Chapter: The Massage Connection ANATOMY AND PHYSIOLOGY : Introduction to Anatomy and Physiology
Connective Tissue
Connective Tissue
Structure
Connective tissue is the most abundant of all tissue, forming a continuous network thoughout the body. If all other tissue was removed, connective tissue would form the three-dimensional framework of the body, much like cellulose in plants. Connective tissue, such as bone, blood and fat, appear to be different from each other, but they have some common features that place them under this classification. All connective tissue have three characteristics—they have special-ized cells; protein fibers that are present outside the cells; and a fluid known as ground substance, in which the fibers and cells are suspended. The fibers and the ground substance combined are referred to as the matrix that surrounds the cells.
Unlike epithelia, the cells in connective tissue are scattered. Connective tissue is not exposed to the ex-terior and most connective tissue is vascularized (i.e., they have a good supply of blood vessels). Many types of connective tissue have nerve endings that respond to various sensations, such as touch, pressure, pain, and temperature changes.
Function
Connective tissue has many functions. It forms the structural framework for the body and helps support, surround, and interconnect various organs and tis-sues. It also helps transport fluid and substances from one region to the other (e.g., blood). Certain connective tissue protects the organs and certain tis-sue has special cells scattered in them that help kill invading organisms. Connective tissue may serve as a storage sites for nutrients (e.g., fat).
Classification
Connective tissue may be classified as connectivetissue proper, fluid connective tissue, and sup-porting connective tissue. The three types differ inthe type of cells, fibers, and ground substance. The proportions also vary, altering the consistency.
Connective Tissue Proper
This type of connective tissue (see Figure 1.23) has many different types of cells suspended in the matrix. The properties and proportions of fibers also vary.
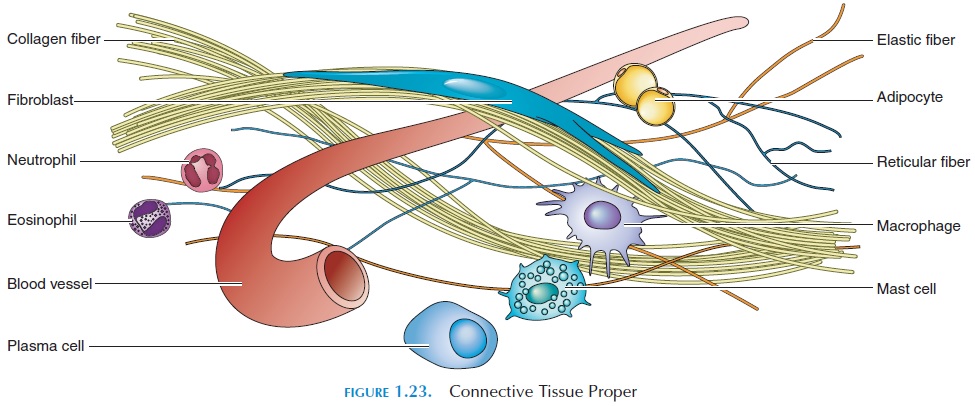
Cells
Connective tissue proper has cells that help with repair, healing, and storage, as well as other cells that help with defense. Fibroblasts and mesenchymal cells re-pair injured tissue; adipocytes store fat. Other cells in connective tissue proper that have the capability of mi-grating to injured areas are macrophages, mi-crophages, mast cells, lymphocytes, and platelets.
Fibroblasts
Fibroblasts are the most abundant cells. They secrete a polysaccharide known as hyaluronic acid and pro-teins into the ground substance, which gives connec-tive tissue its thick consistency. Fibroblasts also se-crete proteins that interact and form the protein fibers in the ground substance that is responsible for the strength, flexibility, and elasticity of connective tissue.
Mesenchymal Cells
Mesenchymal cells are the mother cells that differen-tiate into fibroblasts and other cells when there is in-jury.
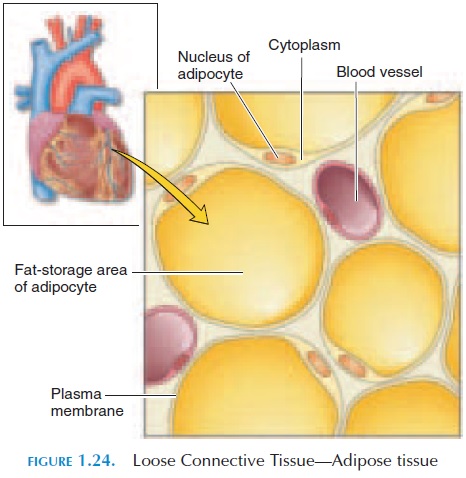
Adipocytes
Adipocytes (see Figure 1.24) are fat cells in which the cytoplasm is filled with a huge, fat droplet. The num-ber of adipocytes varies from region to region and from one person to another.
Macrophages
Macrophages are defense cells that have wandered into the connective tissue from the blood. Scavenger cells, they remove dead cells and foreign agents. Cer-tain macrophages may be fixed to a site (fixedmacrophages), as found in the liver and spleen. Oth-ers are wanderers, attracted to injured areas by chemicals liberated by injured tissue. These are the free macrophages.
Microphages
Microphages are other types of white blood cells (neutrophils and eosinophils) that are attracted to sites of injury and inflammation. They, too, help with defense.
Mast cells
Mast cells are small, connective tissue cells usually found near blood vessels. Mast cell cytoplasm con-tains the chemicals histamine and heparin. When in-jury occurs or when stimulated by allergic sub-stances, mast cells liberate chemicals into the surrounding tissue, producing the typical reactions observed in inflammation.
Lymphocytes
Lymphocytes are white blood cells that wander in tis-sue and function as defense cells.
Platelets
Platelets are the smallest cells present in the blood; they help stop bleeding at the time of injury.
Connective Tissue Fibers
Connective tissue has three different types of fibers, which vary in proportion. The fibers may be colla-gen fibers, reticular fibers, or elastic fibers. Theproportion of different fibers in the ground sub-stance is responsible for the different texture and property.
Collagen Fibers
Collagen fibers are the most common type. They are long, straight, and unbranched. They are made up of protein strands tightly wound together like rope and held together by hydrogen bonds, giving connective tis-sue flexibility. Collagen, however, is strong and can withstand a lot of force if applied from both ends. Ten-dons and ligaments, which withstand a lot of force as muscle contracts, are made up almost entirely of colla-gen. The flexibility of collagen also allows joints to move as the tendons and ligaments go across them.
Collagen fibers can be arranged in different ways to alter the property of the tissue, dictated by the ground substance and the local tissue. They may be arranged randomly, forming sheets (e.g., fascia); systematically stacked (e.g., aponeurosis); spun loosely (e.g., subcu-taneous tissue); or arranged in parallel (e.g., tendon).
Reticular Fibers
Reticular fibers are also proteins, but they are much thinner, forming branching networks. This gives the connective tissue flexibility. At the same time, these fibers are tough and can resist force applied in differ-ent directions. Because of these properties, reticular fibers are more abundant in areas where cells and or-gans must be kept together. Reticular fibers hold blood vessels and nerves in place.
Elastic Fibers
Elastic fibers are branched, wavy fibers containing the protein elastin. The special characteristic of elastin is that it can be stretched and it will return to its original size when released.
Ground Substance
The ground substance is the medium in which the cells and protein fibers are suspended. Usually clear and colorless, it has the consistency of thick syrup. Proteoglycan, which gives ground substance its vis-cous property, is formed by the interaction of poly-saccharides and proteins secreted by fibroblasts into the extracellular fluid.
Substances moving in and out of cells have to pass through the ground substance before they enter blood vessels. The consistency of ground substance varies from region to region. In tissue where mobility is required, the major component of ground sub-stance is hyaluronic acid. In tissues where support is the major function, chondroitin sulfate is the major component.
Depending on how loose or dense they appear, connective tissue proper can be classified as looseconnective tissue or dense connective tissue.
Loose connective tissue has more ground sub-stance and less protein fibers and cells. It is the “pack-ing material” that fills the space between organs, pro-viding support and absorbing shock. For example, it is the presence of loose connective tissue that keeps the skin in place. At the same time, it allows the skin to be pinched up and separated to some extent from the un-derlying tissue. Along with the adipose tissue, this layer of loose connective tissue present under the skin forms the subcutaneous layer or the superficial fas-cia. Adipose tissue is a special type of loose connectivetissue (see Figure 1.24). It acts as a shock absorber and insulator to slowdown loss of heat.
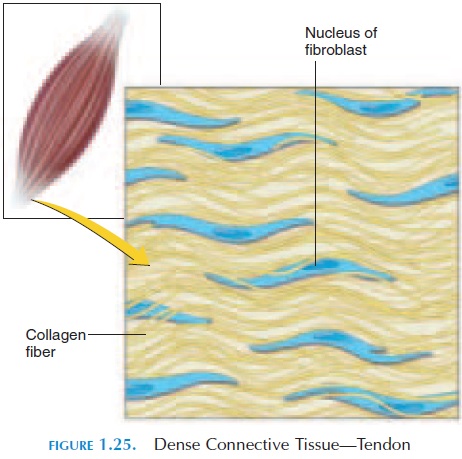
Dense connective tissue has much more proteinfiber—predominantly collagen—than loose connective tissue. The collagen fibers may be arranged regularly or irregularly, giving the tissue variable flexibility and strength. Dense connective tissue has a shiny, white appearance. Tendons, ligaments, aponeurosis, the cap-sule of joints, the outer layer of bones (periosteum), the outer layer of cartilage (perichondrium), are all ex-amples of this type of tissue (see Figure 1.25).
Fluid Connective Tissue
Blood and lymph are examples of fluid connective tis-sue. The liquid matrix of blood is the plasma. Blood cells are suspended in the plasma. Proteins, nutrients, waste products, hormones, and electrolytes are dis-solved in the plasma. Lymph is the fluid flowing inside lymphatic vessels, varying in composition according to the site they drain. The structure, composition, and function of blood and lymph are described in Chap-ters XX and XX, respectively.
Supporting Connective Tissue
Supporting connective tissue provides a strong, solid framework; cartilage and bone are typical examples. Strength is provided by the presence of numerous fibers in the ground substance. In bone, in addition to the fibers, insoluble calcium salts are deposited in the ground substance.
Cartilage
Cartilage matrix (see Figure 1.26) is made up of a special polysaccharide known as chondroitin sul-fate, which interacts with the proteins in the groundsubstance to formproteoglycans. Cartilage cells known as chondrocytes are found in the matrix. These cells are located in cavities known as lacunae. Unlike other connective tissue, cartilage does not have blood vessels and must rely on diffusion of nu-trients from surrounding areas.
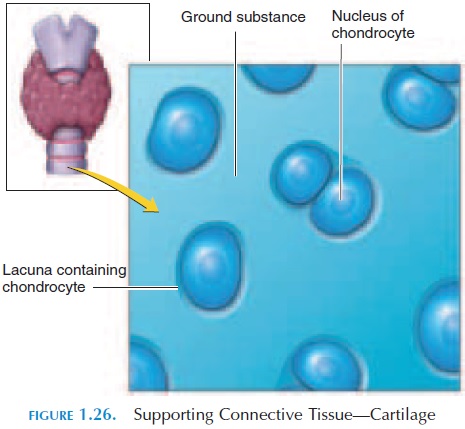
The property of cartilage depends on the type and proportion of protein fibers scattered in the matrix. Depending on its property, cartilage may be classified as hyaline cartilage, elastic cartilage, or fibrocar-tilage. Hyaline cartilage has closely packed collagenfibers, making it tough and flexible. The most com-mon cartilage type, it is found in joints covering the ends of the bones. It is also found in the epiphyseal plate (the region where bone growth occurs). Elastic cartilage has more elastic fibers, making the cartilage more “springy.” It is found in regions such as the ex-ternal ear. Fibrocartilage has little ground substance and more collagen fibers, making the cartilage tough, helping it resist compression and absorb shock. It is found in the intervertebral disks (the cartilage be-tween two vertebrae).
Connective Tissue—the Fluid Crystal
From the description of the various types of connective tissue, it can be observed that by varying the propor-tion of the three components—ground substance, pro-tein fibers, and cells—the property of the tissue can be changed significantly. By having a watery ground sub-stance, fluid connective tissue, such as blood, is formed. By introducing more protein fiber, less fluid but tougher tissue is formed.
By altering the propor-tion of collagen, elastic, and reticular fibers, the tissue can be as tough as tendons that withstand more force or flexible (but tough) tissue, such as tissue that covers muscles. With the introduction of specialized proteins and cells, such as chondrocytes, the connective tissue is transformed into solid, flexible cartilage. With the in-troduction of insoluble calcium salts into the ground substance, the tissue becomes rigid—bone.
The remarkable properties of connective tissue make it comparable to fluid crystal—a type of sub-stance that can be transformed from one state to an-other. As it is largely made up of nonliving material, its fluid crystal state can be manipulated to a large ex-tent by application of heat, cold, stretch, and activity.
Connective Tissue Thixotropic Properties
Connective tissue, such as gels, has the property of thixotropy. This phenomenon solidifies substances,such as gelatin, when cold or left undisturbed and liq-uefies substances when warmed or stirred.
Connective tissue, if not stretched and warmed by muscular activity, tends to stiffen and become less flexible. This is one of the reasons why early mobility is emphasized after injury. Stiff, less mobile joints are more common in sedentary individuals.
Massage therapy has a tremendous impact on con-nective tissue. The stretches, strokes, movement, and heat make connective tissue more fluid, allowing greater movement and flow, encouraging better blood flow and speedy removal of pain producing toxins from the area.
Connective Tissue and Adhesive Properties
Unfortunately, with disuse and chronic pressure, the collagen fibers of connective tissue tend to pack to-gether by hydrogen bonding. In areas that are chron-ically stressed, inflamed, or that have not been used for a long time, the connective tissue layers, which separate organs, bind together, preventing easy movement and gliding of the organs over each other. This is known as adhesions. Nerves and blood ves-sels may get caught in these adhesions, causing com-plications. Reduced range of motion, ischemic pain, and loss of sensation and voluntary control are some of the negative outcome of adhesions.
Manipulation helps prevent adhesions in those sit-uations or slow it down. It also helps align the colla-gen fibers in a way to better reduce friction and allow movement.
Membranes
Membranes, which cover and protect other struc-tures, are formed by the combination of epithelia and connective tissue. Four such membranes exist in the body—mucous membrane, serous membrane, cu-taneous membrane, and synovial membrane.
Examples of mucous membrane are the lining of digestive, respiratory, urinary, and reproductive tracts. The epithelium secretes mucous in these re-gions. Serous membrane lines the peritoneal, pleural, and pericardial cavities and secretes a watery fluid. The body’s outer surface is covered by skin, a cuta-neous membrane. The synovial membrane, which se-cretes the synovial fluid, lines all synovial joints.
Related Topics