem-orrhage,
perforation, or obstruction, and for those with ZES not re-sponding to
medications (Yamada, 1999). Surgical procedures include
vagotomy, with or without pyloroplasty, and the Billroth I and Billroth II
procedures. Patients who need ulcer surgery may have had a long illness. They
may be discouraged and have had interruptions in their work role and pressures
in their family life.
FOLLOW-UP CARE
Recurrence
within 1 year may be prevented with the prophylac-tic use of H2 receptor antagonists
given at a reduced dose. Not all patients require maintenance therapy; it may
be prescribed only for those with two or three recurrences per year, those who
have had a complication such as bleeding or outlet obstruction, or those who
are candidates for gastric surgery but are at too high a risk for surgery. The
likelihood of recurrence is reduced if the pa-tient avoids smoking, coffee
(including decaffeinated coffee) and other caffeinated beverages, alcohol, and
ulcerogenic medications (eg, NSAIDs).
Related Topics